03 May 2022: Original Paper
Outcomes of Split Liver Transplantation vs Living Donor Liver Transplantation in Pediatric Patients: A 5-Year Follow-Up Study in Korea
Kyung Chul Yoon12ABCDEF, Sanghee Song3BC, Sanghoon Lee4BC, Ok-Kyung Kim3BC, Suk Kyun Hong1BC, Nam-Joon Yi1ABCDEF, Jong Man Kim4BCD, Kwang-Woong Lee1ABCD, Myoung Soo Kim5BCD, YoungRok Choi1BCD, Kyung-Suk Suh1ABCD, Suk-Koo Lee4ACDEF*DOI: 10.12659/AOT.935682
Ann Transplant 2022; 27:e935682
Abstract
BACKGROUND: The number of pediatric patients awaiting liver transplantation has decreased. Due to its increased use in Korea, split liver transplantation (SLT) may be a substitute for living donor liver transplantation (LDLT); however, the outcomes of pediatric SLT and LDLT in Korea remain unreported.
MATERIAL AND METHODS: We reviewed data of Korean patients aged <18 years who received SLT from 2005 to 2014, based on the Korea national database and compared to recipients who underwent LDLTs at Seoul National University Hospital during the same period.
RESULTS: A total of 63 and 56 patients were included in SLT and LDLT, respectively. The most common indication for LT was biliary atresia (60.3% in SLT vs 67.9% in LDLT). The Pediatric End-Stage Liver Disease score did not differ between the groups (P>0.05). The 1-, 3-, and 5-year overall survival rates were 92.1%, 90.2%, and 86.6% in the SLT and 96.4%, 94.6%, and 94.6% in the LDLT groups, respectively (P=0.21); the corresponding graft survival rates were 88.9%, 87.1%, and 83.6% in the SLT and 92.9%, 91.0%, and 91.0% in the LDLT groups, respectively (P=0.31). Fulminant hepatic failure was a risk factor for graft failure [OR, 8.77 (1.08-70.92); P=0.042], but not overall survival [OR, 11.78 (0.56-247.29); P=0.11].
CONCLUSIONS: The graft and overall survival rates of SLT and LDLT were not different in pediatric patients in Korea, and fulminant hepatic failure was the only risk factor affecting graft survival outcomes.
Keywords: Liver Transplantation, Living Donors, Unrelated Donors, Child, End stage liver disease, Follow-Up Studies, Humans, Liver Failure, Acute, Republic of Korea, Severity of Illness Index
Background
An increase in the number of deceased donor liver transplantations (DDLTs) usually accompanies a decrease in the number of living donor liver transplantations (LDLTs) in the annual report of both the scientific registry of transplant recipients (SRTR) and the European liver transplant registry (ELTR) [1,2]. According to the Korean Network for Organ Sharing (KONOS) data, the number of deceased donors has recently increased in Korea (Figure 1A) (www.KONOS.go.kr). Additionally, compared with adult candidates, there is a relatively small number of pediatric candidates on the liver transplantation (LT) waiting list (<1%) in Korea. The annual number of pediatric LTs is less than 70, and the proportion of pediatric LTs is approximately 5% (Figure 1B); between January 2005 and December 2014, the total number of LTs was 9934, including 541 pediatric LTs (5.4%).
Among DDLTs, split liver transplantation (SLT) is a highly feasible option to overcome the organ shortage, especially in pediatric LT candidates [1,3–6]. Therefore, the number of pediatric SLTs has been increasing in Korea (Figure 1C). However, SLT is regarded as a marginal graft compared with LDLTs in pediatric LT patients or whole-liver DDLT in both adult and pediatric patients [7,8]. Even in highly selected deceased organ donors, there is considerable debate regarding the poor outcomes of pediatric SLT compared with those of LDLT or whole-liver DDLT due to the longer ischemic time, genetic irrelevances, and inadequate volume of the graft [1,3–6]. The number of SLTs has recently increased, especially in pediatric patients in Korea; however, the outcomes have not yet been reported. Therefore, we aimed to investigate the outcomes of pediatric SLT with a left lateral section graft using the Korean national database. The outcomes of pediatric SLT were compared with those of pediatric LDLT using the same graft in a single large-volume LDLT center.
Material and Methods
SLT POLICY IN KOREA:
The deceased donor’s liver is allocated to a recipient on the waiting list by the KONOS system according to the patient’s urgency status, donor-to-recipient weight ratio (>0.5 and <2), and blood type. The KONOS status is similar to the United Network for Organ Sharing status, which was used in Korea before the model for end-stage liver disease scoring-based system. Status 1 has highest priority in case of fulminant hepatic failure of acute graft failure within 7 days after liver transplantation. Status 2A is defined as patients with chronic liver disease who had Child-Turcotte-Pugh (CTP) score higher than 10 and who meet medical criteria (variceal bleeding requiring blood transfusion, ascites or hydrothorax more than 4 liters a week, and spontaneous bacterial peritonitis). Status 3 is defined as patients who had a CTP score more than 7 without meeting the 2B criteria. The splitting criteria were previously introduced in detail, and were applied considering donor characteristics (age, body weight, and hemodynamic stability), less use of inotropics, and recipient characteristics [8]. If the deceased donor’s health condition is found suitable for SLT, the KONOS system allocates both an adult and pediatric candidate as SLT recipients. Although there are no specific inclusion or exclusion criteria regarding how to become an SLT candidate for adults, pediatric recipients are allocated according to specific criteria. KONOS policies for designating an SLT do not include a category for graft biopsy or anatomical variation of a graft; this policy for splitting was changed and broadened in January 2014, while the criteria for recipients were revised in January 2013.
SPLIT PROCEDURE FOR A LEFT LATERAL SECTION GRAFT IN KOREA:
An in situ split technique similar to LDLT is usually performed for SLT in Korea [8,9]. In a left lateral section graft, the left hepatic and portal veins, left and middle hepatic arteries, and left bile duct are preserved. A right trisection graft usually preserves the inferior vena cava (including the right and middle hepatic vein), celiac axis, main portal vein, and common bile duct. Regarding hepatic artery division, the left and middle hepatic arteries were preserved and reconstructed for left-sided liver grafts in SLTs. Although uncommon, an aberrant segmental artery for segment 2 or 3 may have developed from the middle hepatic artery. The middle hepatic artery is important for monosegment LT in small children, especially those undergoing SLT without preoperative donor images. In cases of replaced left hepatic artery variation, back-table reconstruction is performed. The bile duct division depends on the surgeon’s preferences, using cholangiography or only proving and division. These split procedures are counterpart descriptions of a previous right trisection graft study [8].
STATISTICAL ANALYSIS:
SPSS version 22.0 for Windows (IBM Corp., Armonk, NY, USA) was used to perform data analysis. The chi-square test was performed for categorical variables, and the
ETHICS APPROVAL:
This study followed the ethical guidelines of the Declaration of Helsinki and was approved by the Institutional Review Board of Seoul National University Hospital (Institutional Review Board no. 1708-025-875).
Results
DEMOGRAPHICS:
Table 1 shows the demographics of donors and recipients in the SLT and LDLT groups. The LDLT group had more recipients aged <1 year than the SLT group (LDLT, 63.5% vs SLT, 40.4%); however, the median age was not different between the 2 groups. Body weight was greater in the LDLT group than in the SLT group [median: LDLT, 14.6 (10.2–25.4) vs SLT, 10.0 (7.2–13.0); P<0.01], and the number of patients weighing <10 kg was higher in the SLT group (54.0%) than in the LDLT group (23.2%; P<0.01). The most common indication was biliary atresia, with similar proportions observed in both groups (SLT, 60.3% vs LDLT, 67.9%). The Pediatric End-Stage Liver Disease score [SLT, 15.5±12.1 vs LDLT, 16.2±13.7; P=0.76] and graft weight (g) [SLT, 345 (283–410) vs LDLT, (297–368); P=0.69] were not significantly different between the groups. The total ischemic time (minutes) was longer in the SLT group (256±163) than in the LDLT group (102±40; P<0.01), the graft-recipient weight ratio (GRWR,%) was greater in the SLT group (3.83±1.7) than in the LDLT group (2.44±1.36; P<0.01), and the mean follow-up period (months) was longer in the LDLT group (74±40) than in the SLT group (44±30; P<0.01). The mean donor age (years) was higher in the LDLT group (34.6±6.4) than in the SLT group (24.9±7.7; p<0.01), and the proportion of donors aged >40 years was higher in the LDLT group (25%) than in the SLT group (1.6%; P<0.01). The number of male donors was higher in the SLT group than in the LDLT group (SLT, 69.8% vs LDLT, 46.4%; P<0.02).
