28 July 2022: Articles 
An Unusual Case of Primary Ileal Trichobezoar Causing Intussusception
Challenging differential diagnosis, Diagnostic / therapeutic accidents, Management of emergency care, Rare disease, Clinical situation which can not be reproduced for ethical reasons, Rare coexistence of disease or pathology
Mitchell M. Won1ABDEF, Marla A. Sacks2ABCDEF, Rebekah Leigh1EF, Yomara S. Mendez2EF, Laura F. Goodman3AEF, Edward Tagge2ADE, Andrei Radulescu2AEF*DOI: 10.12659/AJCR.935460
Am J Case Rep 2022; 23:e935460
Abstract
BACKGROUND: Intussusception, which is the prolapse of one section of intestine into another, is a common cause of small-bowel obstruction in pediatric patients. Bezoars are concretions of ingested foreign material. Trichobezoars, which are bezoars made of hair, occur in the context of trichotillomania, the compulsive pulling of hair, and trichophagia, the eating of hair. If gastric trichobezoars grow to sufficient size, an intestinal extension can serve as a lead point for intussusception to occur. Rarely, hair passes completely through the stomach and forms a trichobezoar within the small bowel. This obstruction can also create lead points and cause intussusception. This is one of the few reported cases of intussusception due to a primary intestinal bezoar.
CASE REPORT: We present the case of an 8-year-old boy with an unknown history of trichophagia and a preliminary diagnosis of appendicitis. Upon imaging, a bowel obstruction related to a small-bowel intussusception was discovered to be the probable cause. A diagnostic laparoscopy revealed an ileo-ileal intussusception caused by an ileal bezoar. Conversion to exploratory laparotomy assisted in removing the causative bezoar. The patient recovered without postoperative complications.
CONCLUSIONS: We report a case of an isolated intestinal trichobezoar causing intussusception in a boy. While intussusception secondary to a trichobezoar most commonly occurs due to ‘Rapunzel syndrome,’ this case shows that it is possible for an intestinal trichobezoar to form without the presence of ‘Rapunzel syndrome.’ This unique cause of intussusception presented as a small-bowel obstruction, requiring evacuation of the bezoar.
Keywords: Bezoars, Intussusception, Pediatric Emergency Medicine, Child, Humans, Intestinal Obstruction, Male, Stomach, trichotillomania
Background
Intussusception occurs when part of the intestine prolapses into an adjacent segment [1]. Sometimes described as a ‘telescoping’ action [2,3], a lead point in the proximal bowel (intussusceptum) is caught and carried by peristalsis into the distal bowel (intussuscipiens), squeezing and compressing the mesenteric vessels [1]. This leads to the classic tetrad of signs and symptoms: colicky abdominal pain, vomiting, ‘red currant jelly’ stools, and a palpable mass [1]; however, all 4 signs present together infrequently and late in the disease course [4]. Ultimately, ischemia of the bowel leads to necrosis, perforation, and peritonitis if untreated [1].
Bezoars are masses of ingested foreign material [5]. Nomenclature of the bezoar depends on the constitution of the mass: phytobezoars are made up of plant material, pharmacobezoars are from medications, and trichobezoars are from hair [5]. Bezoars may be asymptomatic, but can present with symptoms of mass effect such as gastric pain, early satiety, nausea, and vomiting [6]. While the majority occur in the stomach [7], bezoars infrequently form in the small intestine [5], and rarely present in the colon [8]. Intestinal bezoars can present with symptoms of small-bowel obstruction, which can ultimately lead to perforation if not diagnosed and treated urgently [5].
Of the various bezoar compositions, trichobezoars are the most common [5,9]. Trichophagia, the consumption of hair, is associated with trichotillomania, the compulsive pulling of hair [10]. Trichotillomania most commonly presents in the pediatric population, with a large female predominance between the ages of 9 and 13 years [11]. Trichobezoars have been reported to develop secondarily to trichotillomania in up to 38% of patients [12], as trichobezoars are far more likely to occur in people that pick at and consume their hair.
