14 February 2022: Human Study
Degree of Myopia and Reduced Physical Activity in 3600 College Students in China
Xiangyu Zhao1ABCDEG, Yanan Zhang2ABCFG*DOI: 10.12659/MSMBR.934807
Med Sci Monit Basic Res 2022; 28:e934807
Abstract
BACKGROUND: This study aimed to evaluate the degree of myopia and reduced physical activity in 3600 college students in China between 2018 and 2020.
MATERIAL AND METHODS: The study included 3600 participants (1742 men and 1858 women) aged 19 to 23 years from a Chinese college. The distribution of the levels of eyesight associated with physical exercise was assessed using the Early Treatment Diabetic Retinopathy Study chart measurement method.
RESULTS: The rates of myopia of students enrolled students in 2018, 2019, and 2020 were 84.31%, 87.22%, and 89.17%, respectively, which showed an increasing trend (P<0.01). For the students starting in 2018, the rate of myopia showed an upward trend in their 3 years of college (P<0.01). The incidence of myopia was significantly different during the academic year between students who participated and did not participate in sports clubs (P<0.01).
CONCLUSIONS: The findings from this study showed that between 2018 and 2020 there was a high prevalence of myopia in college students in China, which increased annually and was associated with reduced physical activity while at college. These findings may have public health implications for improving physical activity in this population. Physical exercise could effectively prevent the occurrence of myopia, improve the visual status of students, and alleviate the decline of vision.
Keywords: Eye, Medical Informatics, Plyometric Exercise, Students, Medical, Adult, China, Exercise, Female, Humans, Male, Myopia, Prevalence, Students, young adult
Background
Myopia is common among college students and not only affects physical health, but also poses risks to other eye complications. It also adversely affects students’ mental health, study life, and employment. Studies have shown that the mechanism of myopia formation is complex and includes a combination of factors, such as hereditary [1–4], environment [5–9], and lifestyle [10–12]. Effectively preventing myopia, providing intervention measures to reverse the current situation of myopia rate among college students, alleviating the development speed of myopia, and improving the level of vision are of great significance to the health of college students.
Despite the importance visual acuity to activities of daily living, the most commonly used measurement of vision, visual acuity, is relatively crude because it evaluates only 1 of the broad range of visual functions [13]. This article mainly uses the Bailey-Lovie or Early Treatment Diabetic Retinopathy Study (ETDRS) chart method to measure the visual acuity of college students. Standardization of the task in this test requires letters of equal legibility, with the same number of letters in each row, and uniform spacing between the letters and rows. There is also a logarithmic progression in letter size [14].
College sports clubs provide a physical fitness platform that can bring students with the same interests, hobbies, and motor skills together to engage in extracurricular training and competition. It is an integrated curriculum teaching mode with sound organization and management. In this study, we encouraged students to participate in sports clubs and do strengthening exercises to alleviate myopia. This included having students play basketball, table tennis, martial arts, and other sporting activities every week for no less than 3 days a week and 2 h a day. In addition, school basketball, table tennis, martial arts, and other individual clubs have hundreds of games every academic year, and students are required to actively participate. Club members are passionate in training and competition, which enhance their physical and mental health and cultivate sporting interests and habits. In their spare time, students can actively walk around the campus and go to the playground, effectively reducing the risk of myopia, improving vision and recovery, and intervening in the decline of vision [15,16].
Therefore, this study aimed to evaluate the degree of myopia using the Early Treatment Diabetic Retinopathy Study chart and the effects of reduced physical activity on myopia in 3600 college students in China between 2018 and 2020.
Material and Methods
PARTICIPANTS:
A school-based study was performed for students who were enrolled as freshmen in years 2018, 2019, and 2020. Upon entry, the students underwent eyesight testing. The freshmen starting in 2018 were tracked and tested for 3 years (from 2018 to 2021), the freshmen of 2019 were tracked and tested for 2 years (from 2019 to 2021), and the freshmen of 2020 were tracked and tested for 1 year (from 2020 to 2021). In total, 3600 students participated, including 1200 starting in each year. Written informed consent was obtained from all participants, and the study was approved by the local Ethics Committee.
EYESIGHT TEST:
The Early Treatment Diabetic Retinopathy Study chart was used to measure visual acuity of students starting in 2018, 2019, and 2020, and to test the visual acuity of the students starting in 2018 for 3 consecutive years.
In addition, 100 members of the basketball club, 100 members of the table tennis club, 100 members of the Wushu club, and 200 non-club members were selected to test the vision at the beginning and end of the 2019 sophomore year and to compare the development of vision. Each club member participated in club training or competitions no less than 3 times a week for no less than 2 h each time. Non-club members continued with normal study and daily activities.
Regarding visual acuity criteria, uncorrected visual acuity of 5.0 or better was considered normal eyesight, otherwise it was considered myopia. The degree of myopia was divided into 3 categories: low myopia (≤-3.00D), moderate myopia (−3.00 to −6.00 D), and high myopia (≥-6.00D).
STATISTICAL ANALYSIS:
Analysis of variance was used for comparison of physical performance among different variables.
Results
Table 1 shows the myopia rates of new students entering the college in 2018, 2019, and 2020 were 84.33%, 87.25%, and 89.17%, respectively, and the average myopia rate was 86.92%. The moderate and high myopia rates were 20.00% and 13.17%, 21.00% and 15.17%, 26.25% and 24.17%, respectively. Moderate and high myopia showed an increasing trend (
From the results of the visual test for the 3 consecutive years of the class starting in 2018, the myopia rate showed an increasing trend (
Tables 3–6 show there was a significant difference in the incidence of myopia between sports clubs’ members (basketball, table tennis, wushu) and non-club members during the 2019 academic year (
Among the 2017 students in the survey, 300 students participated in sports club activities every day, of which 209 students (57.93%) were nearsighted. A total of 200 students did not participate in the club, of which 183 (91.50%) had myopia. The chi-squared test was used to determine whether physical exercise had an effect on the prevention of myopia, and the difference was statistically significant (chi-squared value=112,
Discussion
The results of the study show that the prevalence of myopia among college students gradually increased. The total myopia rate in this survey was as high as 84.33%, and the prevalence gradually increased with time. Controlling the development of myopia is critical. At the same time, research also shows that physical exercise can effectively alleviate myopia.
The rate of myopia and high myopia of Chinese college students increased yearly, a serious situation calling for prevention and control (Figure 1). Evidence indicates that participation in sports can prevent and control the occurrence of myopia [19–21]. Jesus et al [19] investigated the differences in visual functions between people who play basketball and those who do not and found that basketball players had greater near-point convergence and halo discrimination. Yurova et al [20] divided 600 adolescents into exercise and non-exercise groups, and each group was then divided into a group with emmetropia, with low and moderate myopia, from the beginning and end of the eyesight test comparison. The incidence of myopia in the exercise group was low, and the sports activities in the low and moderate myopia group were better for maintaining current visual acuity and delaying the development of myopia. Jacobsen et al [21] conducted a 2-year follow-up study with 156 students at the University of Copenhagen. The results showed that physical activity was negatively correlated with myopic refractive changes and contributed to the improvement of myopia.
The mechanism of myopia formation is caused by a decrease in the accuracy of the regulation of the ciliary muscles and coordination of function. The ciliary muscles cannot relax with distant vision. The ciliary muscles have a regulation lag with near vision, and the sensitivity and accuracy are decreased. In sports, the eye relaxes the ciliary muscles by constantly looking far and near, so that the sensitivity and accuracy are effectively enhanced. In ball sports, such as table tennis and basketball, the eyes should always watch the fast-moving, whirling and spinning balls. The eyes are constantly changing between distant and near vision, and the blood circulation and metabolic functions are enhanced. Eye fatigue was effectively restored, and vision improved, as shown in Figure 2. Similarly, non-ball wushu sports can also accelerate the blood circulation inside the eyeball, enhance metabolism, and effectively change the stiffness state of the ciliary muscle and the adjustment ability of the refractive system, thereby achieving the prevention and treatment of myopia, as shown in Figure 3.
This study had some limitations. We did not control possible confounding factors, including the time spent on electronic devices, such as computers and mobile phones, and the specific study and rest time of each student. The exclusion of individuals who were unable to complete the test may have led to bias.