SURVIVAL OUTCOMES AND ANALYSIS OF RELATED RISK FACTORS:
The 1-, 3-, and 5-year graft survival rates did not significantly differ between the SLT (88.9%, 87.1%, and 83.6%, respectively) and LDLT groups (92.9%, 91.0%, and 91.0%, respectively; Figure 3A; p=0.31). The 1-, 3-, and 5-year overall survival rates were also not significantly different between the SLT (92.1%, 90.2%, and 86.6%, respectively) and LDLT groups (96.4%, 94.6%, and 94.6%, respectively; Figure 3B; P=0.21).
Fulminant hepatitis (OR, 8.77 [1.08–70.92]; P=0.042) was the only risk factor for graft failure. Other factors – including a recipient age >1 year, recipient weight >10 kg, transplantation type, total ischemic time >300 min, GRWR >4%, PELD score >20, donor age >40 years, and male donor – did not affect the graft survival rate (Table 2; P>0.05). Conversely, no significant risk factors related to overall survival were identified (Table 3; p>0.05), and the 3-month mortality rates were similar between the groups (Table 4).
SURGICAL COMPLICATIONS:
Surgical complications requiring intervention in the SLT and LDLT groups are described in Table 4. The rates of vascular complications – including the hepatic vein (9.5% vs 16.1%, P=0.28), portal vein (11.1% vs 14.3%, P=0.6), and hepatic artery (9.5% vs 10.7%, P=0.83) – were similar between the SLT and LDLT groups; however, the rate of biliary complications was higher in the LDLT group (28.6%) than in the SLT group (4.3%; P=0.01). The rates of intra-abdominal bleeding were comparable between the SLT and LDLT groups (6.3% vs 10.7%; P=0.39).
CAUSES OF DEATH:
In the SLT group, the common causes of deaths were hepatic artery complications (2/7, 28.6%) and cardiovascular events (2/7, 28.6%; Table 5). Cardiovascular events (2/7, 28.6%), hepatic artery complications (2/7, 28.6%), pulmonary hemorrhage (1/7, 14.3%), and acute respiratory distress syndrome (1/7, 14.3%) were the causes of 3-month mortality, whereas pneumonia (1/7, 14.3%) was the cause of late mortality >3 months after LT.
In the LDLT group, liver abscess (1/3, 33.3%) and aplastic anemia (1/3, 33%) were the causes of 3-month mortality, and there was 1 late mortality case of recurrent hepatoblastoma (1/3, 33.3%).
Discussion
In Korea, the annual number of pediatric LTs is less than 70; however, the proportion of pediatric DDLTs increased to 50% in 2014. The increased number of deceased donors was correlated with the increased number of SLTs. Possible reasons for the increased number of DDLTs between 2011 and 2013 were described in a Korean adult SLT study [8]. In 2010, an independent Korean organ procurement organization was established by the government. Since 2011, reporting potentially brain-dead candidates to this organization has been a legal obligation of medical staff who are primary caregivers of these patients. Another reason is changes in the surgical policy in 2013 to expand the donor organ pool for SLT [8]. If the outcomes of SLT are similar to those of LDLT, the increased number of SLTs could support the substitution of LDLT; however, no studies have reported outcomes of Korean pediatric SLT patients. We therefore compared the SLT and LDLT groups using the left lateral section, the most commonly used type of partial liver graft in pediatric recipients.
This study demonstrates that SLT grafts and overall survival outcomes are not inferior to those of LDLT. Previously, SLTs exhibited lower graft survival rates than LDLTs [2,7,10]. The 1-, 3-, and 5-year graft survival rates of SLT were lower than those of LDLT, based on ELTR data (78%, 74%, and 71% vs 83%, 80%, and 78%,
In most patients, the preoperative patient condition has been reported as a strong risk factor for graft or overall survival in pediatric LTs [5,6,11]. In our study, patients had a similar proportion of status 1 (SLT, 7.9% vs LDLT, 8.0%) and low proportion of malignant disease (SLT, 3.2% vs LDLT, 5.4%). A relatively short ischemic time was correlated with the geographical characteristics of Korea, and a younger donor age in the SLT group may lead to outcomes comparable to those in the LDLT group; however, the number of recipients was smaller in the SLT group than in the LDLT group.
The pretransplant patient conditions – including mechanical ventilation, renal failure, or needing intensive care unit management – were associated with poor outcomes for graft and overall survival [11]. The pretransplant state of the recipients was recorded using the KONOS status (similar to the UNOS status) [8] and PELD score in our registry, but not in detail. The PELD score, which was developed as a predictor for waiting list mortality, was not a risk factor for graft failure or overall survival [11,12]. In our study, both KONOS status and PELD score were also not risk factors for survival outcome, and only fulminant liver failure was a risk factor for graft failure.
As older donor age is regarded as a risk factor for poor recipient outcomes, older donors are not accepted by the SLT criteria [7]. However, there is considerable debate regarding whether the upper limit of the donor age – which ranges from 40 to 60 years in each country – affects the patient outcomes [8,11,13–15]. In this study, donor age was not a significant factor for graft failure or overall survival outcomes. One of the possible reasons may be the short ischemic time of Korean DDLT, as well as the strict donor age limit for potential SLTs, ranging from 10 to 40 years. The ischemic time considered meaningful and that was related to graft quality was 6–10 h [7,14]; however, in this study, the median total ischemic time of SLT was 256 (±163) min due to the short transport distance in this relatively small country. The relatively stable recipient conditions, compared with those of adult SLT recipients in Korea and pediatric SLT recipients in Western countries, could be an additional reason when considering the low PELD score and underlying diseases [8]. To validate a suitable donor age for SLT, a nation-based study is needed to exclude selection bias and may explain the meaning of other biochemical or biopsy results based on the donor age according to each nation’s situation [15,16].
Although similar in situ splitting techniques were performed for both SLT and LDLT [8,9], the total ischemic time was longer in the SLT group, and the biliary complication rate was significantly higher in the LDLT group. In many reports of living donor outcomes, biliary complications were the most common surgical complication requiring intervention (17.5–21.5%) [10,17,18]. In a previous study of pediatric LT using Korean data [18], the biliary complication rate was 22.8% (122/534) (proportion of a left lateral section, 32.5% in this study); however, in that study, the SLT group exhibited a very low occurrence of biliary complications (4.3%). This may be because detailed data were not available in the national registry database, as well as due to the relatively short follow-up period in the SLT group. Other possible technical reasons may be minimal dissection requirement and that the longer stump of the bile duct can be retained in SLT than in LDLT. The left bile duct in the graft should be shorter and more dissected to maintain the arterial supply to the remnant bile duct of the live donor.
Excluding patients with biliary complications, vascular complications were similar in both groups. The incidence of hepatic artery complications in pediatric LT patients ranged from 1.5% to 18.3% [4,19,20], while that of portal vein-related problems ranged from 1.5% to 8.5% [4,20]; the rates of hepatic vein complications ranged from 0% to 9.1% [9,18]. This vascular complication was more common in patients receiving a partial liver graft than those receiving a whole-liver graft. The incidence of hepatic artery complications was higher in patients aged <1 year, with metabolic liver disease, or with multiple anastomosis and a small hepatic artery [9,13,20]. However, technical complication-related mortalities are uncommon in pediatric LTs using partial grafts [13,19], excluding hepatic artery complications. In this study, hepatic artery complications were related to early mortality in the SLT group; thus, the policy of using only left and middle hepatic arteries – preserving the celiac axis to right trisection graft – should be re-evaluated in our Korean SLT procedures.
This study has some limitations. First, it was a retrospective study, requiring dependence on the completeness of medical records. In particular, detailed information was not available in the SLT group as the data were retrieved from a national registry database. Second, the LDLT outcomes of a single high-volume LDLT center were compared with those of national data in the SLT group. Center experience was considered a significant factor affecting the recipient’s outcomes [7,21]; however, most pediatric SLTs in Korea (90%) were performed in 1 of 3 high-volume LDLT centers. Thus, the comparison between the 2 groups in this was not performed. Third, this study reflected the special situation of SLT and LDLT in Korea. The indication and techniques of SLT, and waiting and ischemic times of the deceased organ in Korea are quite different from those in other countries. Therefore, this conclusion may not be directly applicable to other countries.
The graft and overall survival rates, including early mortality rates for SLT and LDLT, were not different in pediatric patients in Korea. To the best of our knowledge, this is the first report of the outcomes of Korean pediatric SLTs. Fulminant hepatic failure was the only risk factor affecting graft survival outcomes; however, as biliary complications were more common in the LDLT group, further evaluation is required.
