08 December 2020: Original Paper
Waitlisted Transplant Candidates’ Attitudes and Concerns Toward Transplantation During COVID-19
Ek Khoon Tan12ABCDEF*, Ye Xin Koh12ABE, Terence Kee23ADEF, Juhainah Binte Juhari2ABE, Teing Ee Tan45ADE, David Kheng Leng Sim26ADE, Aloysius Yew Leng Ho26ADE, Lalitha Krishnan2ABE, Ping Sing Tee2ABE, Thinesh Lee Krishnamoorthy27ADEF, Brian Kim Poh Goh12ADE, Ban Hock Tan89ADEF, Shimin Jasmine Chung29ADEF, Ghee Chee Phua210ADE, Prema Raj Jeyaraj112ADEDOI: 10.12659/AOT.926992
Ann Transplant 2020; 25:e926992
Abstract
BACKGROUND: In solid organ transplant (SOT) and hematopoietic stem cell transplant (HSCT) recipients, coronavirus disease 2019 (COVID-19) can contribute to a severe clinical course and an increased risk of death. Thus, patients awaiting a SOT or HSCT face the dilemma of choosing between a life-saving treatment that presents a significant threat of COVID-19 and the risk of waitlist dropout, progression of disease, or mortality. The lack of established literature on COVID-19 complicates the issue as patients, particularly those with inadequate health literacy, may not have the resources needed to navigate these decisions.
MATERIAL AND METHODS: We conducted a standardized phone survey of patients awaiting SOT or HSCT to assess the prevalence of inadequate health literacy and attitudes toward transplant during the COVID-19 pandemic.
RESULTS: Seventy-one patients completed the survey, with a response rate of 84.5%. Regardless of health literacy, most waitlisted candidates recognized that the current pandemic is a serious situation affecting their care and that COVID-19 poses a significant risk to their health. Despite the increased risks, most patients reported they would choose immediate transplantation if there was no foreseeable end to the pandemic, and especially if the medical urgency did not permit further delay. There were no differences in responses across the patient waitlist groups for heart, kidney, liver, and stem cell transplant.
CONCLUSIONS: These findings can help transplant centers decide how transplantation services should proceed during this pandemic and can be used to educate patients and guide discussions about informed consent for transplant during the COVID-19 pandemic.
Keywords: Health Care Surveys, Health Literacy, Transplantation, Aged, 80 and over, COVID-19, Global Health, Health Knowledge, Attitudes, Practice, Organ Transplantation, Pandemics, Patient Preference, Postoperative Complications, Singapore, Waiting Lists
Background
Coronavirus disease 2019 (COVID-19), which is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, can contribute to a severe clinical course and an increased risk of death in solid organ transplant (SOT) or hematopoietic stem cell transplant (HSCT) recipients. Mortality rates as high as 18% to 27.8% have been reported in SOT recipients who become infected with SARS-CoV-2 [1,2]. This mortality rate has been attributed to the patients’ immunosuppressed state, pre-existing comorbidities, and increased healthcare needs [3]. These observations, together with the diversion of hospital resources toward managing patients with COVID-19, have led to a worldwide decrease in organ donors and the number of transplants performed [4]. SOTs and HSCTs are life-saving procedures that cannot be deferred indefinitely without incurring waitlist dropout, progression of disease, or mortality. Enabling organ transplantation to continue is particularly important in countries with low organ donation rates such as Singapore, where the backlog in transplants has severe ramifications [5]. Worldwide, the transplant community has toiled to develop strategies to make transplants safer and to learn how to manage patients infected with SARS-CoV-2 [1,6,7].
We recognized that one critical aspect of patient care that has not been addressed is the concerns and attitudes of patients toward transplantation during this time. The COVID-19 pandemic has created a potent dilemma for these patients who otherwise would have considered it unthinkable to turn down an organ offer without knowing when another organ would be available. Proceeding with a long-awaited transplant during the pandemic is in essence exchanging the risk of end-stage organ failure, liver, or hematological malignancy for the risk of increased vulnerability to COVID-19. The abundance of emerging data on COVID-19 also makes it difficult for the average patient to appreciate the implications of their decisions on their medical care.
Presently, we do not know what the prevailing attitudes and concerns are among patients waitlisted for SOT and HSCT. In fact, not all SOT and HSCT transplants have the same medical urgency. Therefore, it was crucial for us to understand our patients’ disposition on this issue to guide how we conduct transplantation services. This will also allow us to develop effective patient education strategies and facilitate discussions on informed consent. A particularly vulnerable group are patients with inadequate health literacy (IHL), who may be subject to misinformation and thereby unable to navigate the complex issues surrounding care during this challenging time [8]. Hence, we sought to address these important questions by conducting a standardized phone survey of our top waitlisted patients across the SOT and HSCT programs and determine if IHL impacts their opinions on transplant during the pandemic.