Conclusions
The findings from this study showed that between 2018 and 2020 there was a high prevalence of myopia in Chinese college students, which increased annually and was associated with reduced physical activity while at college. These findings may have public health implications for improving physical activity in this population.
Figures
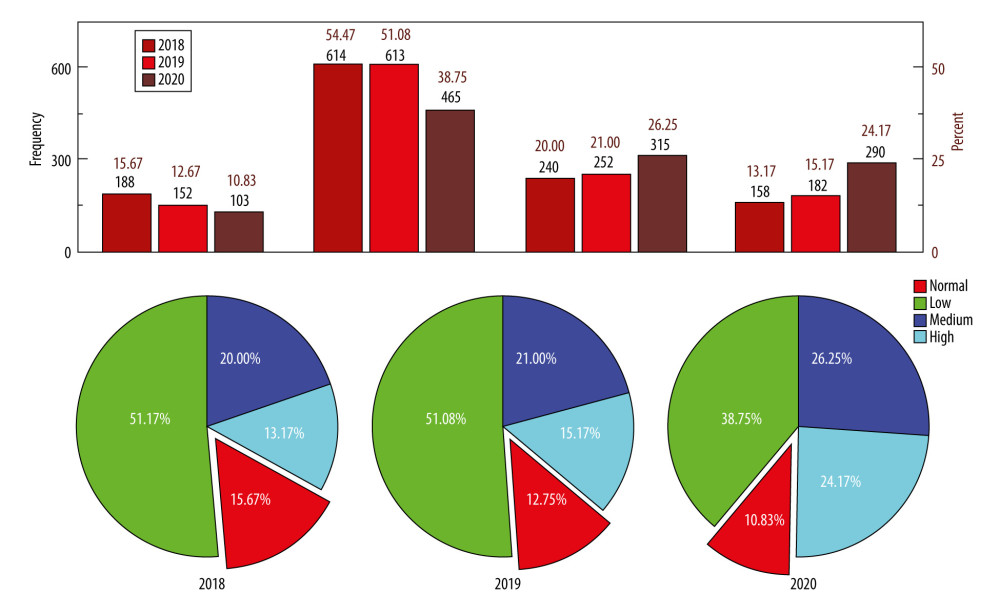 Figure 1. The distribution map of the level of college student’s eyesight for freshmen starting in 2018, 2019, and 2020 in China.
Figure 1. The distribution map of the level of college student’s eyesight for freshmen starting in 2018, 2019, and 2020 in China. 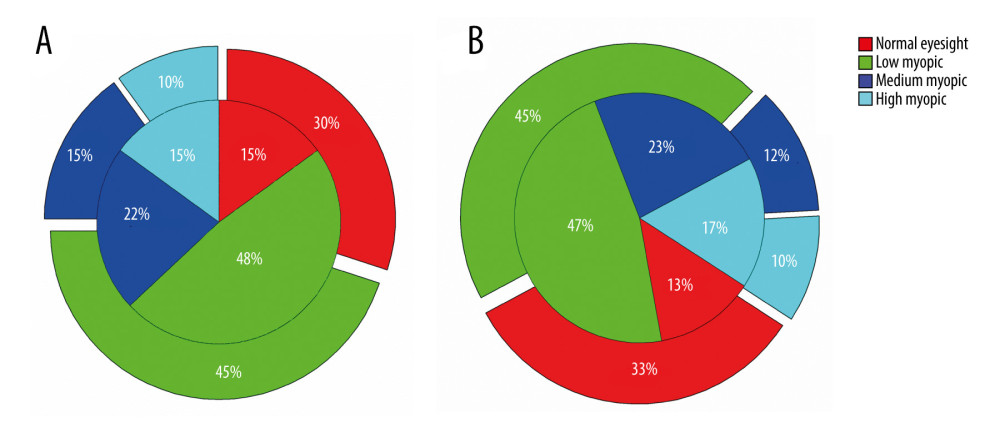 Figure 2. The distribution map of the level of college student’s eyesight in ball sports clubs in China. The inner and outer circles of the pie chart indicate the beginning and end of the school year, respectively. (A) Basketball clubs; (B) table tennis clubs.
Figure 2. The distribution map of the level of college student’s eyesight in ball sports clubs in China. The inner and outer circles of the pie chart indicate the beginning and end of the school year, respectively. (A) Basketball clubs; (B) table tennis clubs. 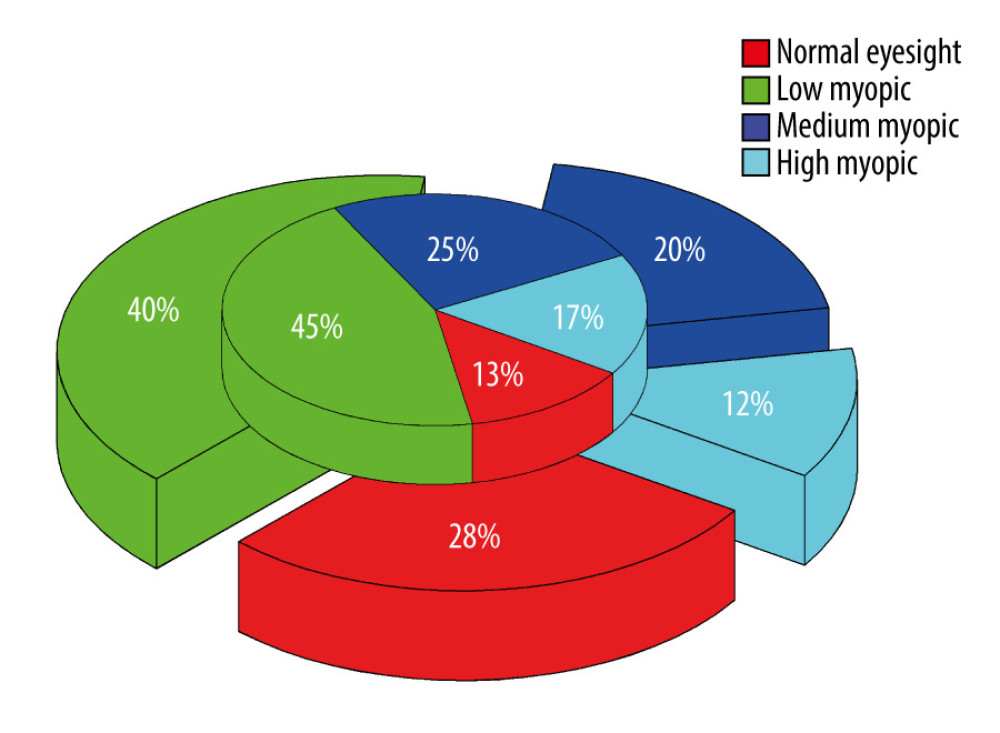 Figure 3. The distribution map of the level of college student’s eyesight of non-ball wushu sports clubs in China. The inner and outer circles of the pie chart indicate the beginning and end of the school year, respectively.
Figure 3. The distribution map of the level of college student’s eyesight of non-ball wushu sports clubs in China. The inner and outer circles of the pie chart indicate the beginning and end of the school year, respectively. Tables
Table 1. Vision test results of freshmen classes starting in years 2018, 2019, 2020 (n=3600).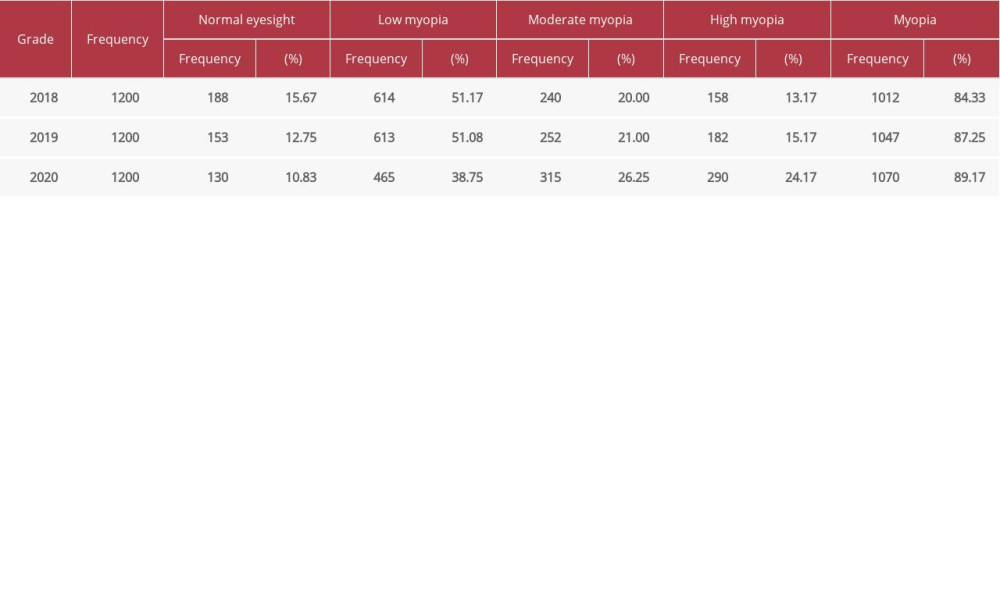 Table 2. Vision test results for the 3 consecutive academic years of the class starting in 2018 (n=1200).
