09 May 2023: Original Paper
Outcomes of Kidney Transplantation in Older Recipients
Ehab Hammad1ABDEF*, Dieter Broering2A, Yaser Shah1E, Ahmed Nazmi1E, Amira Al Abassi3E, Jens G. Brockmann3E, Samir Elshouny4BE, Layal Fajji2B, Hassan Aleid1E, Tariq Ali1ACEFDOI: 10.12659/AOT.938692
Ann Transplant 2023; 28:e938692
Abstract
BACKGROUND: Access to kidney transplantation is limited for elderly patients with end-stage renal disease (ESRD), who often die while on the waiting list or receive kidneys from marginal deceased donors. In our transplantation center, most donated kidneys were from younger living relatives, in whom donations to elderly outcomes were not previously studied. In this study, we aimed to determine the short- and long-term outcomes of patients aged ³65 years to justify the use of kidneys from younger donors in older recipients. We also compared the outcomes between those who received kidneys from living donors (LDs) and deceased donors (DDs).
MATERIAL AND METHODS: We analyzed the patients’ demographic data and the 1-, 5-, and 10-year patient and graft survival rates of patients aged ≥65 years who received kidney transplants between January 2005 and December 2020.
RESULTS: Among 158 patients, 136 received kidneys from LD and 22 from DD. The mean age was 69 years old. In this cohort, the most common cause of ESRD was diabetes. The graft survival rates were 99%, 96%, and 94% after 1, 5, and 10 years, respectively. Patient survival was 94%, 83%, and 61% after 1, 5, and 10 years, respectively. Delayed graft function rates, 1-year patient survival, and 5- and 10-year graft survival rates were lower in the DD group. Ischemic heart disease and transplantation from DD were independent risk factors for mortality.
CONCLUSIONS: Our study demonstrated reasonably good patient and graft survival rates in older patients. Outcomes were better in patients who received kidneys from LD.
Keywords: Kidney Transplantation, Living Donors, Aged, Humans, Graft Survival, Tissue Donors, Kidney Failure, Chronic, Risk Factors, Kidney, Treatment Outcome
Background
Older adults have an increased prevalence of end-stage renal disease (ESRD) owing to continuous improvements in medical care and the ability to treat co-morbid conditions. Data from the United States Renal Data System (USRDS) registry showed that half of the patients in the United States who initiated renal replacement (RRT) therapy were over 65 years old [1]. However, dialysis may not be considered the best modality of RRT for these patients compared with kidney transplantation [2,3]. The 1-year mortality after dialysis initiation in older adults is 30%, according to the USRDS registry [4]. There is evidence that older patients undergoing chronic haemodialysis have a high burden of frailty [5], accidental falls [6], and cognitive impairment [7]. Improved quality of life and survival after kidney transplantation have been demonstrated in several studies [2,8–10]. Lonning et al showed a clinically significant improvement in health-related quality of life (HRQoL) after kidney transplantation in 120 patients aged 65 years or older [11]. The HRQoL scores were similar to those described in an age-matched general population, except in the social function domain after 12 months of engraftment [11]. Oniscu et al reported that kidney transplantation offered a significant survival advantage over dialysis in 325 elderly patients who were suitable transplant candidates [9].
Although aging is no longer considered a contraindication to transplantation, several factors, such as shortened life expectancy, limited donor pool, and co-morbid conditions, result in limited access to transplantation for older patients [12,13]. The likelihood of being listed for transplant falls with increasing age. Even for patients listed for transplantation, the probability of older patients receiving a transplant is much lower than for younger patients; only 8% of listed patients aged 65–75 years old receive transplants within 5 years of dialysis initiation [14]. Owing to these challenges, transplantation from living donors (LD) may be a good option for older patients; however, this remains debatable because of the shorter life expectancy, especially if potential donors are from younger age groups.
Our center is one of the largest in the Middle East for organ transplantations. In 2021, we performed 356 kidney transplants (314 adult and 42 pediatric patients). Approximately one-quarter of our patients had type II diabetes and other co-morbid conditions. As the risk of ESRD is higher in elderly populations, our center has been performing kidney transplantations in aging patients. In Saudi Arabia, approximately 80% of kidney transplantations are performed with kidneys from LDs, as the deceased kidney donation program is not well established. Our country has an extended family system, and many people are willing to donate kidneys to their relatives. For older patients, their children usually come forward to donate kidneys.
This study aimed to evaluate patient and graft outcomes in older patients with ESRD who received kidney transplantations from young living kidney donors. We also aimed to compare the outcomes between those who received kidneys from LDs and deceased donors (DDs).