Material and Methods
PATIENTS:
Our primary objective was to determine the opinions and concerns of waitlisted candidates for transplant during the current COVID-19 pandemic. Our secondary objectives were to determine the degree of health literacy in this population, factors associated with IHL, and whether IHL affects patients’ attitudes toward transplant during COVID-19. We identified patients who were actively waiting for or identified to move forward with a heart, kidney, liver, or stem cell transplant at the SingHealth Duke-NUS Transplant Centre. Up to 50 patients aged above 21 years from each service, starting from those either highest on the waitlist or closest to transplant, were identified. Sample size calculation was based on an estimated 50% response rate with a target of 25 responses in the programs with a large waiting list, such as the kidney program [9]. An additional 10 patients were identified from the kidney program of those exclusively awaiting and ready to move forward with a living donor kidney transplant. Patients who were admitted to the hospital were excluded from the survey. A standardized phone interview was conducted by 3 study team members (EKT, YXK, and JBJ). These interviews were conducted between May 4, 2020, and June 1, 2020, also known as the “extended circuit breaker” period, when safe distancing measures were strictly enforced and activities around the country were limited to only essential services [10]. During this time, stay-home notices lasting 14 days were issued to all persons entering the country, and quarantine orders were issued to contacts of a patient confirmed with COVID-19 infection. Three phone call attempts were made per patient, and if a patient remained uncontactable, this would be classified as a nil response and excluded from the cohort. The standardized questionnaire (Appendix 1) was translated and could be administered in English, Mandarin, and Malay languages. Study responses included components of background demographic data, a brief health literacy assessment, and questions related to COVID-19 and patient care.
ASSESSMENT OF HEALTH LITERACY:
The 3-question Short Literacy Survey was used to ascertain the presence of IHL [11,12]. For question 1 (surrogate reader) and question 3 (difficulty learning about health), the options “Always”, “Most of the time”, and “Occasionally” indicated IHL. For question 2 (confidence in forms), the options “Not at all” and “A little bit” indicated IHL. The other options indicated marginal or adequate health literacy. In this study, an IHL response to any of the 3 questions resulted a in classification of IHL.
QUESTIONS RELATED TO COVID-19:
A 30-item survey was designed to assess the following domains: (a) general outlook on the pandemic; (b) patient’s self-assessment of situation on waitlist; (c) impact of COVID-19 on transplant; (d) donor-derived infections; (e) peri- and posttransplant care; (f) willingness to proceed with transplant (Appendix). Each question was asked in a sequential manner. A 3-point rating scale (Yes, No, Do not know) was used in favor of the 5-point Likert scale for ease of delivery over the phone. All patient responses were recorded anonymously. This study was approved by the SingHealth Centralised Institutional Review Board (Ref: 2020/2188).
STATISTICAL ANALYSIS:
Statistical analysis was performed using SPSS software version 20.0 (IBM Corp). Categorical variables were compared using the χ2 test. Linear-by-linear association was applied for ordinal variables. A parallel-forms strategy for reliability testing was introduced using paraphrased or negatively worded questions assessing the same concept. Responses from negatively worded questions underwent reverse scoring. “Do not know” responses were excluded in reliability tests, and the performance of these tests was assessed using the Pearson correlation coefficient. All
Results
HEALTH LITERACY:
The Short Literacy Survey questions 1 (surrogate reader), 2 (confidence in forms), and 3 (difficulty learning about health) indicated IHL in 35.2%, 18.3% and 29.6% of patients, respectively. There was a moderate correlation between questions 1 and 2 (r=0.41, P<0.001); 1 and 3 (r=0.36, P=0.002); 2 and 3 (r=0.41, P<0.001). Using the composite assessment (IHL on any question), 47.9% of respondents were classified as having IHL. Table 2 shows the association between IHL and patient factors. IHL was associated with older age (P=0.003), a lower self-reported level of education (P=0.001), and higher number of children (P=0.001). There were no differences noted between sex (P=0.76) or transplant group (P=0.06).
GENERAL OUTLOOK OF PANDEMIC:
The responses to questions on COVID-19 are detailed in Table 3. Most patients responded that the COVID-19 situation was serious in the country (question 1, 81.7%) and in the world (question 2, 93.0%). More than half answered that the COVID-19 situation was likely to last more than a year (question 4, 59.2%).
SELF-ASSESSMENT OF SITUATION ON WAITLIST:
Most patients were hopeful that they would get a transplant (question 5, 73.2%). Most of the patients were aware that, should their condition deteriorate, they would drop out and be denied a transplant (question 6, 78.9%). A negatively worded version of question 5 was repeated as question 7, and the response was reduced to 57.7% of patients believing that they would not drop out. Reliability testing of question 5 and question 7 (negatively worded) showed no correlation (r=−0.02,
IMPACT OF COVID-19 ON TRANSPLANT:
Most patients responded that transplantation services should continue despite COVID-19 (question 8, 70.4%), and more than half responded that the pandemic had reduced their likelihood of getting a transplant (question 9, 56.3%). Most patients answered that a patient posttransplant was more susceptible to contracting COVID-19 (question 11, 69%), and if infected, would experience a more serious clinical course (question 12, 83.1%).
DONOR–DERIVED INFECTIONS:
Most patients did not think it was safe to receive organs or an allogenic stem cell transplant from a COVID-19-positive donor (question 13, 71.8%). The majority had confidence in the ability to test and exclude COVID-19 in the donor (question 15, 70.4%), and even after the telephone interviewers elaborated on the concept of a false negative result, most patients would accept the result and proceed with a transplant (question 16, 66.2%).