Table 2. Vision test results for the 3 consecutive academic years of the class starting in 2018 (n=1200).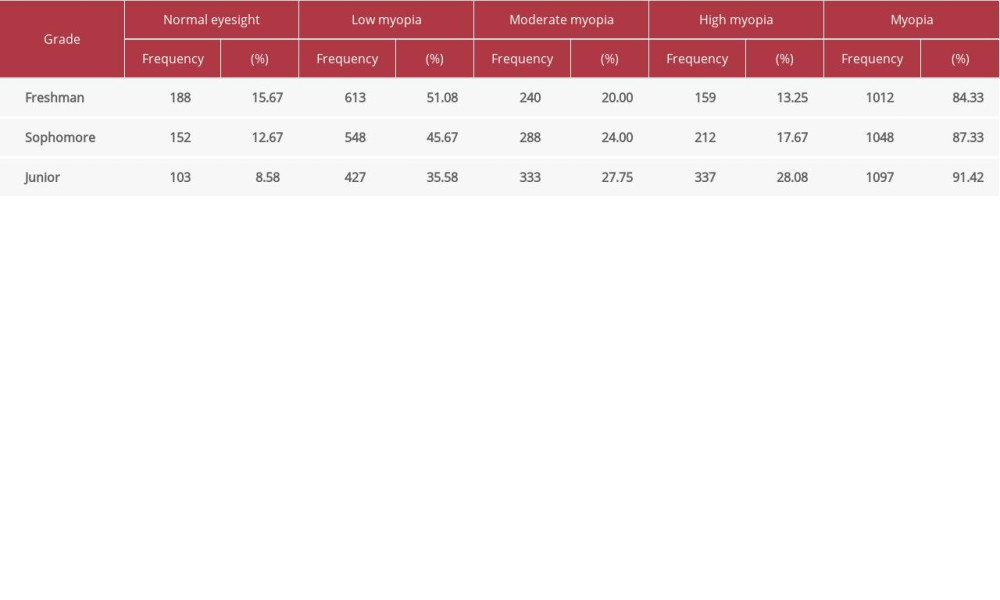 Table 3. Visual acuity test results of non-club members during the academic year for class starting 2019 (n=200).
Table 3. Visual acuity test results of non-club members during the academic year for class starting 2019 (n=200).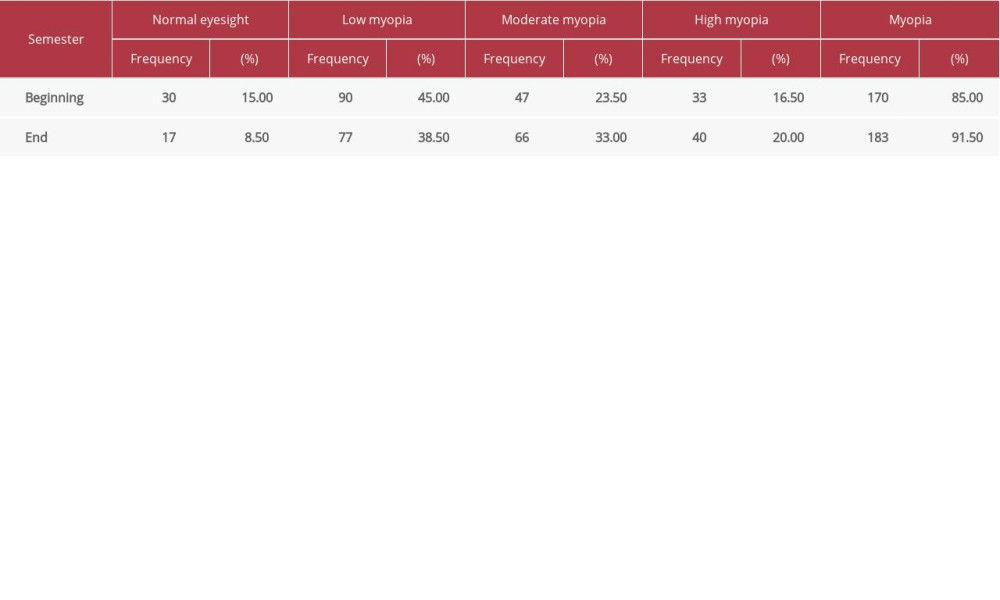 Table 4. Visual acuity test results for basketball club members during the 2019 academic year for class starting in 2018 (n=100).
Table 4. Visual acuity test results for basketball club members during the 2019 academic year for class starting in 2018 (n=100).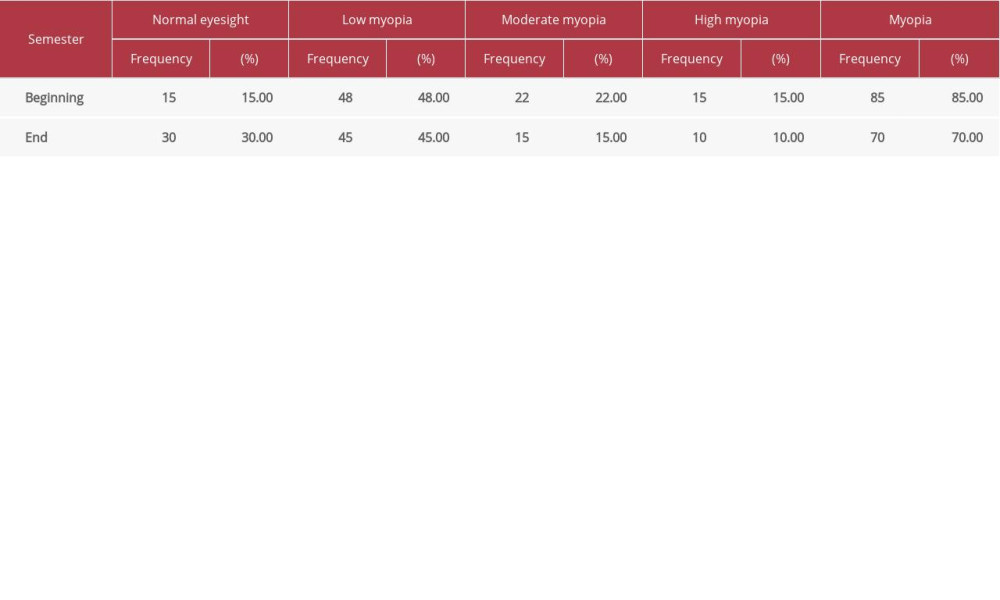 Table 5. Visual acuity test results for table tennis club members during the 2019 academic year for class starting in 2018 (n=100).