Conclusions
In conclusion, the graft and overall survival rates of SLT and LDLT were not significantly different in pediatric patients in Korea, and fulminant hepatic failure was the only risk factor affecting graft survival outcomes.
Figures
Tables
Table 1. Demographics of donors and recipients in the SLT versus LDLT groups.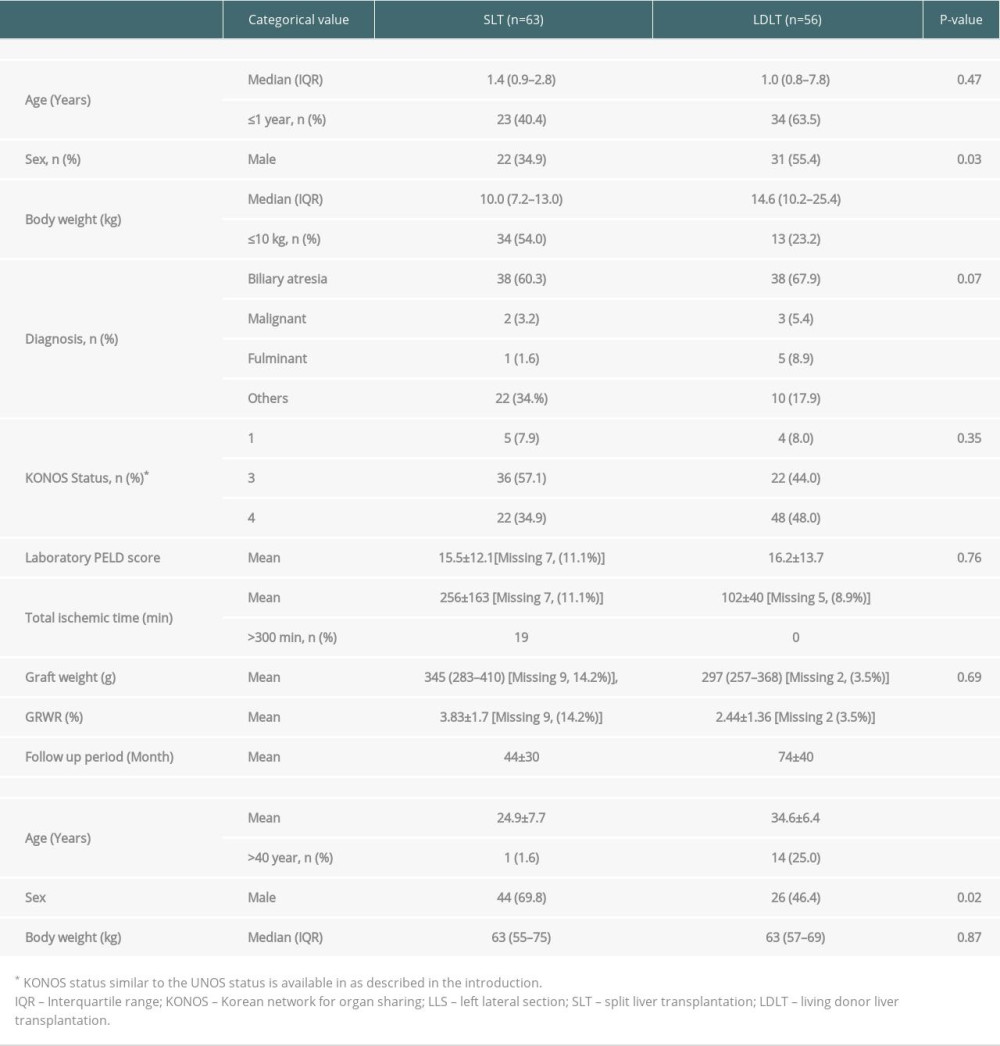 Table 2. Multivariate analysis of factors affecting graft failure.
Table 2. Multivariate analysis of factors affecting graft failure.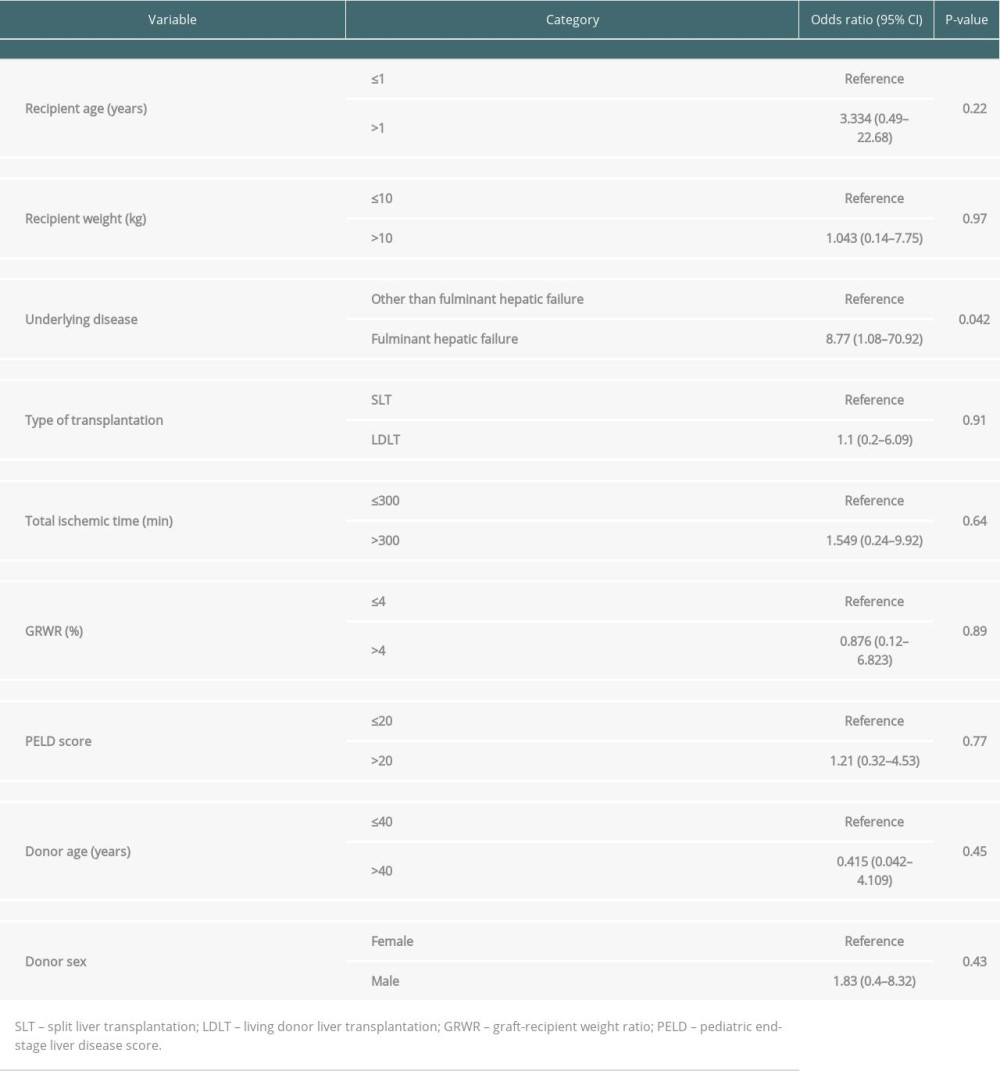 Table 3. Multivariate analysis of factors affecting overall survival.