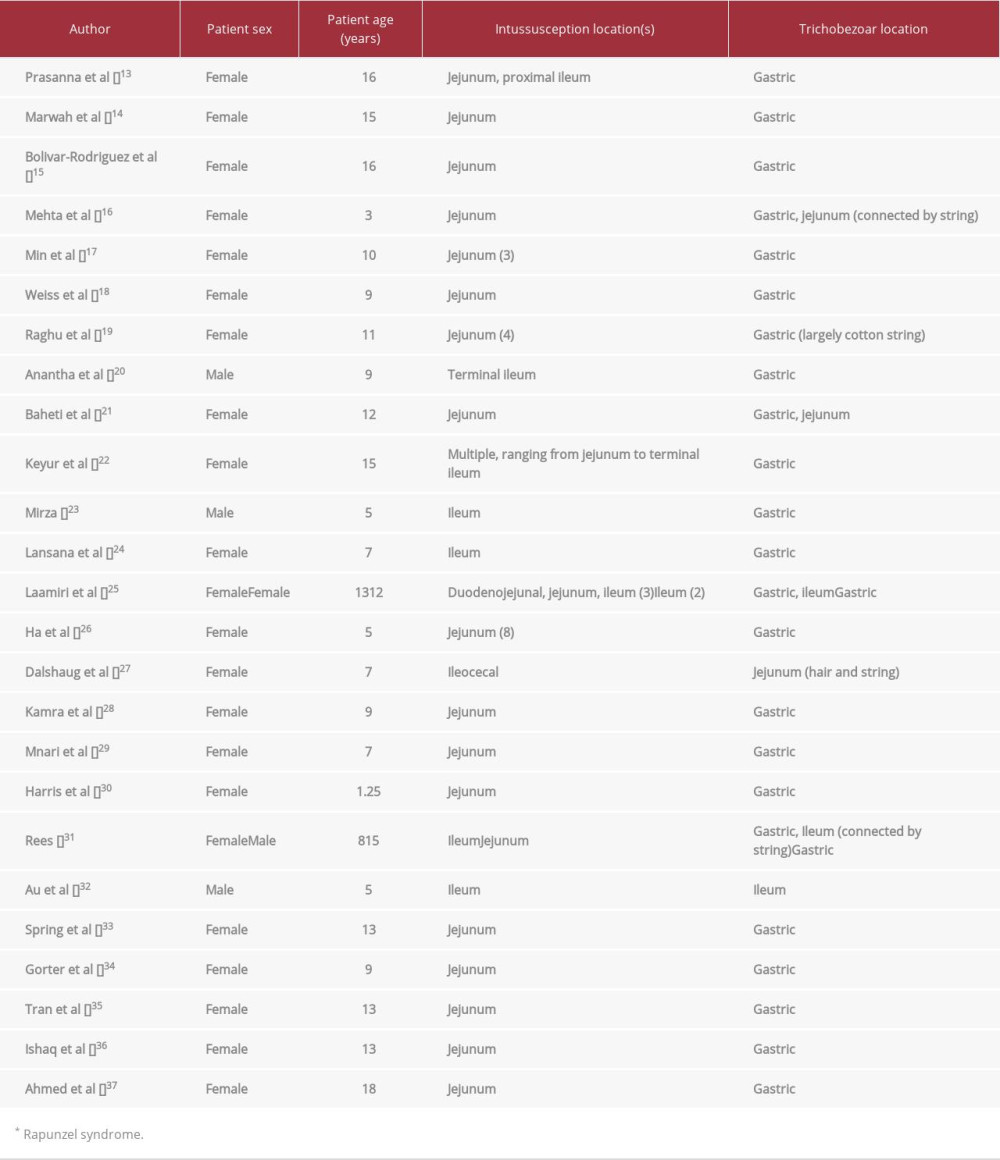
Trichobezoars have been well-documented as a source of a pathological lead point, and thus a cause of intussusception in children [5–7,9,13–38]. In the majority of cases, ‘Rapunzel syndrome’ was identified (Table 1). ‘Rapunzel syndrome,’ first named by Vaughen et al in 1968 [38], occurs when a gastric trichobezoar forms a tail which extends beyond the pyloric sphincter. A tail of sufficient size can catch on the intestinal wall and serve as a lead point for intussusception to occur, as normal peristalsis carries the tail and the entrapped wall further down into the intestine [20]. Less commonly, trichobezoars form in the intestines and cause intussusception [27,32].