Table 5. Visual acuity test results for table tennis club members during the 2019 academic year for class starting in 2018 (n=100).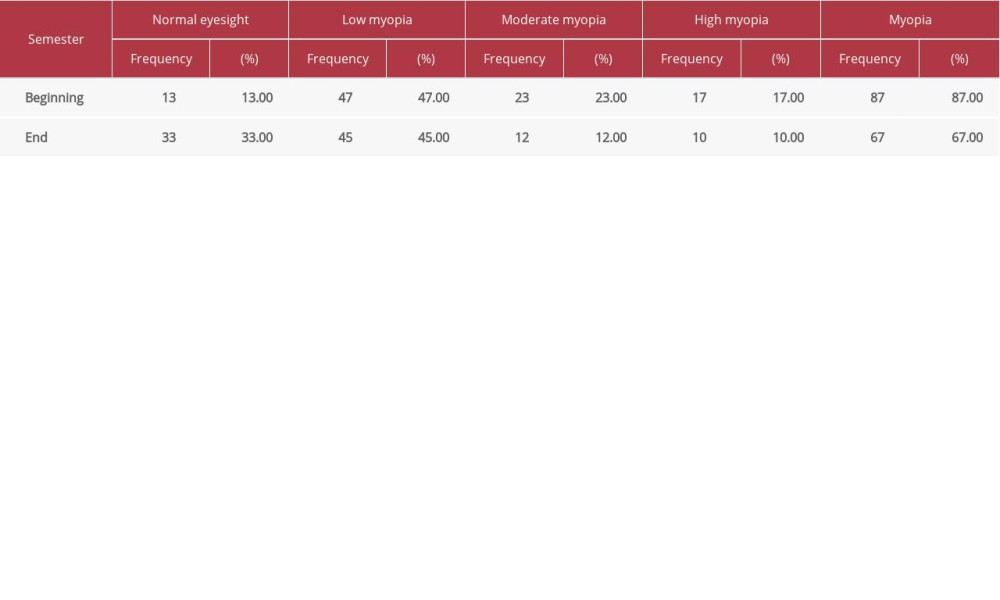 Table 6. Visual acuity test results for wushu club members during the 2019 academic year for class starting in 2018 (n=100).
Table 6. Visual acuity test results for wushu club members during the 2019 academic year for class starting in 2018 (n=100).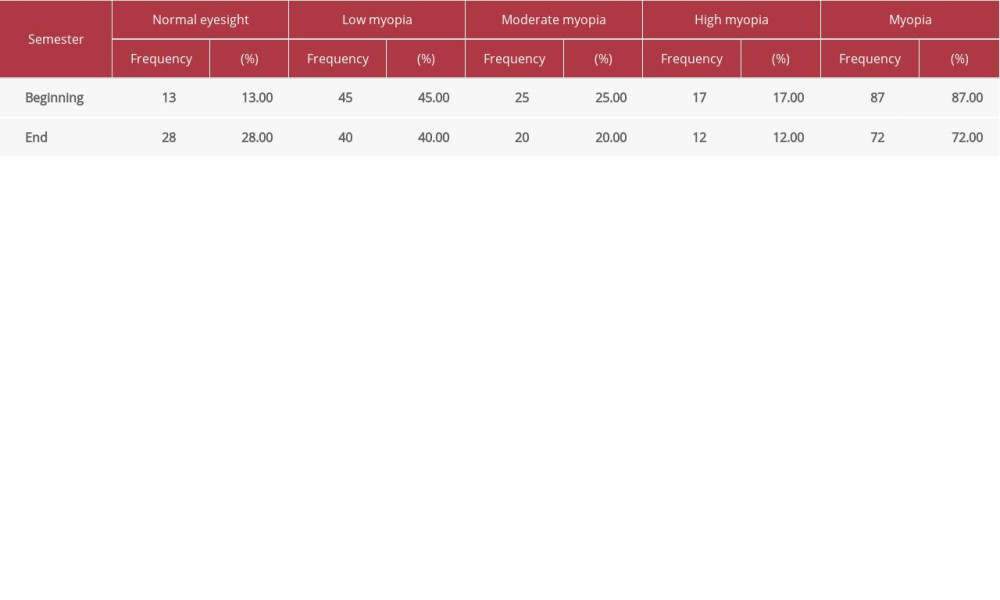
References
1. Berg RVD, Dirani M, Chen CY, Myopia and personality: The Genes in Myopia (GEM) personality study: Invest Ophthalmol Vis Sci, 2008; 49(3); 882-86
2. Bullimore MA, Conway R, Nakash A, Myopia in optometry students: Family history, age of onset and personality: Ophthalmic Physiol Opt, 2010; 9(3); 284-88
3. Majava M, Bishop PN, Hägg P, Novel mutations in the small leucine-rich repeat protein/proteoglycan (SLRP) genes in high myopia: Hum Mutat, 2010; 28(4); 336-44
4. Dirani M, Islam A, Baird PN, Body stature and myopia – The Genes in Myopia (GEM) twin study: Ophthalmic Epidemiol, 2009; 15(3); 135-39
5. Ip JM, Rose KA, Morgan IG, Myopia and the urban environment: Findings in a sample of 12-year-old Australian school children: Invest Ophthalmol Vis Sci, 2008; 49(9); 3858-63
6. Flitcroft DI, The complex interactions of retinal, optical and environmental factors in myopia aetiology: Prog Retin Eye Res, 2012; 31(6); 622-60
7. Feldkämper M, Schaeffel F, Interactions of genes and environment in myopia: Dev Ophthalmol, 2003; 37(37); 34
8. Frcs MM, Pakrasi S, Garg SP, The role of environmental factors and hereditary predisposition in the causation of low myopia: Acta Ophthalmologica, 2010; 66(S185); 54-57
9. Morgan IG, Rose K, Yunnan minority eye study suggests that ethnic differences in myopia are due to different environmental exposures: Invest Ophthalmol Vis Sci, 2015; 56(8); 4430
10. Era P, Myopia, use of eyes, and living habits among men aged 33–37 years: Acta Ophthalmologica, 2010; 63(4); 395-400
11. Choi KY, Yu WY, Chi L, Childhood exposure to constricted living space: A possible environmental threat for myopia development: Ophthalmic Physiol Opt, 2017; 37(5); 568-75
12. Iribarren R, Iribarren G, Castagnola MM, Family history and reading habits in adult-onset myopia: Curr Eye Res, 2002; 25(5); 309-15
13. Kniestedt C, Stamper RL, Visual acuity and its measurement: Ophthalmol Clin North Am, 2003; 16(2); 155-70
14. Bailey IL, Lovie JE, New design principles for visual acuity letter charts: Optom Vis Sci, 1976; 53(11); 740-45
15. Lu C, Stolk RP, Sauer PJ, Factors of physical activity among Chinese children and adolescents: A systematic review: Int J Behav Nutr Phys Act, 2017; 14(1); 36
16. Qu Y, Yu J, Xia W, Correlation of myopia with physical exercise and sleep habits among suburban adolescents: J Ophthalmol, 2020; 2020(3); 1-10
17. Harvey EM, Dobson V, Miller JM, Effectiveness of recommended visual acuity screening referral criteria in a population with a high prevalence of astigmatism: Contin Med Educ, 2006; 176(6); 1779-84
18. Stratford PW, Kennedy DM, Robarts SF, Modelling knee range of motion post arthroplasty: Clinical applications: Physiother Can, 2010; 62(4); 378-87
19. Jesús V, Raimundo J, David C, Visual function, performance, and processing of basketball players versus sedentary individuals: J Sport Health Sci, 2017; 87(9); 1-8
20. Yurova OV, Andjelova DV, Chayka AA, The influence of physical loads on the functional parameters of the eyes in the children and adolescents regularly engaged in sports activities: Vopr Kurortol Fiziot-er Lech Fiz Kult, 2017; 94(3); 44-48
21. Jacobsen N, Jensen H, Goldschmidt E, Does the level of physical activity in university students influence development and progression of myopia: Invest Ophthalmol Vis Sci, 2008; 49(4); 1322-27
Figures
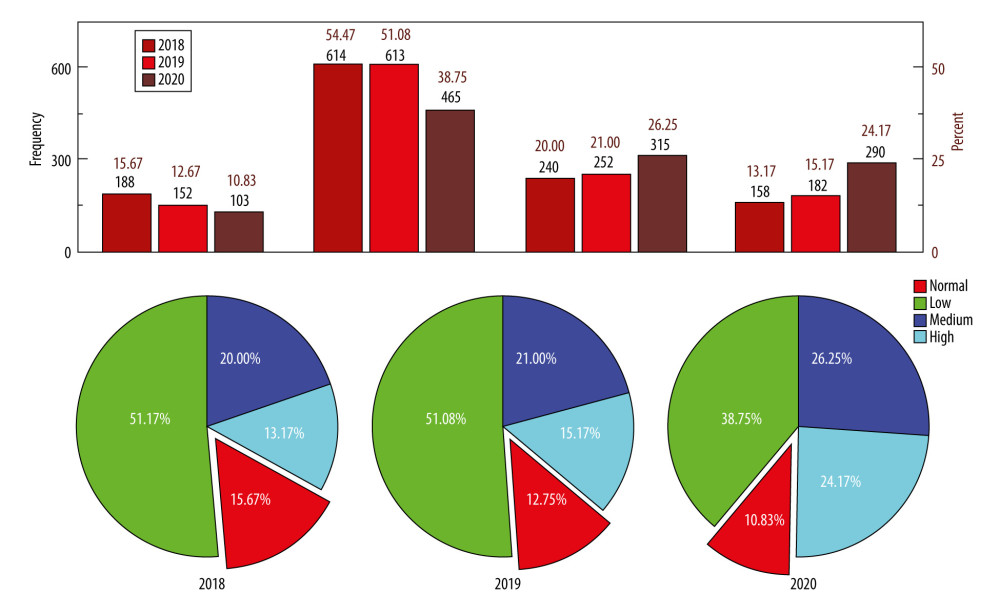 Figure 1. The distribution map of the level of college student’s eyesight for freshmen starting in 2018, 2019, and 2020 in China.