Table 3. Multivariate analysis of factors affecting overall survival.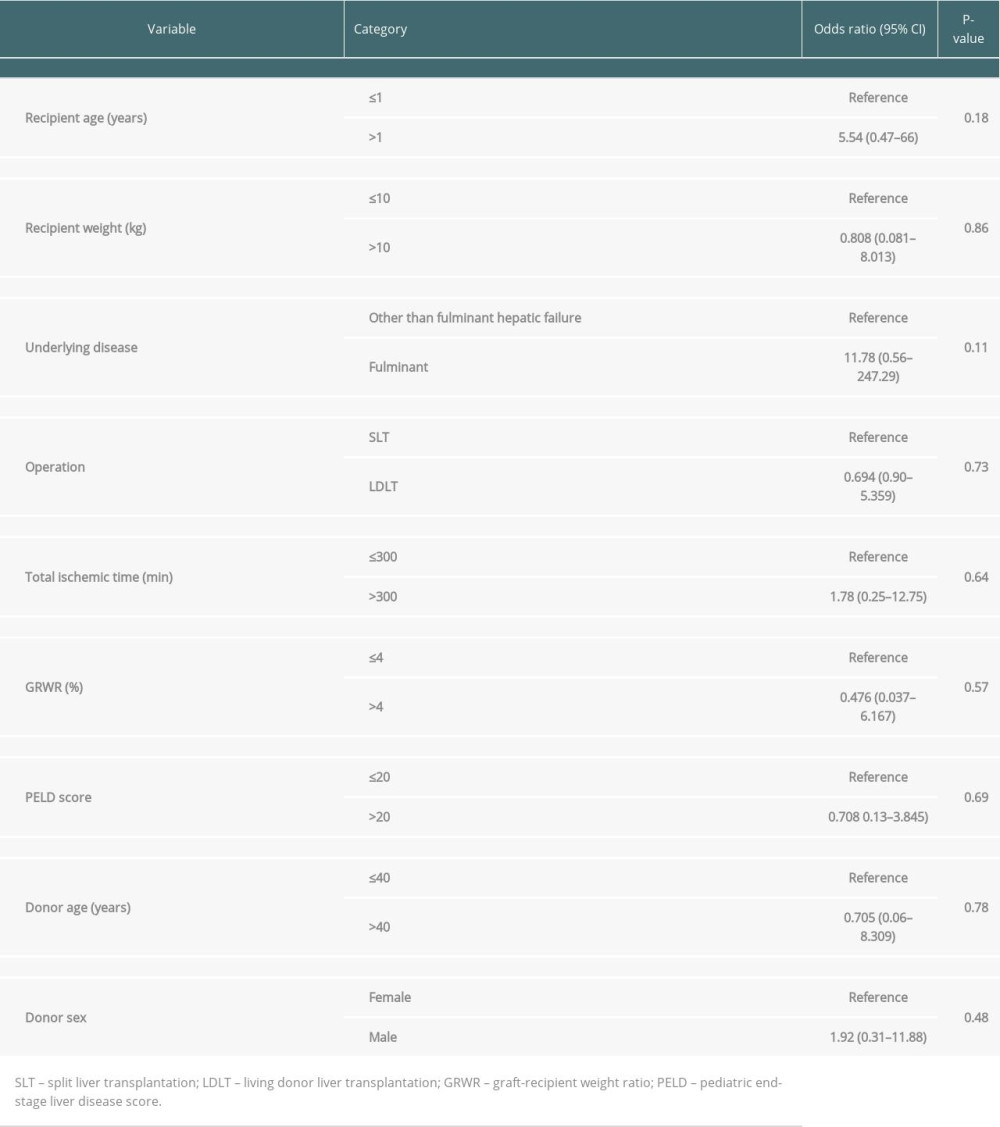 Table 4. Technical complications and deaths in the SLT versus LDLT groups.
Table 4. Technical complications and deaths in the SLT versus LDLT groups.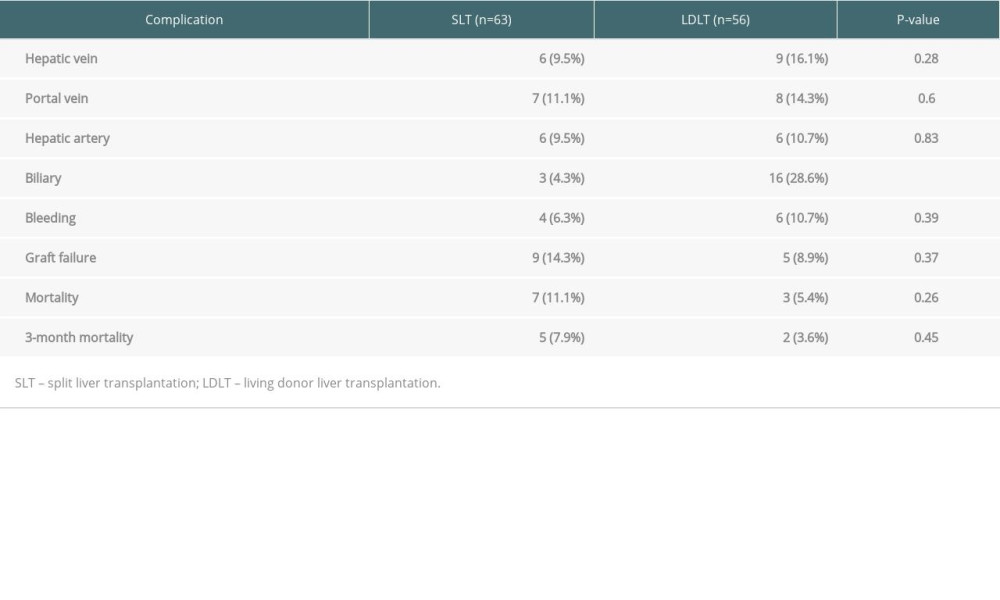 Table 5. Cause of death in the SLT versus LDLT groups.
Table 5. Cause of death in the SLT versus LDLT groups.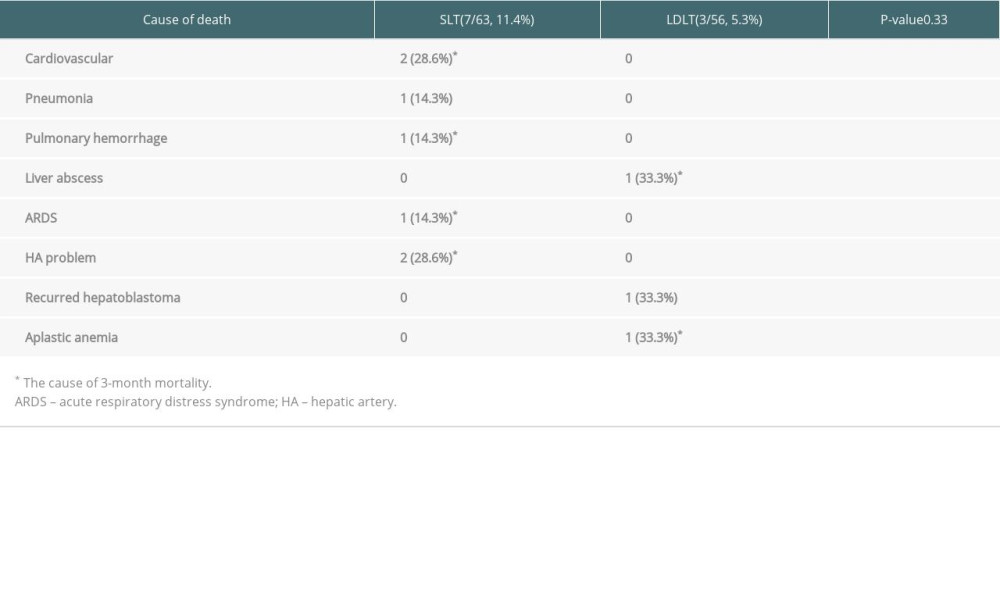
References
1. Kim WR, Lake JR, Smith JM, OPTN/SRTR 2017 Annual Data Report: Liver: Am J Transplant, 2019; 19(Suppl 2); 184-283
2. Adam R, Karam V, Cailliez V, 2018 Annual Report of the European Liver Transplant Registry (ELTR) – 50-year evolution of liver transplantation: Transpl Int, 2018; 31; 1293-317
3. Farmer DG, Venick RS, McDiarmid SV, Predictors of outcomes after pediatric liver transplantation: An analysis of more than 800 cases performed at a single institution: J Am Coll Surg, 2007; 204; 904-14 discussion 914–16
4. D’Alessandro AM, Knechtle SJ, Chin LT, Liver transplantation in pediatric patients: Twenty years of experience at the University of Wisconsin: Pediatr Transplant, 2007; 11; 661-70
5. Austin MT, Feurer ID, Chari RS, Survival after pediatric liver transplantation: Why does living donation offer an advantage?: Arch Surg, 2005; 140; 465-70 discussion 470–71
6. Mogul DB, Luo X, Bowring MG, Fifteen-year trends in pediatric liver transplants: Split, whole deceased, and living donor grafts: J Pediatr, 2018; 196; 148-53e2
7. Lee KW, Cameron AM, Maley WR, Factors affecting graft survival after adult/child split-liver transplantation: Analysis of the UNOS/OPTN data base: Am J Transplant, 2008; 8; 1186-96
8. Chul Yoon K, Song S, Jwa EK, Survival outcomes in split compared with whole liver transplantation: Liver Transpl, 2018; 24; 1411-24
9. Hong SK, Yi NJ, Chang H, The rate of hepatic artery complications is higher in pediatric liver transplant recipients with metabolic liver diseases than with biliary atresia: J Pediatr Surg, 2018; 53; 1516-22
10. Diamond IR, Fecteau A, Millis JM, Impact of graft type on outcome in pediatric liver transplantation: A report From Studies of Pediatric Liver Transplantation (SPLIT): Ann Surg, 2007; 246; 301-10