PERI- AND POSTTRANSPLANT CARE:
Nearly all patients were confident that the hospital would take adequate precautions to protect them from hospital-acquired COVID-19 (question 17, 95.8%), though there was some concern about acquiring the infection from other patients (question 18, 40.8%) or healthcare workers (question 19, 35.2%). The majority would continue with transplantation at the hospital even if there were active COVID-19 inpatients (question 20, 67.6%). Most patients were agreeable to proceed even if no visitors were allowed (question 21, 70.4%). Question 21 showed a variance in responses between organ groups (data not shown,
Only a small proportion expressed concern about traveling for the outpatient follow-up visits, which could be more intensive after transplant (question 22, 29.6%), and the inability to obtain prescription medications (question 23, 19.7%). Approximately one-third of the patients were concerned that their decision to transplant would incur a risk to their caregiver (question 24, 36.6%). The majority of respondents thought that healthcare workers were at increased risk of getting COVID-19 from transplantation activities (question 25, 62%), but most felt that, despite this risk, transplantation services should continue (question 26, 73.2%).
WILLINGNESS TO PROCEED WITH TRANSPLANT:
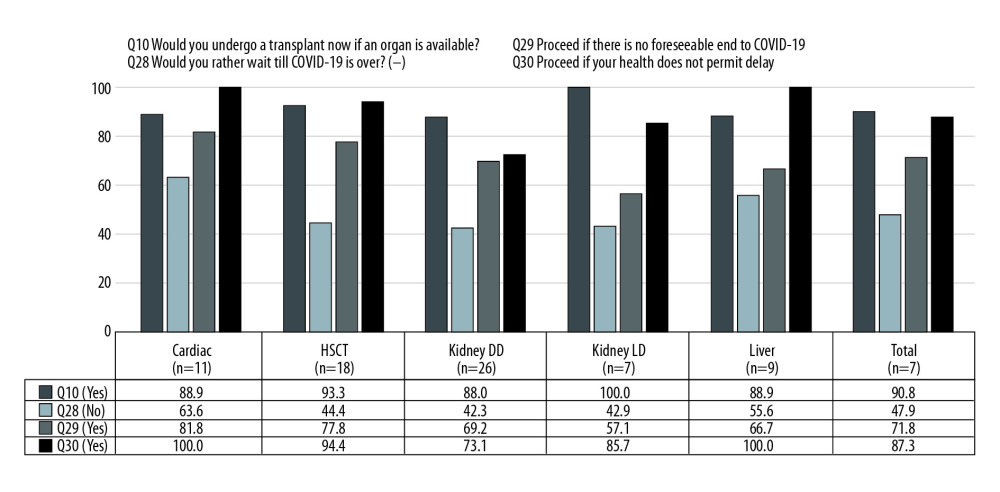
Early in the survey, most patients responded that they would agree to proceed with a transplant immediately if it were available (question 10, 83.1%). This concept was retested at the end of the questionnaire with a negatively worded version, but then only half of patients responded that they would not wait until COVID-19 was over (question 28, 47.9%). There was only a low degree of correlation between question 10 and question 28 (negatively worded), indicating that the response pattern had changed (r=−0.30, P=0.02). However, most patients would agree to transplant immediately if there were no foreseeable end to the COVID-19 pandemic (question 29, 71.8%) or if their medical condition would not permit them to wait until COVID-19 was over (question 30, 87.3%). The Figure 1 shows the distribution of responses of questions 28, 29, and 30 across organ groups, with kidney patients divided into deceased donor and living donor groups (P=NS). Table 3 shows the comparison of responses between patients with IHL with those having marginal or adequate health literacy; there were no differences in responses across all the questions (P=NS).
Discussion
The COVID-19 outbreak has disrupted the delivery of transplantation services, and the impetus is on transplant providers to adapt our care model during this crisis to meet the needs of our patients. The requirement for safe distancing measures has resulted in a reduction in outpatient clinic visits, where we typically get the opportunity to assess patient sentiment and counsel them on their healthcare decisions. Although we can choose to simply review the latest evolving evidence on COVID-19 care for transplant patients and make decisions for them under the paternalistic model of care, we prefer patient-centric care using the shared decision-making model, which is also the preferred method of patients actively awaiting a transplant [13]. Thus, this study was necessary so that we could continue to engage and involve our patients in the decision-making process during this challenging time.
Initially, we acquired a baseline assessment of health literacy because such literacy can affect patients’ comprehension of issues and their decision-making ability. The 3-question Short Literacy Survey was appropriate for our study because it was easy to administer over the phone, and it was designed primarily to identify IHL [11]. While patients with marginal and adequate health literacy may have their own set of concerns and opinions, our focus was on the most vulnerable group of patients, those with IHL, who could be struggling to resolve their concerns with COVID-19. We recognize the possibility of a response bias since respondents may have been embarrassed to admit that they needed help or failed to comprehend information; although, this effect might have been minimized in a phone as compared to a face-to-face interview. Therefore, our finding of 47.9% patients having IHL may still be an underestimate of the true percentage of patients with IHL. The population census has shown that the oldest members of the population have not achieved the high level of education achieved by the younger population [14], and our finding of IHL among older individuals corroborates this data. Future patient education efforts can be focused on older patients, particularly those with only primary or secondary level education. Also, the trend toward increasing IHL among those with more children reflects the population census finding that women with a higher level of education tend to have fewer children [14].