This report documents an 8-year-old boy with a history of trichophagia who presented with ileal intussusception due to a primary intestinal trichobezoar, with no associated gastric trichobezoar or ‘Rapunzel syndrome’ apparent.
Case Report
This patient was a previously healthy 8-year-old boy with no significant history, who was transferred to our Emergency Department (ED) for workup of abdominal pain with a primary suspected diagnosis of appendicitis. The morning prior to presentation, the patient had emesis associated with abdominal pain. Recurrent episodes continued throughout the day. At an outside hospital, an abdominal ultrasound (US) showed a 2-cm mass with inflammation in the right lower quadrant (Figure 1).
Initial laboratory findings showed an elevated white blood cell (WBC) count of 21 800 cells/µL. This imaging study was followed by an abdominal computed tomography (CT) to better characterize the right lower-quadrant mass seen on ultrasound. This CT demonstrated evidence of a high-grade small-bowel obstruction, ‘telescoping’ or ‘swirling’ bowel, and a normal appendix (Figures 2, 3).
Due to the characteristics of the obstructed bowel, there was a high index of suspicion for ileo-ileal intussusception or an internal hernia. The decision was made to proceed with a diagnostic laparoscopy, informed consent was obtained, and the patient was prepared for surgery. Upon entry into the perito-neal cavity, a small-bowel intussusception was noted in the right lower quadrant and was easily reduced laparoscopically. Upon further inspection, a secondary site of small-bowel intussusception was found and the decision was made to convert to laparotomy (Figure 3).
After the bowels were eviscerated from the wound, a large obstructing bezoar was found, limited to the mid-small bowel. A longitudinal antimesenteric enterotomy was performed and the bezoar was removed (Figure 4).
The bowel was inspected to confirm complete removal of the bezoar, and the enterotomy was closed transversely. The abdomen was irrigated and closed in layers in a standard fashion.
Postoperative psychiatric evaluation revealed a history of trichophagia, as the patient had been observed to eat hair off the ground or off combs. He was discharged 6 days after surgery with no complications. The patient was seen in the clinic for follow-up at 2 weeks after the operation. He was healing well from the surgery without wound issues, returned to regular activity, and his hair had been shaven to avoid trichophagia. Both the mother and patient were satisfied with the surgery and postoperative outcome.
Discussion
Trichobezoar-associated intussusception is commonly associated with ‘Rapunzel syndrome’, but ‘Rapunzel syndrome’ is not mandatory for intussusception to occur. A PubMed® literature review using the keywords “bezoar,” “trichobezoar,” and “intussusception” revealed 26 cases of intussuscepted pediatric patients with trichobezoars acting as lead points. In all but 4 of these cases, ‘Rapunzel syndrome’ was identified as the etiology of intussusception.
The overwhelming majority of cases occurred in female patients, with 3 not experiencing ‘Rapunzel syndrome’ (Table 1). Male patients experienced a secondary intussusception far less often than female patients, representing only 4/24 cases. Despite this, ‘Rapunzel syndrome’ was still present in the majority of male cases, with only 1 not presenting with the syndrome [20,23,31,32].