11. McDiarmid SV, Anand R, Martz K, A multivariate analysis of pre-, peri-, and post-transplant factors affecting outcome after pediatric liver transplantation: Ann Surg, 2011; 254; 145-54
12. Bourdeaux C, Tri TT, Gras J, PELD score and posttransplant outcome in pediatric liver transplantation: A retrospective study of 100 recipients: Transplantation, 2005; 79; 1273-76
13. Cardillo M, De Fazio N, Pedotti P, Split and whole liver transplantation outcomes: A comparative cohort study: Liver Transpl, 2006; 12; 402-10
14. Gao Q, Mulvihill MS, Scheuermann U, Improvement in liver transplant outcomes from older donors: A US National Analysis: Ann Surg, 2019; 270; 333-39
15. Hackl C, Schmidt KM, Susal C, Split liver transplantation: Current developments: World J Gastroenterol, 2018; 24; 5312-21
16. Barbas AS, Knechtle SJ, Expanding the donor pool with normothermic ex vivo liver perfusion: The future is now: Am J Transplant, 2016; 16; 3075-76
17. McLin VA, Allen U, Boyer O, Early and late factors impacting patient and graft outcome in pediatric liver transplantation: Summary of an ESPGHAN Monothematic Conference: J Pediatr Gastroenterol Nutr, 2017; 65; e53-e9
18. Kim JM, Kim KM, Yi NJ, Pediatric liver transplantation outcomes in Korea: J Korean Med Sci, 2013; 28; 42-47
19. Doyle MB, Maynard E, Lin Y, Outcomes with split liver transplantation are equivalent to those with whole organ transplantation: J Am Coll Surg, 2013; 217; 102-12 discussion 113–14
20. Zhang R, Zhu ZJ, Sun LY, Outcomes of pediatric liver transplantation: Deceased donor liver transplantation vs living donor liver transplantation: Transplant Proc, 2018; 50; 3601-5
21. Lee H, Jang EJ, Kim GH, Effect of case volume on mortality after pediatric liver transplantation in Korea: Transplantation, 2019; 103; 1649-54
Figures
Tables
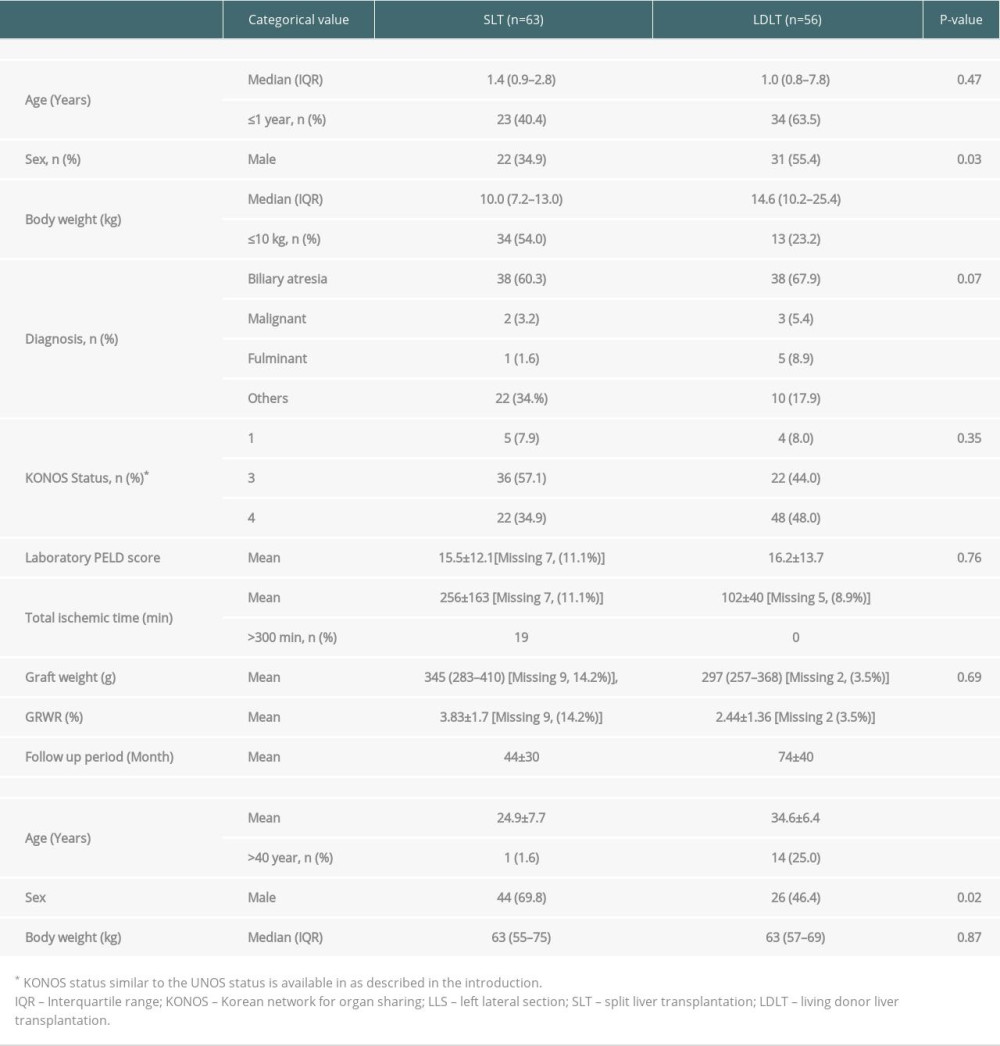 Table 1. Demographics of donors and recipients in the SLT versus LDLT groups.
Table 1. Demographics of donors and recipients in the SLT versus LDLT groups.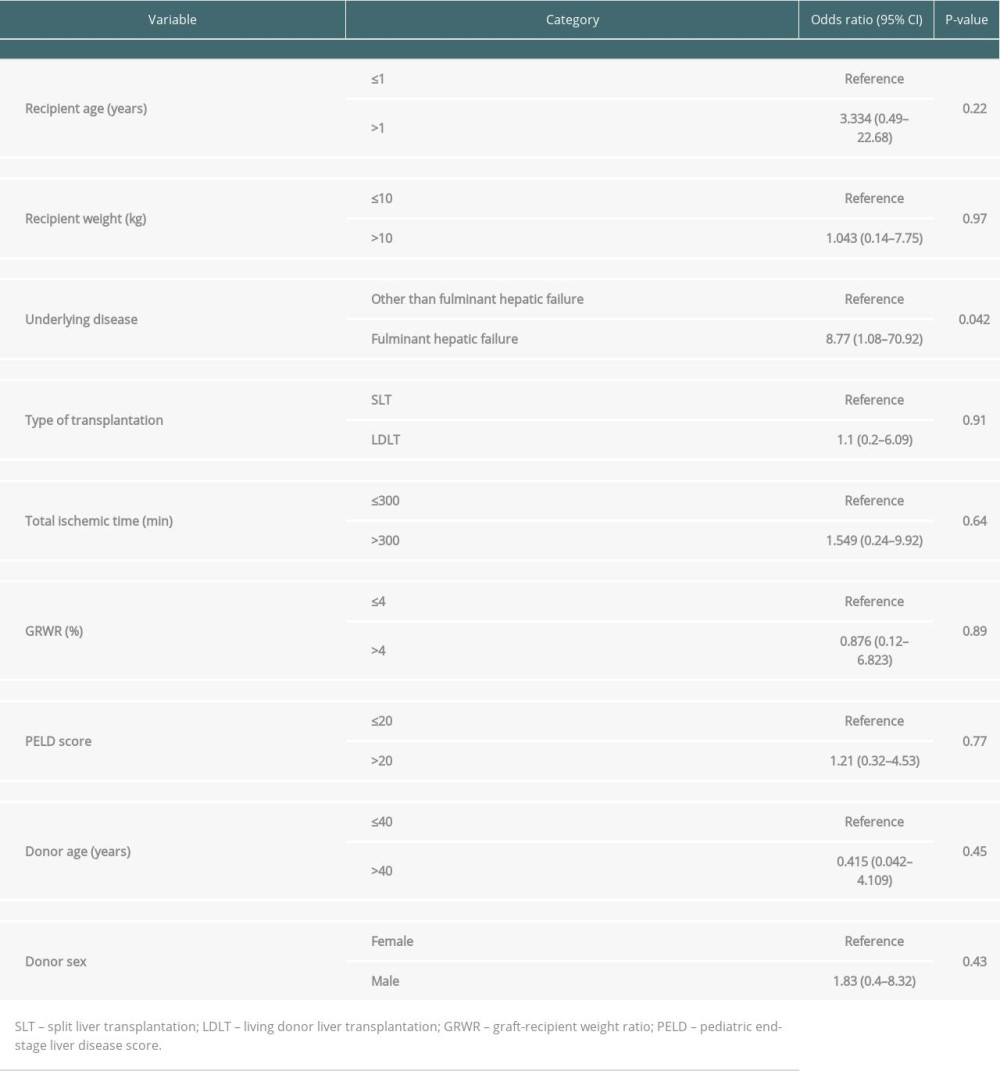 Table 2. Multivariate analysis of factors affecting graft failure.