Figure 1. The distribution map of the level of college student’s eyesight for freshmen starting in 2018, 2019, and 2020 in China.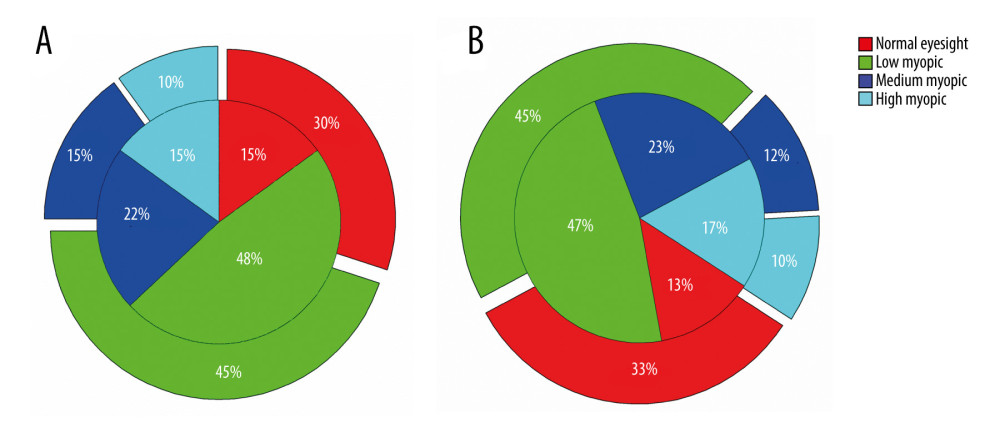 Figure 2. The distribution map of the level of college student’s eyesight in ball sports clubs in China. The inner and outer circles of the pie chart indicate the beginning and end of the school year, respectively. (A) Basketball clubs; (B) table tennis clubs.
Figure 2. The distribution map of the level of college student’s eyesight in ball sports clubs in China. The inner and outer circles of the pie chart indicate the beginning and end of the school year, respectively. (A) Basketball clubs; (B) table tennis clubs.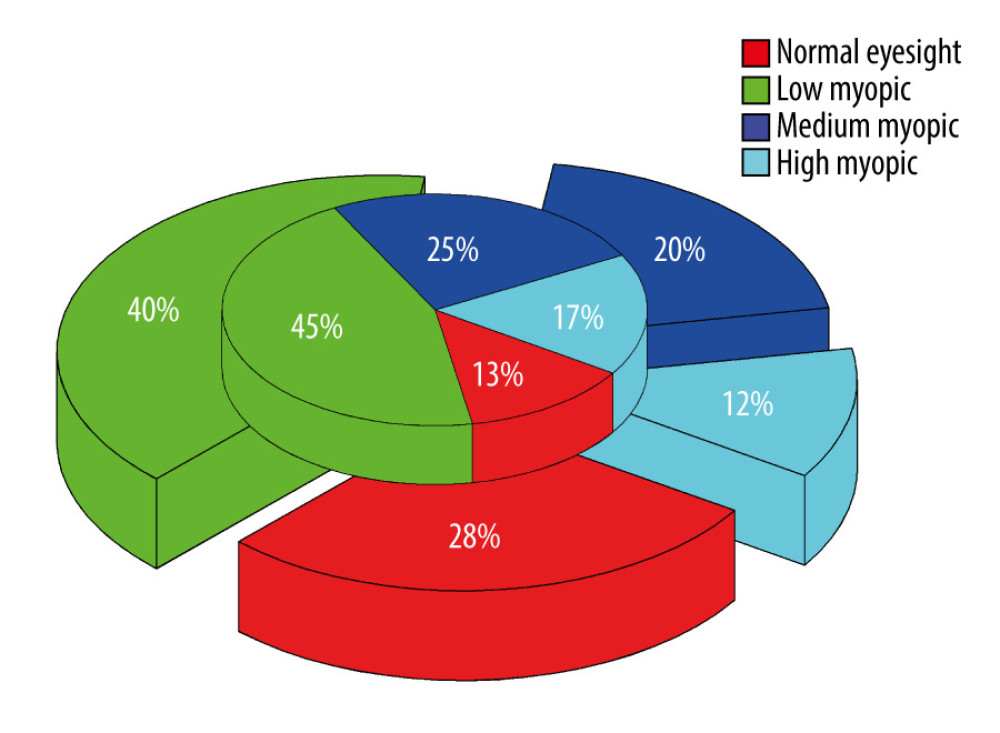 Figure 3. The distribution map of the level of college student’s eyesight of non-ball wushu sports clubs in China. The inner and outer circles of the pie chart indicate the beginning and end of the school year, respectively.
Figure 3. The distribution map of the level of college student’s eyesight of non-ball wushu sports clubs in China. The inner and outer circles of the pie chart indicate the beginning and end of the school year, respectively. Tables
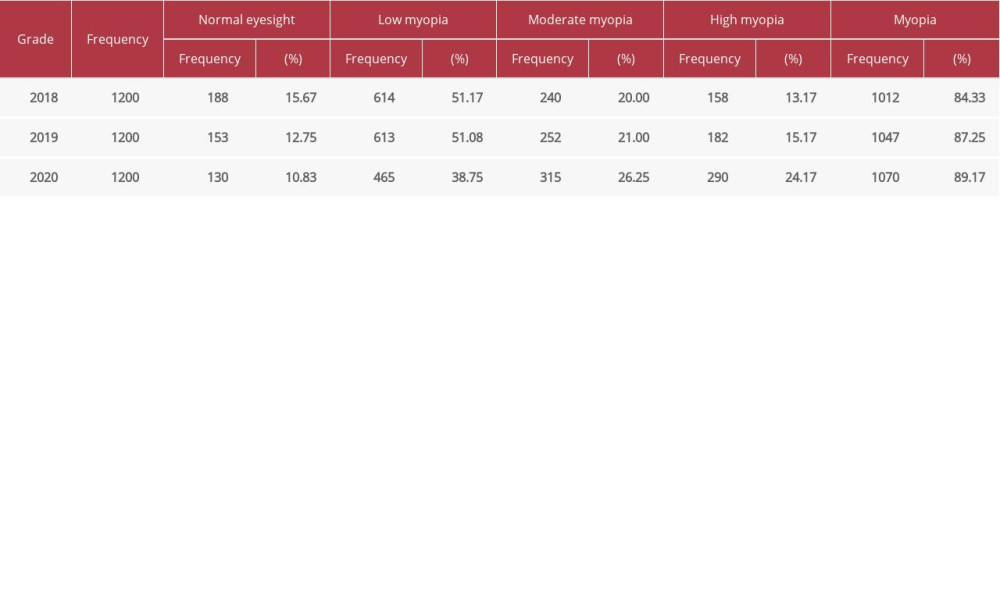 Table 1. Vision test results of freshmen classes starting in years 2018, 2019, 2020 (n=3600).