The lower incidence of intussusception secondary to trichobezoar in boys may be associated with the shorter average length of male hair. The only other patient experiencing intussusception secondary to a primary intestinal bezoar was another male, as seen in the case report of Au et al [32]. Shorter hairs may discourage the development of ‘Rapunzel syndrome’, as the hairs are more likely to pass through the pyloric sphincter completely and collect in the small intestine. Primary intestinal bezoars may also be less likely to cause intussusception, as the lack of an anchoring gastric mass and tail creates a less mechanically favorable environment for the development of a lead point.
Although all case reports document the symptoms of abdominal pain, nausea, and vomiting, patient presentation varies greatly. Onset of abdominal pain can vary from 12 months prior [17] to the day before hospitalization [27]. Obstructive symptoms, such as constipation, obstipation, and distention, are present in some cases [15,16,21,23,28,32,37], but diarrhea is also possible [18,27]. A physical exam may be helpful in determining the location of the trichobezoar, as patients experiencing ‘Rapunzel syndrome’ often had a palpable abdominal mass [13,14,17–21,25,26,28,37], while patients without ‘Rapunzel syndrome’ did not [27,32].
Imaging of ‘Rapunzel syndrome’ is helpful in diagnosis, as the gastric trichobezoar accrues a large mass before the tail reaches a sufficient size to cause intussusception. This results in the CT scan finding of a heterogeneous mass occupying a dilated gastric chamber, described as a ‘beehive pattern’ by Bolivar-Rodriguez et al [15]. Abdominal radiography and ultrasound have also been used to successfully diagnose ‘Rapunzel syndrome’, but CT is preferred due to its higher specificity [39]. Diagnosing intussusception secondary to trichobezoar without ‘Rapunzel syndrome’ presents more difficulty, as endoscopy will not reveal the source of obstruction, and the smaller intestinal trichobezoar may be mistaken for feces [40]. Laparotomy was the intervention of choice for removal of the trichobezoar and reduction of intussusception in all reviewed cases, but a laparoscopic approach has been successful in treatment of ‘Rapunzel syndrome’ without intussusception [41].
Other case reports of pediatric intussusception secondary to trichobezoar in the absence of ‘Rapunzel syndrome’ share similarities with our patient. Dalshaug et al [27] documented a previously healthy 7-year-old girl with an initial diagnosis of viral gastroenteritis. She presented with no leukocytosis, and vomiting was bilious, rather than nonbilious, due to the location of the trichobezoar body in the duodenum [27]. The size and length of the trichobezoar also suggest that a non-gastric ‘Rapunzel syndrome’ may have occurred, with the main duodenal mass anchoring the obstructing tail at the ileocecal junction [27]. Au et al [32] described a case that also shares common features with our patient’s presentation; this 5-year-old boy presented with a 3-day history of abdominal pain and nonbilious vomiting, but this case was also associated with obstipation. Although this patient had a significantly different medical history, diagnosed with both failure to thrive and fecal impaction 1 year prior, the location of the obstructing bezoar was also the ileum [32].
Trichobezoars do not always have uniform composition. Four cases were significant for the presence of inorganic material within the trichobezoar, similar to our patient. Two of these cases were not associated with trichotillomania; Raghu et al [19] noted that the patient had a 10-year history of pica, specifically the threads from clothing, while Rees [31] did not report a significant history. Our patient had been observed to chew on hair and string he found while outside or around the house. Absence of trichotillomania in the patient history does not preclude the presence of a trichobezoar, as one can form through consumption of environmental hair, string, or fibers [9].
Conclusions
Isolated intestinal trichobezoars are a rare cause of intussusception in pediatric patients. Even though a gastric bezoar with an intestinal extension is the most common etiology, lack of a gastric mass does not eliminate trichobezoar as the source of bowel obstruction. Patient exam and history will not always have signs of trichotillomania, as patients may consume hair from their surroundings or environmental fibers.