Table 2. Multivariate analysis of factors affecting graft failure.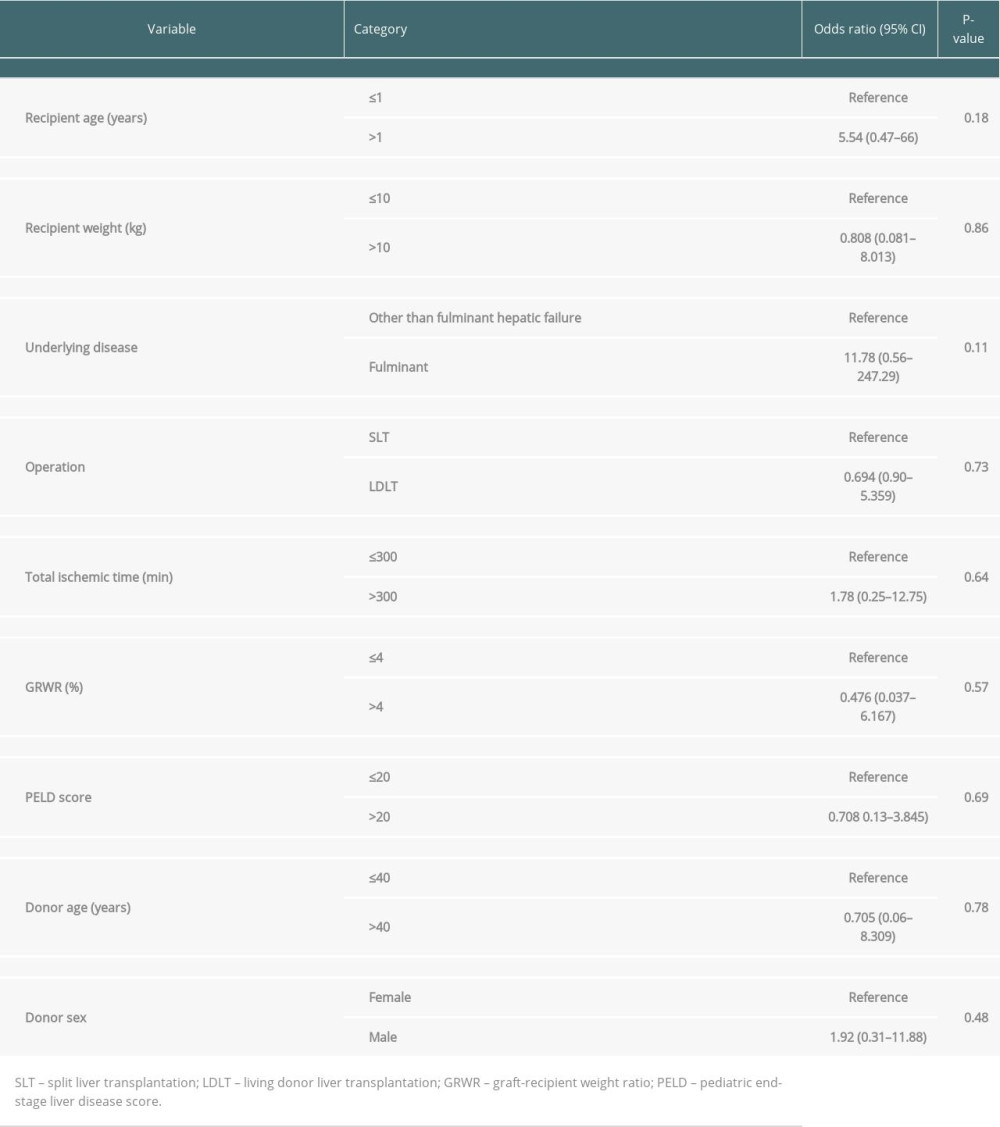 Table 3. Multivariate analysis of factors affecting overall survival.
Table 3. Multivariate analysis of factors affecting overall survival.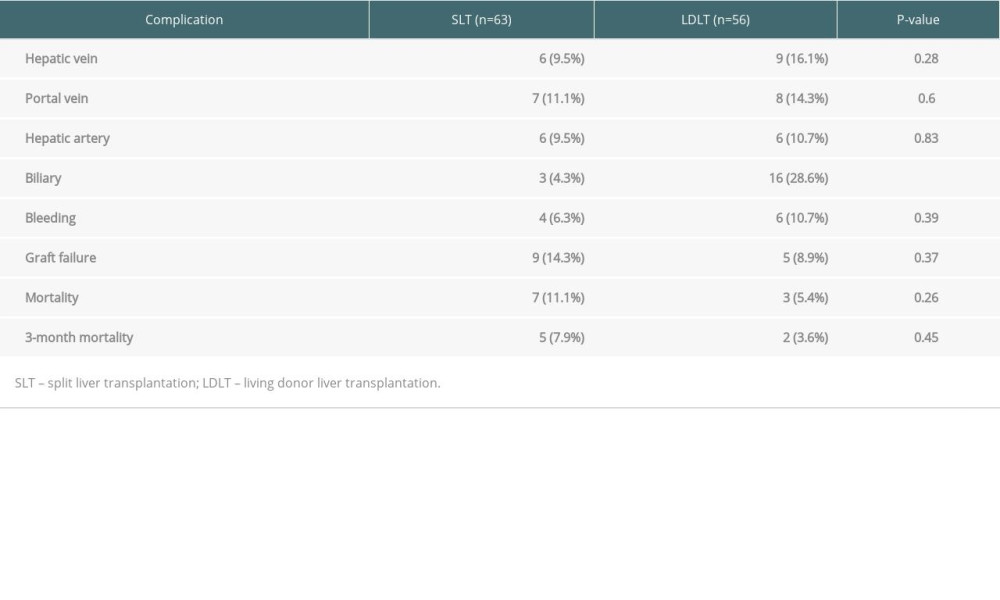 Table 4. Technical complications and deaths in the SLT versus LDLT groups.
Table 4. Technical complications and deaths in the SLT versus LDLT groups.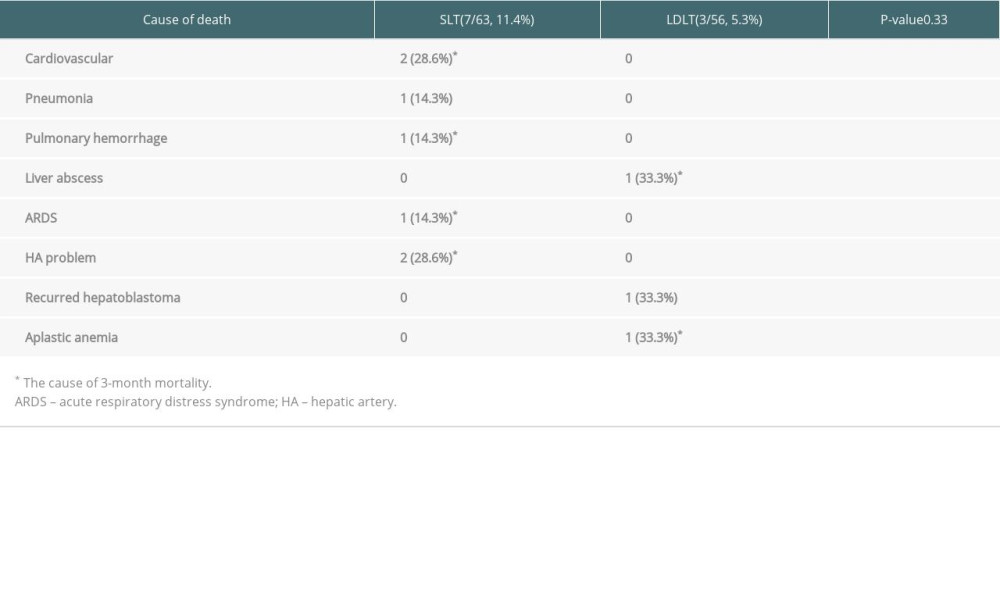 Table 5. Cause of death in the SLT versus LDLT groups.