Table 1. Vision test results of freshmen classes starting in years 2018, 2019, 2020 (n=3600).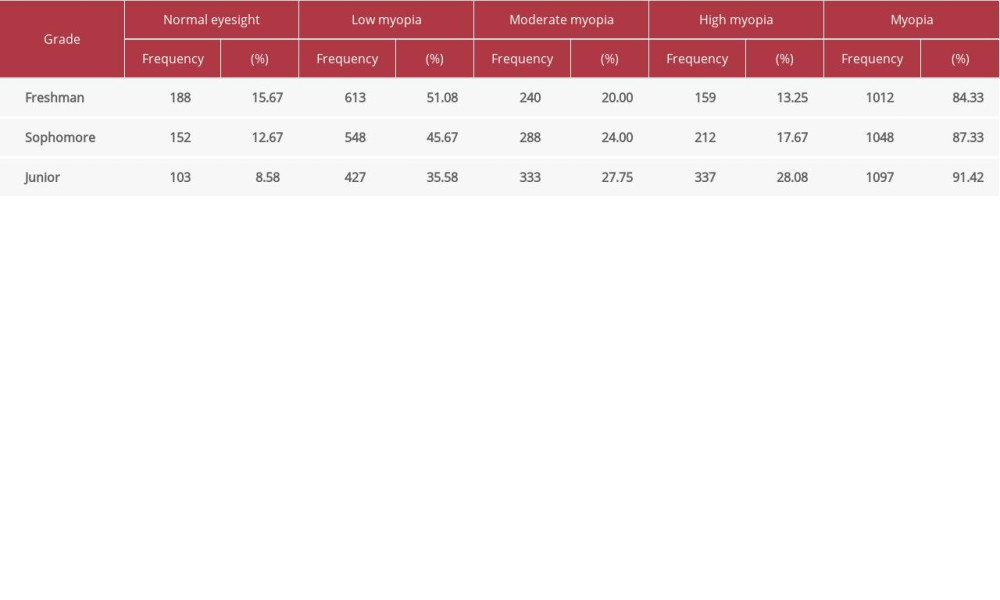 Table 2. Vision test results for the 3 consecutive academic years of the class starting in 2018 (n=1200).
Table 2. Vision test results for the 3 consecutive academic years of the class starting in 2018 (n=1200).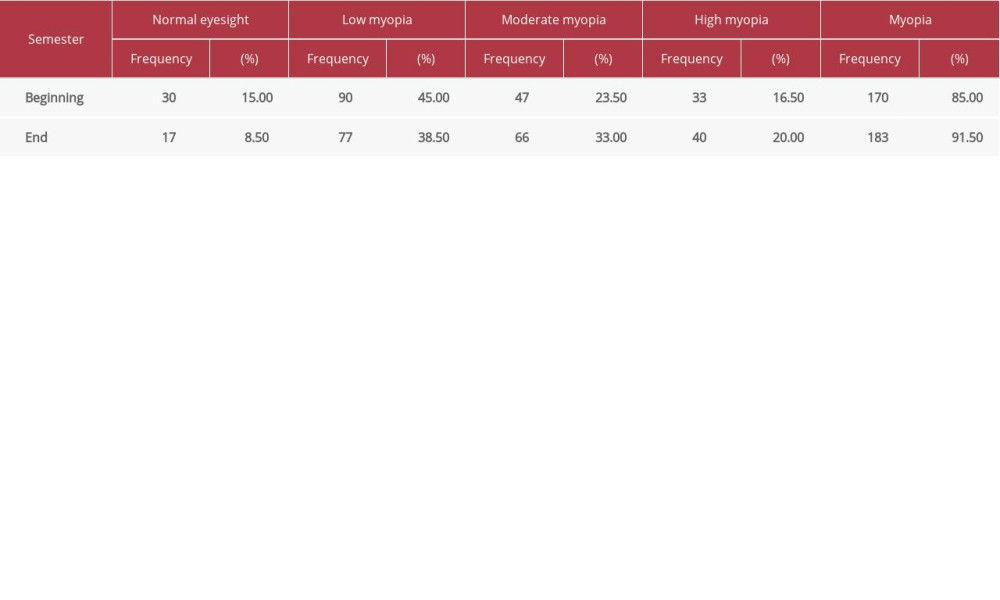 Table 3. Visual acuity test results of non-club members during the academic year for class starting 2019 (n=200).
Table 3. Visual acuity test results of non-club members during the academic year for class starting 2019 (n=200).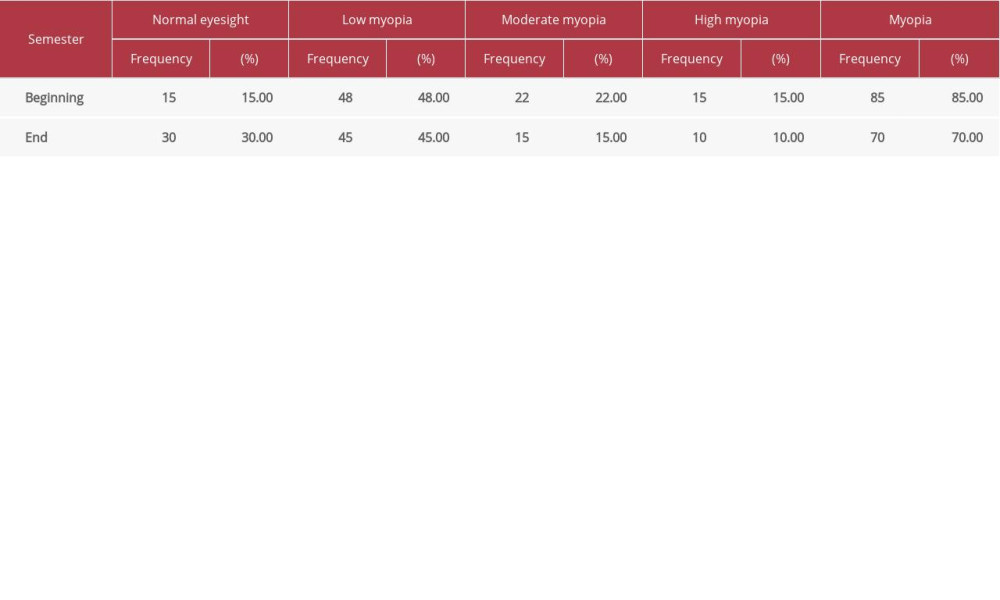 Table 4. Visual acuity test results for basketball club members during the 2019 academic year for class starting in 2018 (n=100).
Table 4. Visual acuity test results for basketball club members during the 2019 academic year for class starting in 2018 (n=100).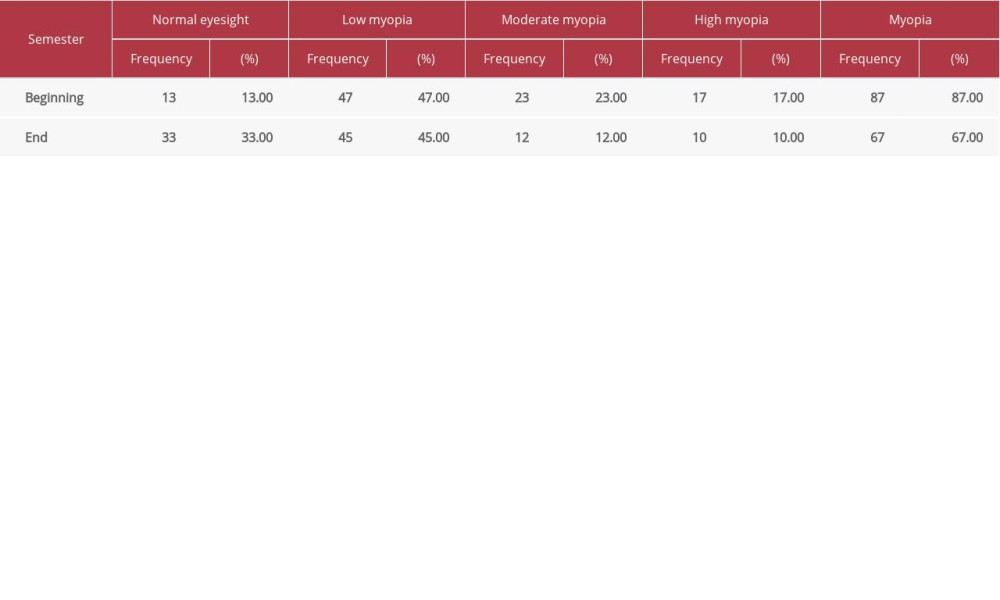 Table 5. Visual acuity test results for table tennis club members during the 2019 academic year for class starting in 2018 (n=100).