Figures
References:
1.. Columbani PM, Scholz S, Intussusception: Pediatric Surgery, 2012; 1093-110, Elsevier Saunders
2.. Edwards EA, Pigg N, Courtier J, Intussusception: Past, present and future: Pediatr Radiol, 2017; 47(9); 1101-8
3.. Binkovitz LA, Kolbe AB, Orth RC, Pediatric ileocolic intussusception: New observations and unexpected implications: Pediatr Radiol, 2019; 49(1); 76-81
4.. Lai AHM, Phua KB, Teo ELHJ, Jacobsen AS, Intussusception: A three-year review: Ann Acad Med Singapore, 2002; 31(1); 81-85
5.. Rabine JC, Nostrant TT, Gastric bezoars: Textbook of Gastroenterology, 2003; 1461-63, Lippincott Williams & Wilkins
6.. Byrne WJ, Foreign bodies, bezoars, and caustic ingestion: Gastrointest Endosc Clin N Am, 1994; 4(1); 99-119
7.. Iwamuro M, Okada H, Matsueda K, Review of the diagnosis and management of gastrointestinal bezoars: World J Gastrointest Endosc, 2015; 7(4); 336-45
8.. Agha FP, Nostrant TT, Fiddian-Green RG, “Giant colonic bezoar”: A medication bezoar due to psyllium seed husks: Am J Gastroenterol, 1984; 79(4); 319-21
9.. Mehra A, Avasthi A, Gupta V, Grover S, Trichophagia along with trichobezoar in the absence of trichotillomania: J Neurosci Rural Pract, 2014; 5(Suppl. 1); S055-57
10.. Grant JE, Odlaug BL, Clinical characteristics of trichotillomania with trichophagia: Compr Psychiatry, 2008; 49(6); 579-84
11.. Sah DE, Koo J, Price VH, Trichotillomania: Dermatol Ther, 2008; 21(1); 13-21
12.. Bhatia MS, Singhal PK, Rastogi V, Clinical profile of trichotillomania: J Indian Med Assoc, 1991; 89(5); 137-39
13.. Prasanna BK, Rapunzel syndrome: A rare presentation with multiple small intestinal intussusceptions: World J Gastrointest Surg, 2013; 5(10); 282
14.. Marwah S, Pandey S, Raj A, Rapunzel syndrome presenting as jejuno-jejunal intussusception: Clin J Gastroenterol, 2015; 8(4); 202-6
15.. Bolívar-Rodríguez MA, Fierro-López R, Pamanes-Lozano A, Surgical outcome of jejunum-jejunum intussusception secondary to Rapunzel syndrome: A case report: J Med Case Rep, 2018; 12(1); 362
16.. Mehta MH, Patel R V, Intussusception and intestinal perforations caused by multiple trichobezoars: J Pediatr Surg, 1992; 27(9); 1234-35
17.. Min KJ, Tchah H, Kim SM, Choi JY, A rare presentation of Rapunzel syndrome with multiple small bowel intussusceptions: Pediatr Emerg Med J, 2019; 6(1); 17-20
18.. Weiss M, Danoff DM, Wood BP, Radiological case of the month: Arch Pediatr Adolesc Med, 1998; 152(4); 403-4
19.. Raghu V, Nagadi AN, Kumar AC, Rapunzel syndrome and small bowel intussusceptions due to a cotton thread bezoar: A case report: J Gastrointest Abdom Radiol, 2018; 1(1); 56-59
20.. Anantha RV, Chadi SA, Merritt N, Trichobezoar causing intussusception: Youngest case of Rapunzel syndrome in a boy in North America: J Pediatr Surg Case Reports, 2013; 1(1); e11-13
21.. Baheti AD, Otjen JP, Phillips GS, A hairy situation: trichobezoar presenting with intussusception, and intestinal and biliary perforation in a child: Radiol Case Reports, 2017; 12(1); 42-44
22.. Keyur B, Dhaval M, Daxa K, The longest trichobezoar (59 in.) presented with gastric perforation and multiple small bowel intussusceptions – a unique presentation: Indian J Surg, 2021; 83; 1083-85