Table 5. Cause of death in the SLT versus LDLT groups.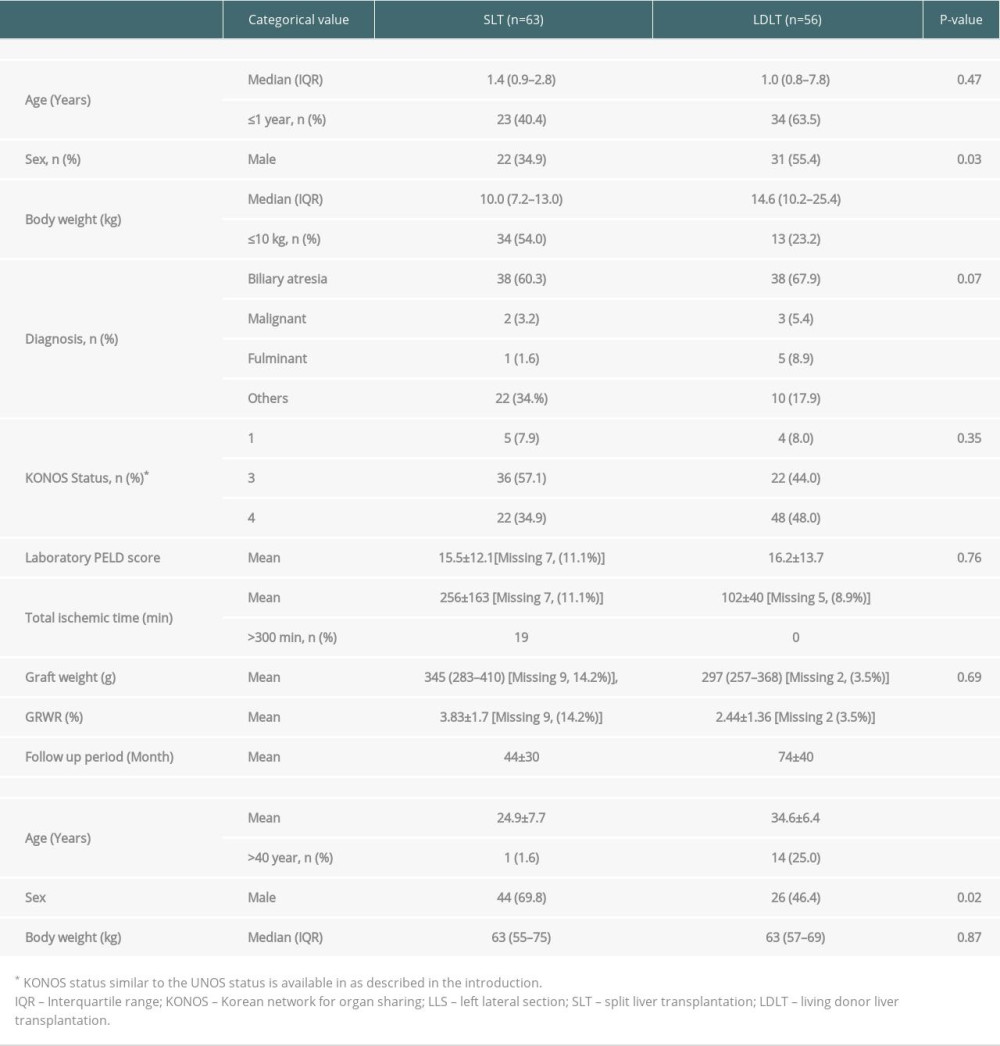 Table 1. Demographics of donors and recipients in the SLT versus LDLT groups.
Table 1. Demographics of donors and recipients in the SLT versus LDLT groups.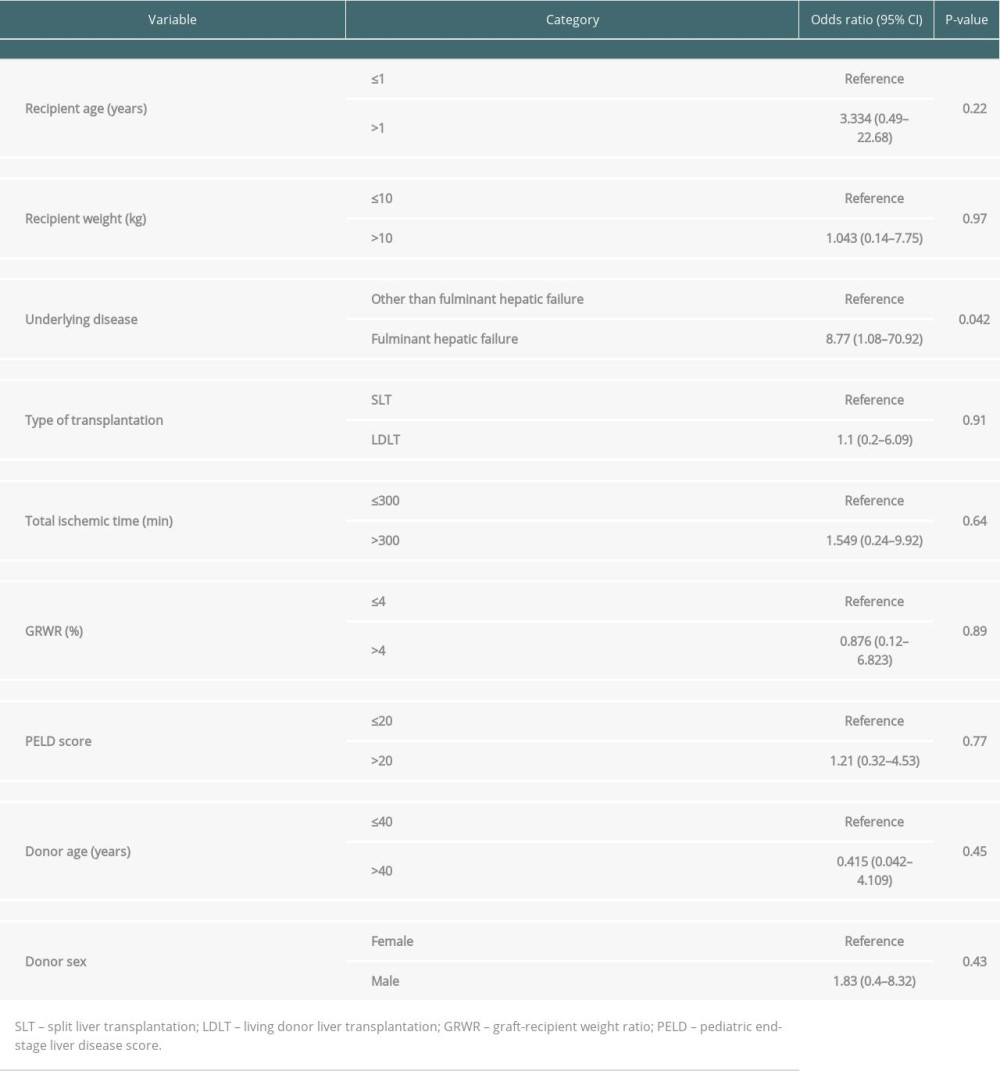 Table 2. Multivariate analysis of factors affecting graft failure.