Table 5. Visual acuity test results for table tennis club members during the 2019 academic year for class starting in 2018 (n=100).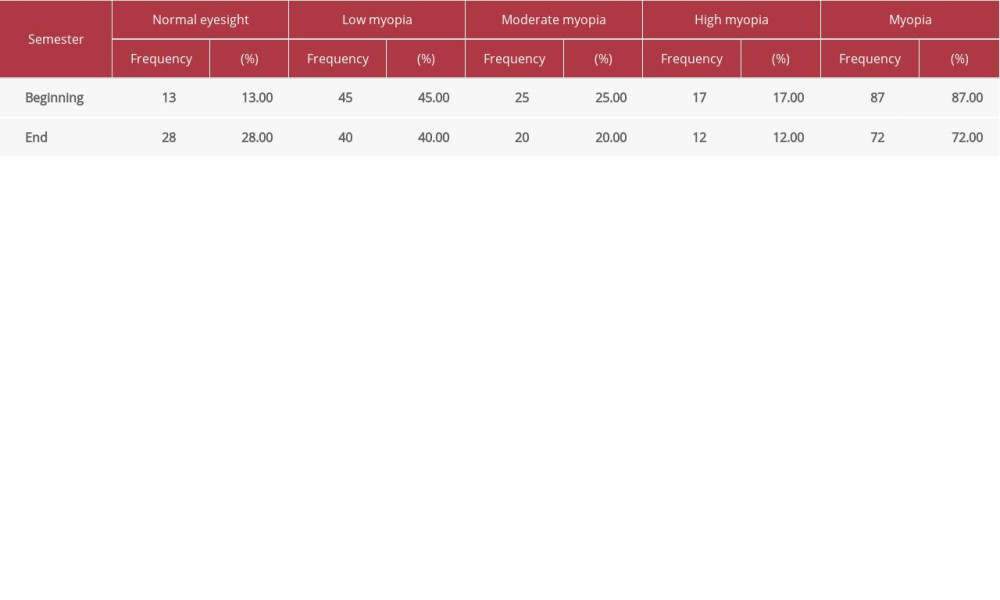 Table 6. Visual acuity test results for wushu club members during the 2019 academic year for class starting in 2018 (n=100).
Table 6. Visual acuity test results for wushu club members during the 2019 academic year for class starting in 2018 (n=100).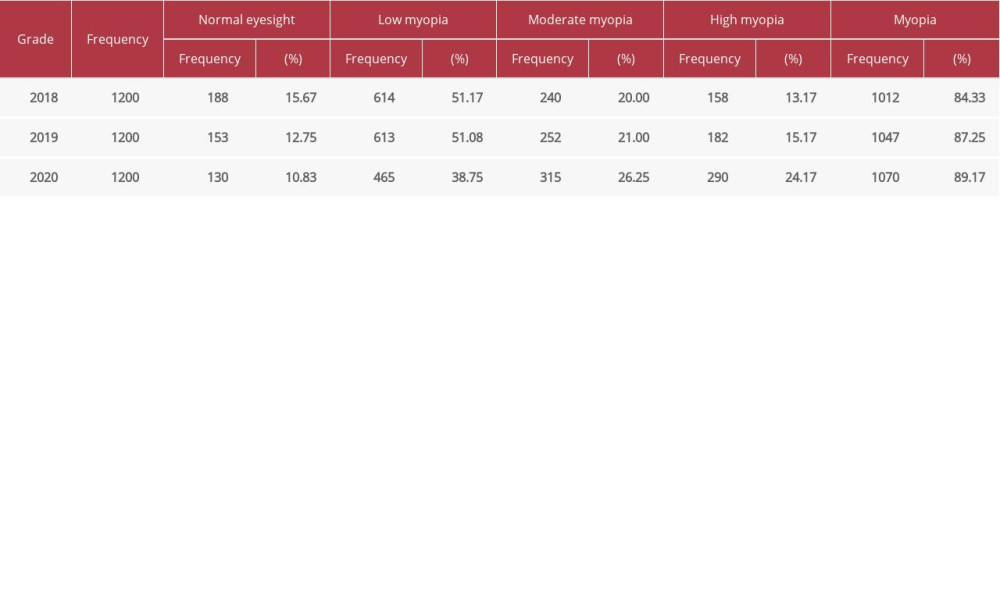 Table 1. Vision test results of freshmen classes starting in years 2018, 2019, 2020 (n=3600).
Table 1. Vision test results of freshmen classes starting in years 2018, 2019, 2020 (n=3600).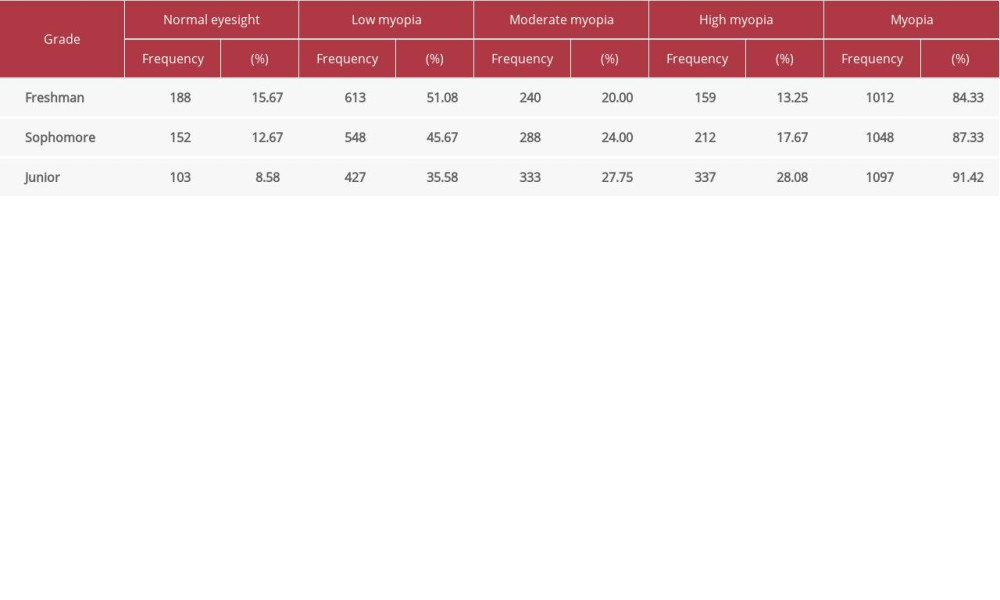 Table 2. Vision test results for the 3 consecutive academic years of the class starting in 2018 (n=1200).
Table 2. Vision test results for the 3 consecutive academic years of the class starting in 2018 (n=1200).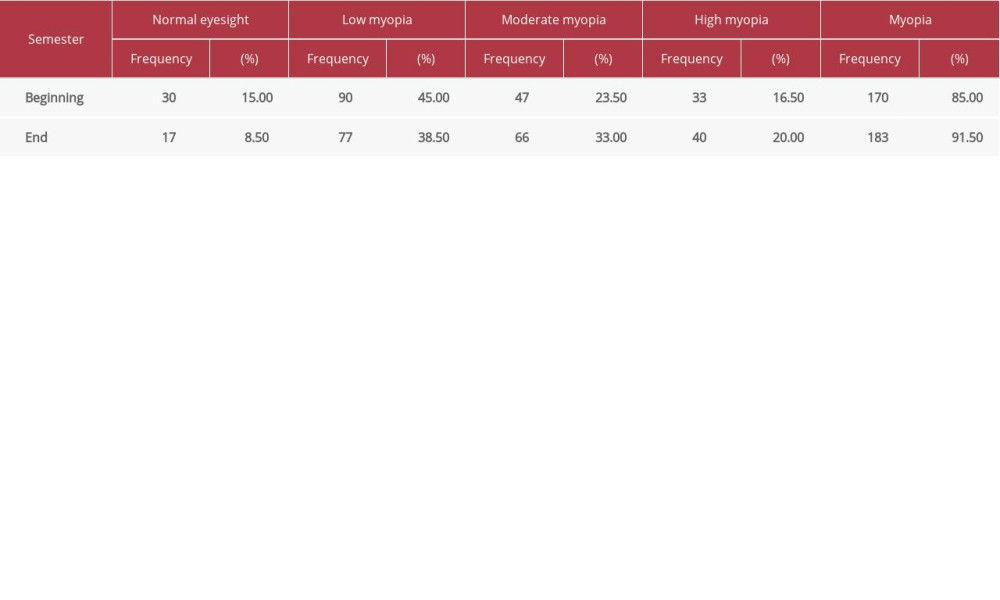 Table 3. Visual acuity test results of non-club members during the academic year for class starting 2019 (n=200).