Because our intent was to gather the current concerns and opinions of patients actively awaiting transplant, we excluded patients who were admitted to the hospital, for 2 reasons: first, active illness may have prohibited their participation; for example, liver decompensation and encephalopathy or other patient illness could have resulted in a partially completed survey due to fatigue; and second, critically ill patients who have transplant as an only option would be more likely to defer to physician recommendations, thus influencing responses that were meant to reflect patient opinion [15].
The most important domain we wanted to assess in this study was the willingness to transplant. While most patients had initially responded that they would proceed with transplant immediately (question 10, 90.8%), after the series of questions designed to introduce thoughts on the risks of COVID-19 to a transplanted patient, including donor-derived infections and peri- and posttransplant care, we demonstrated that the proportion of patients keen to proceed with transplantation decreased by half (question 28, 47.9%). However, once the factors of waiting time and medical urgency were introduced, the proportion of patients who wished to move forward with transplantation increased to 87.3%. This is consistent with previous studies that demonstrated that patients are willing to accept increased risks when their clinical situation is deteriorating [13]. The survey design did not allow an objective assessment of the respondents’ medical condition or urgency to transplant, which would influence their willingness to proceed with transplantation during COVID-19. Instead, our strategy was to survey patients for whom this issue would be most relevant, namely, those highest on the waiting list or close to scheduled transplant (HSCT or living donor kidney). Hence, while we expect that the responses from this study cohort represent an upper estimate of all patients on the waitlist, collecting responses from those whose intended transplant is in the distant future would also not be relevant to the present situation.
While there were no statistical differences between responses from the various organ groups, there was a trend toward a higher threshold to transplant for patients awaiting a kidney transplant, compared to the other organ programs. This was not unexpected since patients with end-stage kidney disease have an effective medical alternative to transplantation, compared to the other organ groups [13]. Companionship has been found to be an important component of care among patients on hemodialysis [16]. This may explain our observation that, compared to patients in other groups, patients awaiting a kidney transplant were more likely to decline an immediate transplant if hospital visitors were not allowed (
There are some limitations to this study. Because of the time sensitive nature of this research and that we wanted to conduct this survey during the peak of COVID-19 sentiment (during the aforementioned circuit breaker period), development of a pilot version of the questionnaire was not performed. The limited size of the patient population also did not allow the creation of a separate validation cohort. Next, there is the challenge of generalizing these results to other populations. The number of community cases of COVID-19 or deaths from COVID-19 in Singapore were not as high as in other countries that perform a large volume of transplants [18]. However, the perceived threat of COVID-19 has been found to correlate with the degree of preventative health behaviors adopted by countries worldwide, something Singapore had scored high in [19]. Therefore, it is reasonable to consider our survey results as representative of a population that is actively concerned with COVID-19. Finally, the disease epidemiology in Singapore is such that the sample population was inherently small and restrictive. Thus, extensive analyses of differences in opinions between groups of patients may not be statistically meaningful. Nevertheless, this also meant that we could engage most of our patients and achieve a relatively high response rate of 84.5% over the phone, allowing an insight into the general sentiment of the patients.
Conclusions
In this study we found that regardless of health literacy, most waitlisted candidates recognized that the pandemic was a serious situation affecting their care, and that COVID-19 posed a significant risk to a transplanted patient’s health. Most patients did not think that the additional inconveniences or risks resulting from continuation of transplantation services during the pandemic were prohibitive. Despite the increased risks, most patients were inclined to undergo immediate transplantation if there was no foreseeable end to the pandemic, and especially if medical urgency did not permit further delay. These findings will be useful to guide transplant centers in deciding whether transplantation services should proceed during this pandemic and to educate patients and guide patient discussions on informed consent for transplant during the COVID-19 pandemic.