23.. Mirza B, Rapunzel syndrome presenting with ileo-ileal intussusception in a boy: J Surg Pakistan, 2011; 16(3); 130-32
24.. Lansana C, Abdoulaye Korse B, Soriba Naby C, Gastrointestinal trichobezoar revealed by intussusception at the University Hospital of Conakry: J Surg, 2021; 9(1); 27
25.. Laamiri R, Kechiche N, Mnari W, Gastrointestinal trichobezoar causing atypical intussusception in a child: Report of two cases: J Pediatr Sci, 2016; 8; 214
26.. Ha SC, Koh CC, Lee CH, A rare case of Rapunzel syndrome with multiple small bowel intussusceptions and bowel obstruction: Formos J Surg, 2016; 49(2); 67-69
27.. Dalshaug GB, Wainer S, Hollaar GL, The Rapunzel syndrome (Trichobezoar) causing atypical intussusception in a child: A case report: J Pediatr Surg, 1999; 34(3); 479-80
28.. Kamra H, Munde SL, Kaur S, Rapunzel syndrome – Trichobezoar in a 9-year-old girl: A case report: J Krishna Inst Med Sci Univ, 2015; 4(3); 113-15
29.. Mnari W, Maatouk M, Hmida B, [Rapunzel syndrome with multiple small-bowel intussusceptions: An unusual association of trichobezoar.]: Arch Pediatr, 2016; 23(6); 629-31 [in French]
30.. Harris VJ, Hanley G, Unusual features and complications of bezoars in children: Am J Roentgenol, 1975; 123(4); 742-45
31.. Rees M, Intussusception caused by multiple trichobezoars: A surgical trap for the unwary: Br J Surg, 1984; 71(9); 721
32.. Au VA, Wong JP, Venu I, Failing to thrive, abdominal pain and vomiting: A hairy situation: Paediatr Child Health, 2018; 23(3); 173-75
33.. Spring S, Anderson R, Carlson JN, 13-year-old with cryptic abdominal pain: West J Emerg Med, 2015; 16(1); 149-50
34.. Gorter RR, Kneepkens CMF, Mattens ECJL, Management of trichobezoar: Case report and literature review: Pediatr Surg Int, 2010; 26(5); 457-63
35.. Tran LT, Dorsey JT, S3092 “Rapunzel, Rapunzel, where is your long, beautiful hair?”: A case report of Rapunzel syndrome: Am J Gastroenterol, 2021; 116(1); S1276
36.. Ishaq N, Khaleeq T, Rapunzel syndrome – a case report: Trichobezoar as a cause of gastric outlet obstruction and intestinal perforation: Dubai Med J, 2022; 5; 122-24
37.. Ahmed MM, Tahir KS, Gubari MIM, Large trichobezoar associated with misdiagnosis, a rare case report with a brief literature review: Int J Surg Case Rep, 2021; 88; 106551
38.. Vaughan ED, Sawyers JL, Scott HW, The Rapunzel syndrome. An unusual complication of intestinal bezoar: Surgery, 1968; 63(2); 339-43
39.. Ho TW, Koh DC, Small-bowel obstruction secondary to bezoar impaction: A diagnostic dilemma: World J Surg, 2007; 31(5); 1072-78 ; discussion 1079–80
40.. Gayer G, Jonas T, Apter S, Bezoars in the stomach and small bowel – CT appearance: Clin Radiol, 1999; 54(4); 228-32
41.. Palanivelu C, Rangarajan M, Senthilkumar R, Madankumar MV, Trichobezoars in the stomach and ileum and their laparoscopy-assisted removal: A bizarre case: Singapore Med J, 2007; 48(2); e37-39
Figures
In Press
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942864
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250