Table 3. Visual acuity test results of non-club members during the academic year for class starting 2019 (n=200).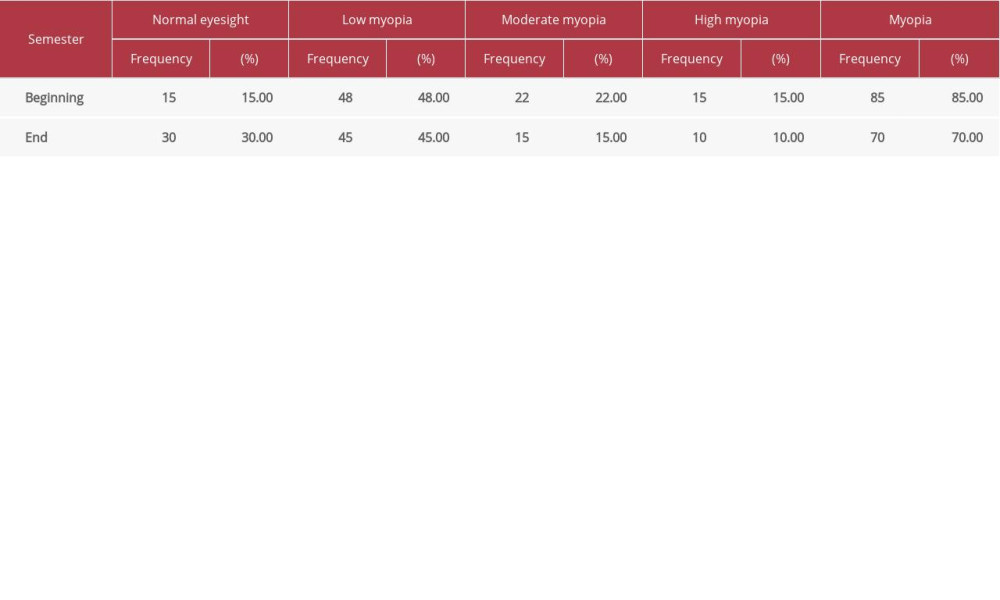 Table 4. Visual acuity test results for basketball club members during the 2019 academic year for class starting in 2018 (n=100).
Table 4. Visual acuity test results for basketball club members during the 2019 academic year for class starting in 2018 (n=100).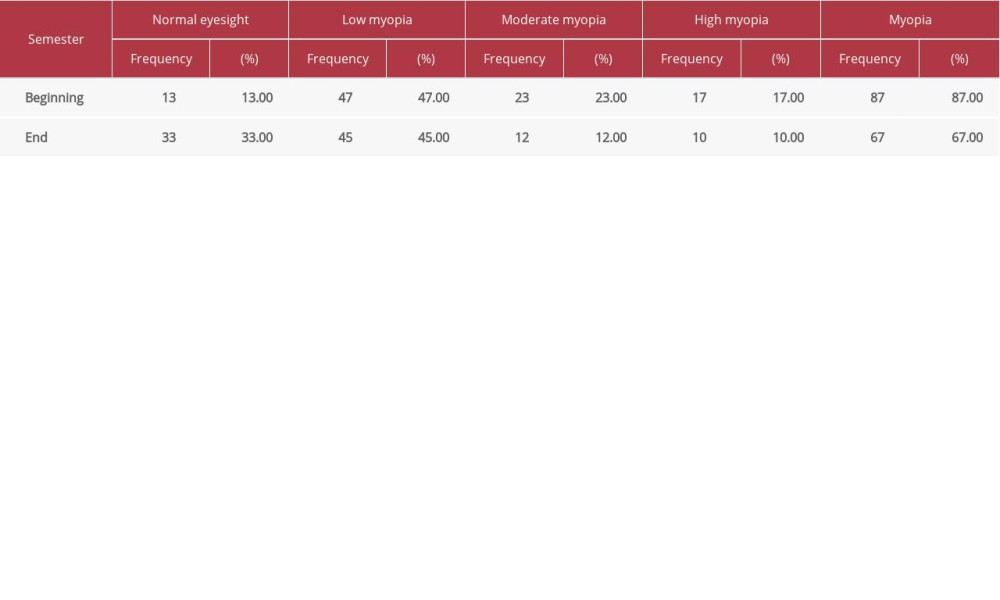 Table 5. Visual acuity test results for table tennis club members during the 2019 academic year for class starting in 2018 (n=100).
Table 5. Visual acuity test results for table tennis club members during the 2019 academic year for class starting in 2018 (n=100).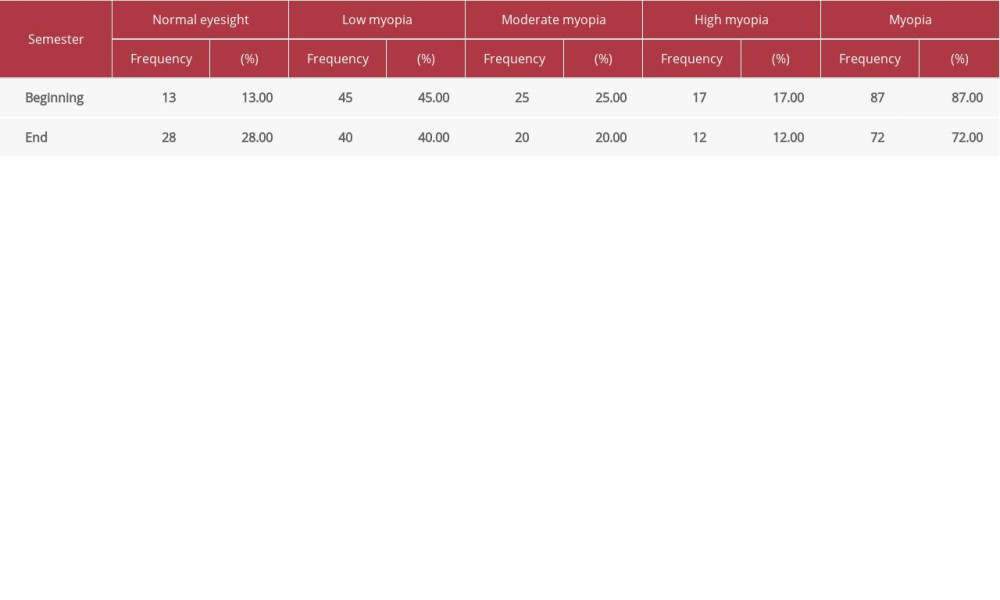 Table 6. Visual acuity test results for wushu club members during the 2019 academic year for class starting in 2018 (n=100).
Table 6. Visual acuity test results for wushu club members during the 2019 academic year for class starting in 2018 (n=100). Most Viewed Current Articles
15 Jun 2022 : Clinical Research
Evaluation of Apical Leakage After Root Canal Obturation with Glass Ionomer, Resin, and Zinc Oxide Eugenol ...DOI :10.12659/MSMBR.936675
Med Sci Monit Basic Res 2022; 28:e936675
07 Jul 2022 : Laboratory Research
Cytotoxicity, Apoptosis, Migration Inhibition, and Autophagy-Induced by Crude Ricin from Ricinus communis S...DOI :10.12659/MSMBR.936683
Med Sci Monit Basic Res 2022; 28:e936683
01 Jun 2022 : Laboratory Research
Comparison of Sealing Abilities Among Zinc Oxide Eugenol Root-Canal Filling Cement, Antibacterial Biocerami...DOI :10.12659/MSMBR.936319
Med Sci Monit Basic Res 2022; 28:e936319
08 Dec 2022 : Original article
Use of Estimated Glomerular Filtration Rate and Urine Albumin-to-Creatinine Ratio Based on KDIGO 2012 Guide...DOI :10.12659/MSMBR.938176
Med Sci Monit Basic Res 2022; 28:e938176