References
1. Pereira MR, Mohan S, Cohen DJ, COVID-19 in solid organ transplant recipients: Initial report from the US epicenter: Am J Transplant, 2020; 20(7); 1800-808
2. Fernández-Ruiz M, Andrés A, Loinaz C, COVID-19 in solid organ transplant recipients: A single-center case series from Spain: Am J Transplant, 2020; 20(7); 1849-58
3. Banerjee D, Popoola J, Shah S, COVID-19 infection in kidney transplant recipients: Kidney Int, 2020; 97(6); 1076-82
4. Loupy A, Aubert O, Reese PP, Organ procurement and transplantation during the COVID-19 pandemic: Lancet, 2020; 395(10237); e95-96
5. Tan EK, Goh BKP, Lee SY, Liver transplant waitlist outcomes and the allocation of hepatocellular carcinoma model for end-stage liver disease exception points at a low-volume center: Transplant Proc, 2018; 50(10); 3564-70
6. Zhong Z, Zhang Q, Xia H, Clinical characteristics and immunosuppressant management of coronavirus disease 2019 in solid organ transplant recipients: Am J Transplant, 2020; 20(7); 1916-21
7. Chung SJ, Tan EK, Kee T, Practical considerations for solid organ transplantation during the COVID-19 global outbreak: The experience from Singapore: Transplant Direct, 2020; 6(6); e554
8. Paakkari L, Okan O, COVID-19: Health literacy is an underestimated problem: Lancet Public Health, 2020; 5(5); e249-e50
9. Phua J, Lim HF, Tay CK, Aung NW, Public awareness of sepsis and stroke in Singapore: A population-based survey: Ann Acad Med Singapore, 2013; 42(6); 269-77
10. Ministry of Health Singapore: 2020 Press Release: Circuit breaker to minimise further spread of COVID-19
11. Chew LD, Bradley KA, Boyko EJ, Brief questions to identify patients with inadequate health literacy: Fam Med, 2004; 36(8); 588-94
12. Powers BJ, Trinh JV, Bosworth HB, Can this patient read and understand written health information?: JAMA, 2010; 304(1); 76-84
13. Op den Dries S, Annema C, Berg AP, Shared decision making in transplantation: How patients see their role in the decision process of accepting a donor liver: Liver Transpl, 2014; 20(9); 1072-80
14. Singapore Department of Statistics: Population Trends, 2019 https://www.singstat.gov.sg/publications/population/populationtrends
15. Pentz RD, Pelletier W, Alderfer MA, Shared decision-making in pediatric allogeneic blood and marrow transplantation: What if there is no decision to make?: Oncologist, 2012; 17(6); 881-85
16. Shahgholian N, Yousefi H, The lived experiences of patients undergoing hemodialysis with the concept of care: A phenomenological study: BMC Nephrol, 2018; 19(1); 338
17. Boyarsky BJ, Po-Yu Chiang T, Werbel WA, Early impact of COVID-19 on transplant center practices and policies in the United States: Am J Transplant, 2020; 20(7); 1809-18
18. Ministry of Health Singapore: COVID-19 Situation Report, 2020 https://www.moh.gov.sg/covid-19/situation-report
19. Dryhurst S, Schneider CR, Kerr J, Risk perceptions of COVID-19 around the world: J Risk Res, 2020; 1-13
Tables
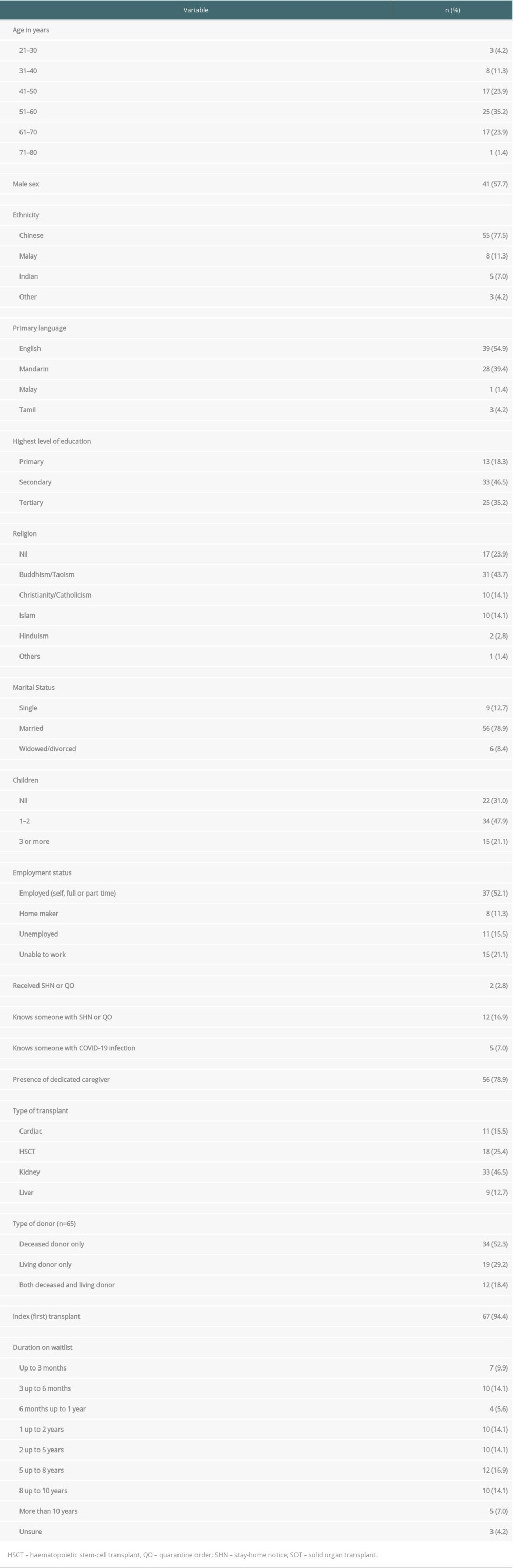 Table 1. Demographic and transplant characteristics of SOT and HSCT respondents (n=71).