Table 2. Multivariate analysis of factors affecting graft failure.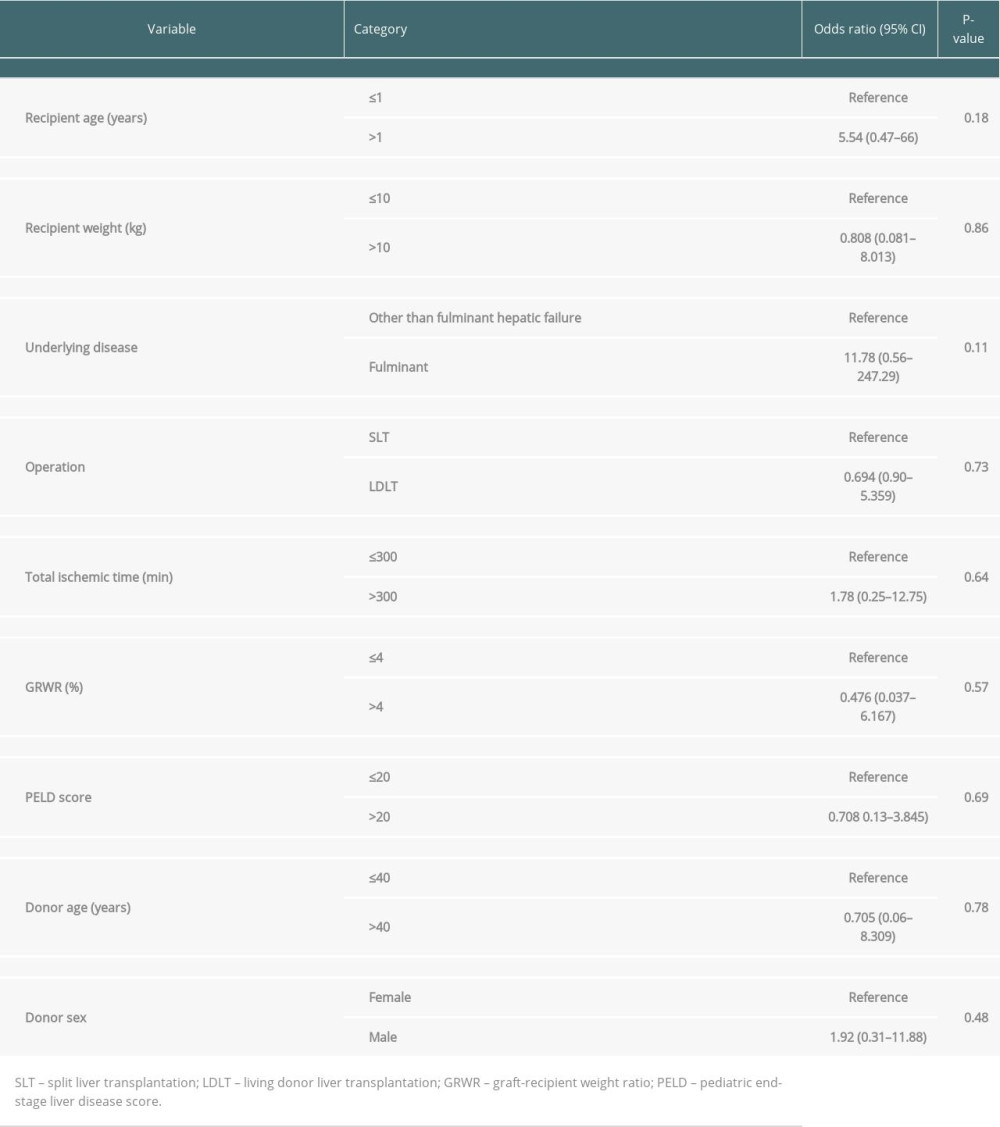 Table 3. Multivariate analysis of factors affecting overall survival.
Table 3. Multivariate analysis of factors affecting overall survival.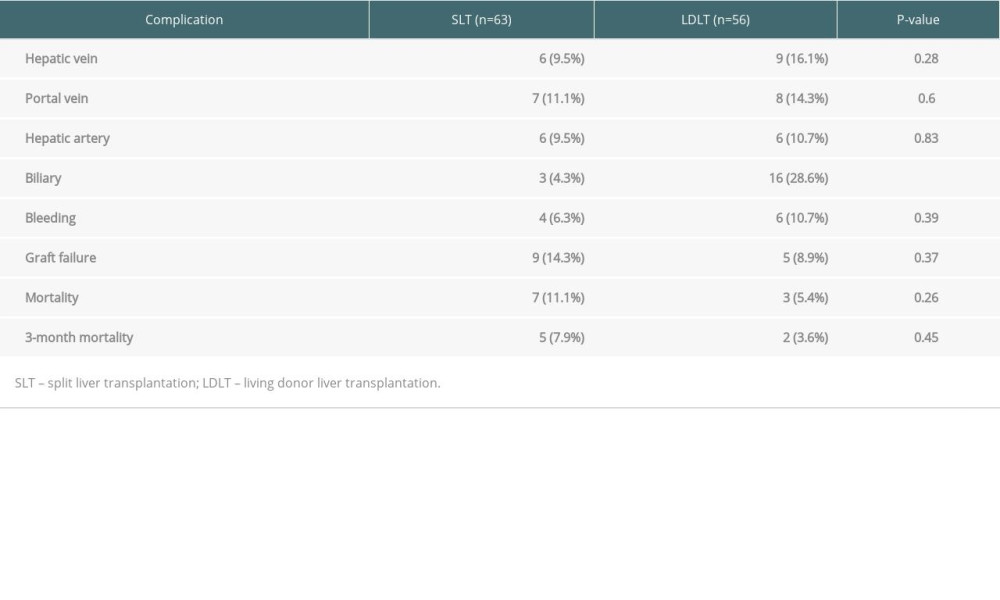 Table 4. Technical complications and deaths in the SLT versus LDLT groups.
Table 4. Technical complications and deaths in the SLT versus LDLT groups.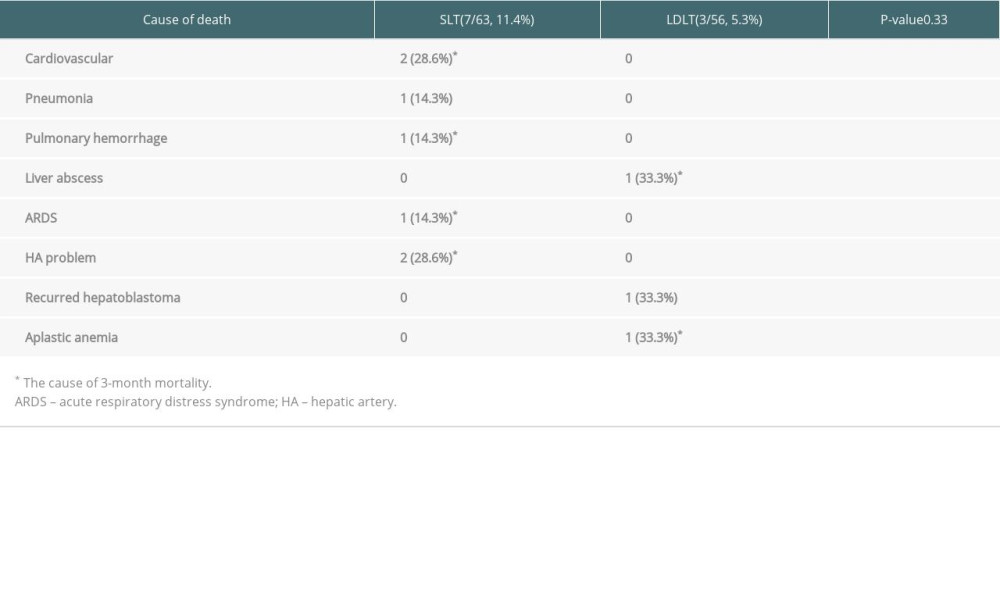 Table 5. Cause of death in the SLT versus LDLT groups.
Table 5. Cause of death in the SLT versus LDLT groups. In Press
18 Mar 2024 : Original article
Does Antibiotic Use Increase the Risk of Post-Transplantation Diabetes Mellitus? A Retrospective Study of R...Ann Transplant In Press; DOI: 10.12659/AOT.943282
20 Mar 2024 : Original article
Transplant Nephrectomy: A Comparative Study of Timing and Techniques in a Single InstitutionAnn Transplant In Press; DOI: 10.12659/AOT.942252
28 Mar 2024 : Original article
Association Between FEV₁ Decline Rate and Mortality in Long-Term Follow-Up of a 21-Patient Pilot Clinical T...Ann Transplant In Press; DOI: 10.12659/AOT.942823
02 Apr 2024 : Original article
Liver Transplantation from Brain-Dead Donors with Hepatitis B or C in South Korea: A 2014-2020 Korean Organ...Ann Transplant In Press; DOI: 10.12659/AOT.943588
Most Viewed Current Articles
05 Apr 2022 : Original article
Impact of Statins on Hepatocellular Carcinoma Recurrence After Living-Donor Liver TransplantationDOI :10.12659/AOT.935604
Ann Transplant 2022; 27:e935604
12 Jan 2022 : Original article
Risk Factors for Developing BK Virus-Associated Nephropathy: A Single-Center Retrospective Cohort Study of ...DOI :10.12659/AOT.934738
Ann Transplant 2022; 27:e934738
22 Nov 2022 : Original article
Long-Term Effects of Everolimus-Facilitated Tacrolimus Reduction in Living-Donor Liver Transplant Recipient...DOI :10.12659/AOT.937988
Ann Transplant 2022; 27:e937988
15 Mar 2022 : Case report
Combined Liver, Pancreas-Duodenum, and Kidney Transplantation for Patients with Hepatitis B Cirrhosis, Urem...DOI :10.12659/AOT.935860
Ann Transplant 2022; 27:e935860