Table 1. Demographic and transplant characteristics of SOT and HSCT respondents (n=71).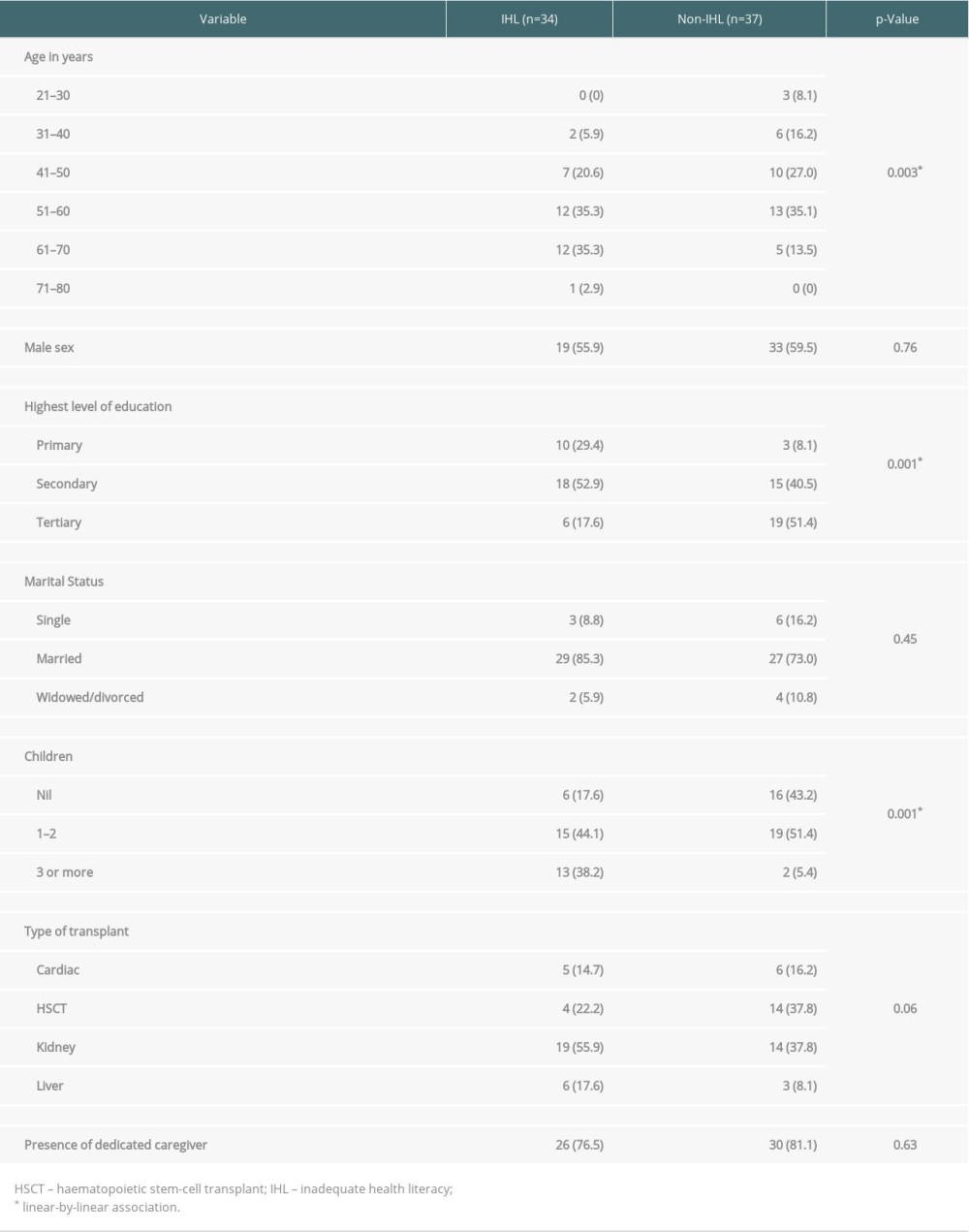 Table 2. Inadequate health literacy and association with factors (n=71).
Table 2. Inadequate health literacy and association with factors (n=71).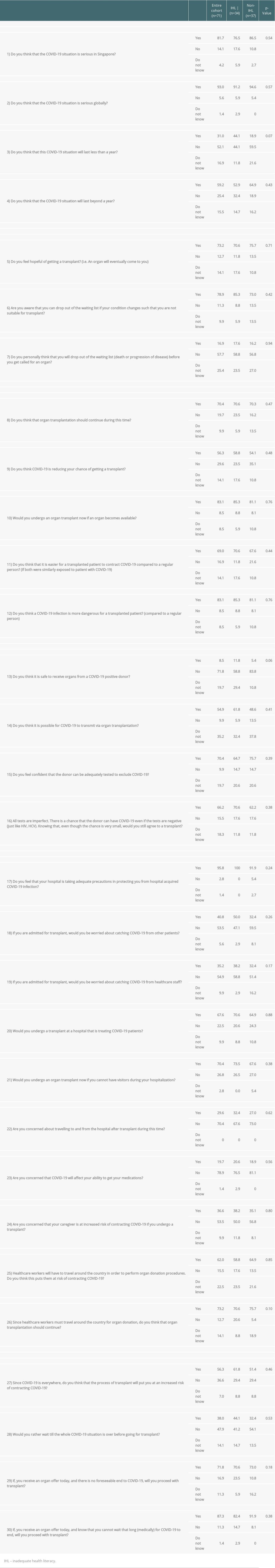 Table 3. Patient responses to questions on COVID-19 vs. presence of IHL (n=71).
Table 3. Patient responses to questions on COVID-19 vs. presence of IHL (n=71).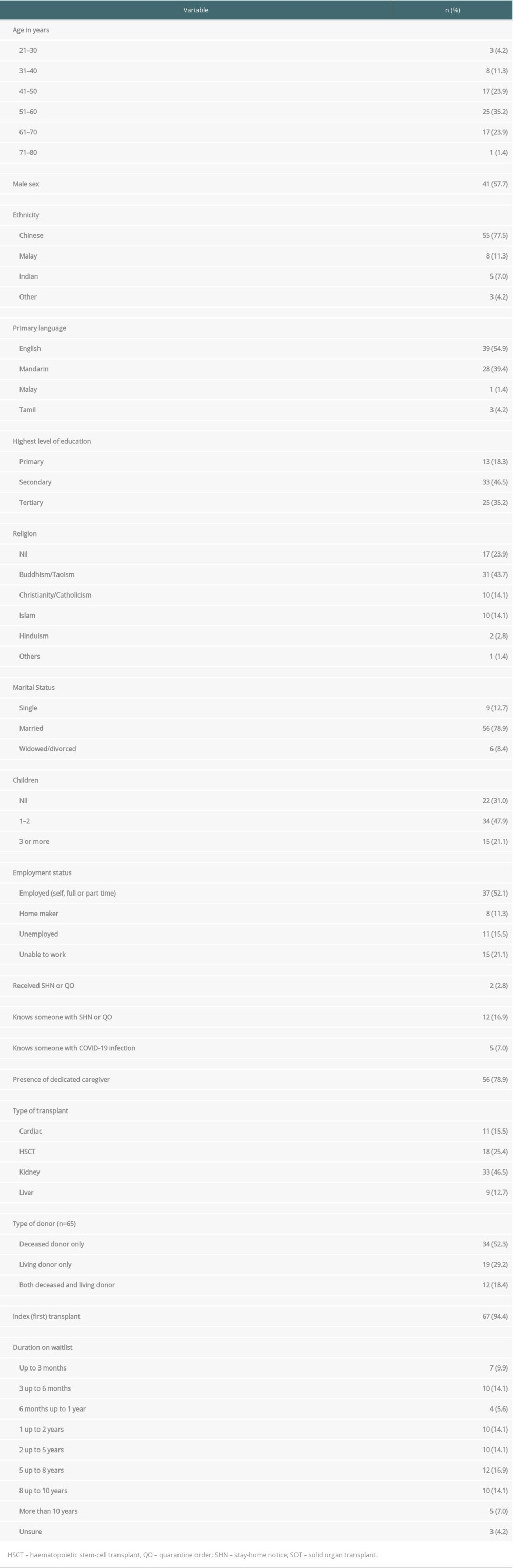 Table 1. Demographic and transplant characteristics of SOT and HSCT respondents (n=71).
Table 1. Demographic and transplant characteristics of SOT and HSCT respondents (n=71).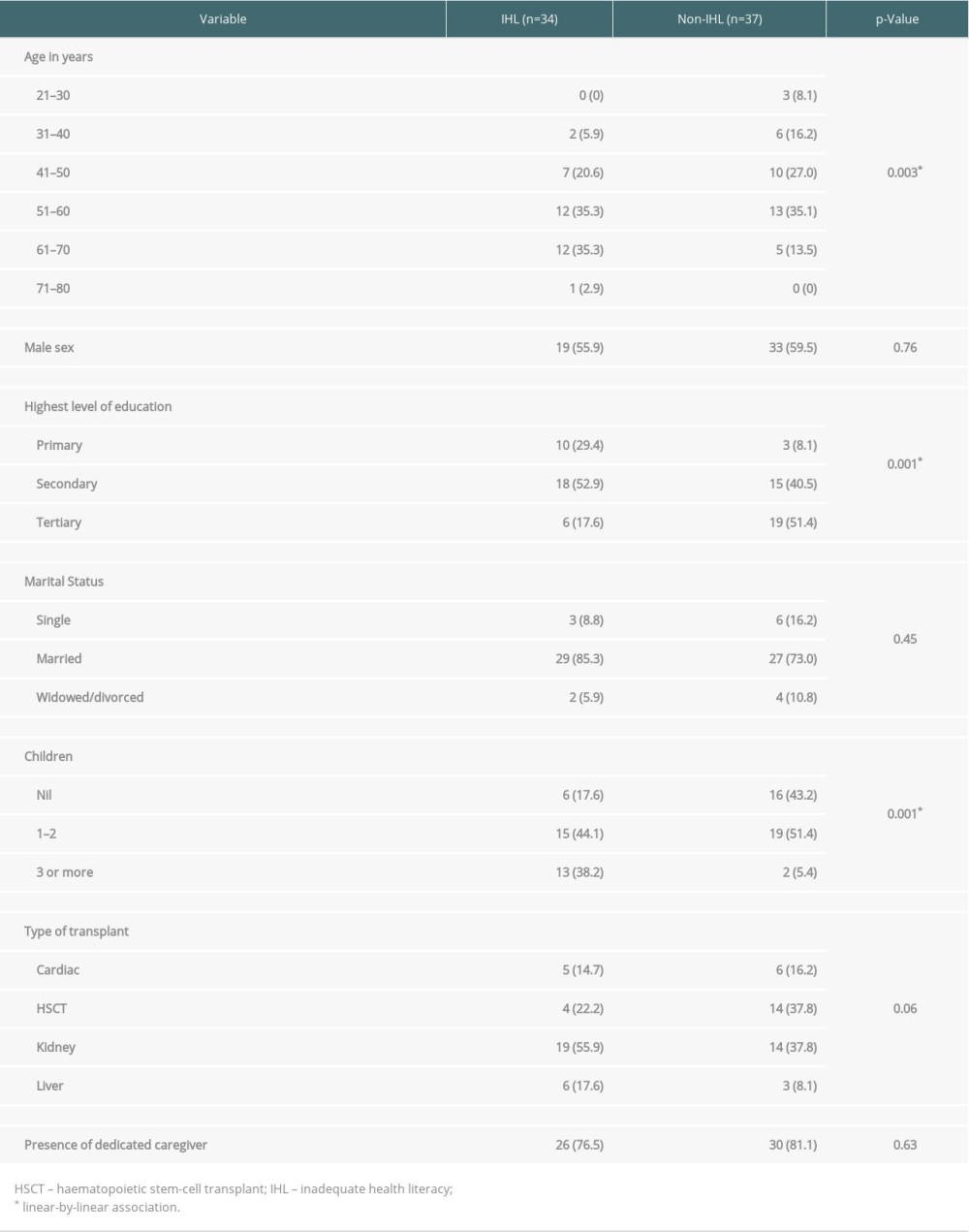 Table 2. Inadequate health literacy and association with factors (n=71).
Table 2. Inadequate health literacy and association with factors (n=71).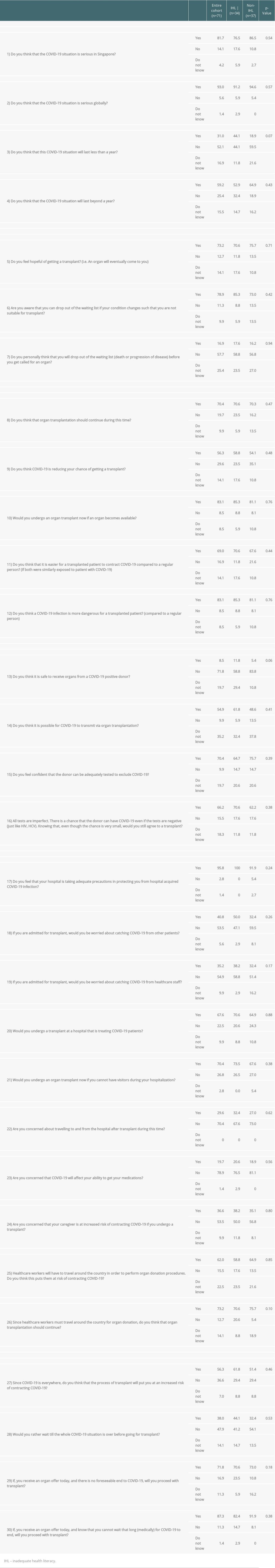 Table 3. Patient responses to questions on COVID-19 vs. presence of IHL (n=71).
Table 3. Patient responses to questions on COVID-19 vs. presence of IHL (n=71). In Press
18 Mar 2024 : Original article
Does Antibiotic Use Increase the Risk of Post-Transplantation Diabetes Mellitus? A Retrospective Study of R...Ann Transplant In Press; DOI: 10.12659/AOT.943282
20 Mar 2024 : Original article
Transplant Nephrectomy: A Comparative Study of Timing and Techniques in a Single InstitutionAnn Transplant In Press; DOI: 10.12659/AOT.942252
28 Mar 2024 : Original article
Association Between FEV₁ Decline Rate and Mortality in Long-Term Follow-Up of a 21-Patient Pilot Clinical T...Ann Transplant In Press; DOI: 10.12659/AOT.942823
02 Apr 2024 : Original article
Liver Transplantation from Brain-Dead Donors with Hepatitis B or C in South Korea: A 2014-2020 Korean Organ...Ann Transplant In Press; DOI: 10.12659/AOT.943588
Most Viewed Current Articles
05 Apr 2022 : Original article
Impact of Statins on Hepatocellular Carcinoma Recurrence After Living-Donor Liver TransplantationDOI :10.12659/AOT.935604
Ann Transplant 2022; 27:e935604
12 Jan 2022 : Original article
Risk Factors for Developing BK Virus-Associated Nephropathy: A Single-Center Retrospective Cohort Study of ...DOI :10.12659/AOT.934738
Ann Transplant 2022; 27:e934738
22 Nov 2022 : Original article
Long-Term Effects of Everolimus-Facilitated Tacrolimus Reduction in Living-Donor Liver Transplant Recipient...DOI :10.12659/AOT.937988
Ann Transplant 2022; 27:e937988
15 Mar 2022 : Case report
Combined Liver, Pancreas-Duodenum, and Kidney Transplantation for Patients with Hepatitis B Cirrhosis, Urem...DOI :10.12659/AOT.935860
Ann Transplant 2022; 27:e935860