Material and Methods
STATISTICAL ANALYSIS:
Data were analyzed using GraphPad Prism 9 software (GraphPad Software, San Diego, CA). Data are expressed as frequencies (percentages), means, standard deviations, and ranges, as appropriate. The chi-square or Fisher’s exact test was used to compare categorical variables. The
ETHICS APPROVAL:
The study was approved by the institution’s ethics committee (Study Number: 2221050). Informed consent was waived because of the retrospective nature of the study.
Results
DEMOGRAPHIC DATA:
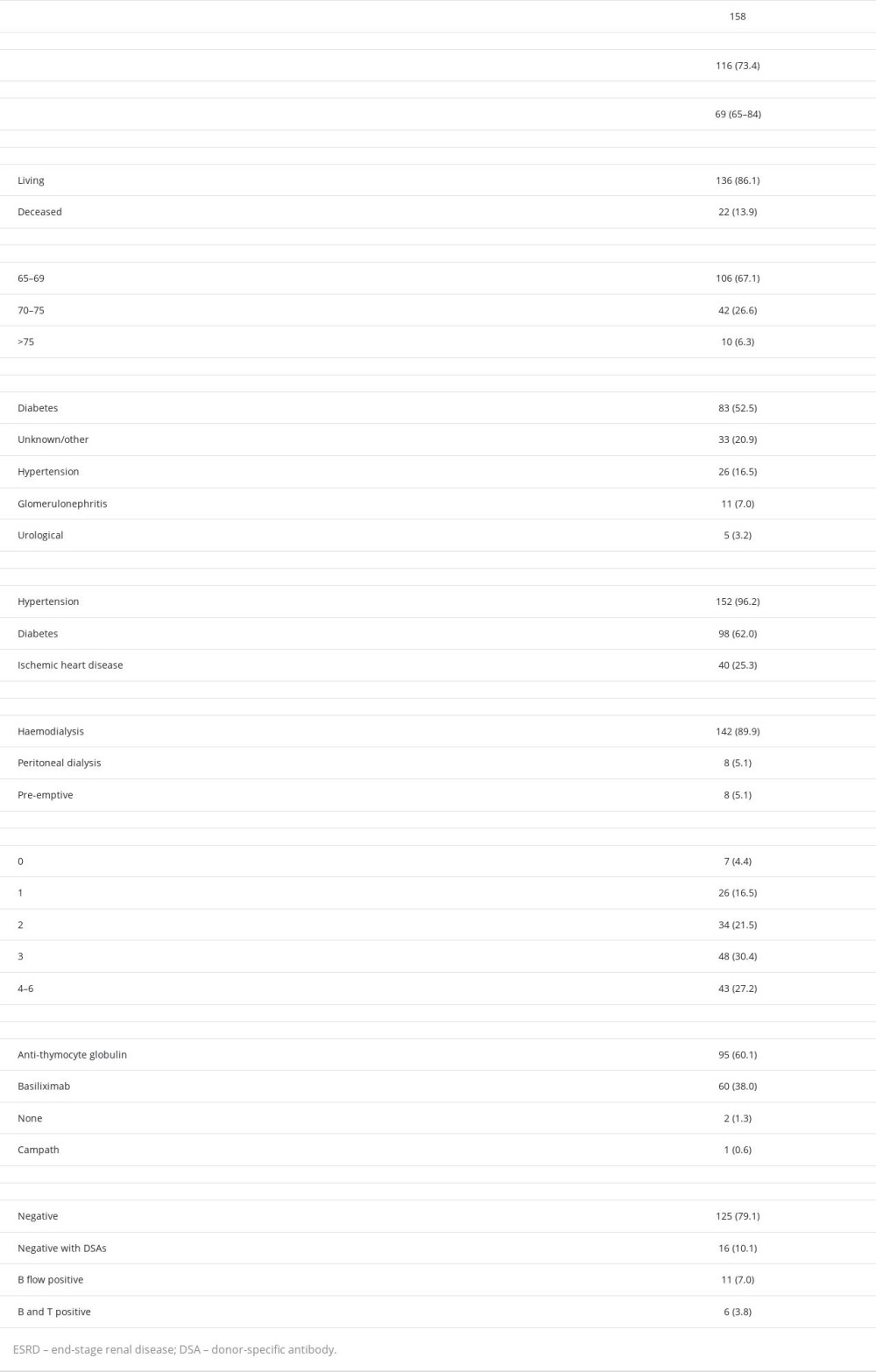
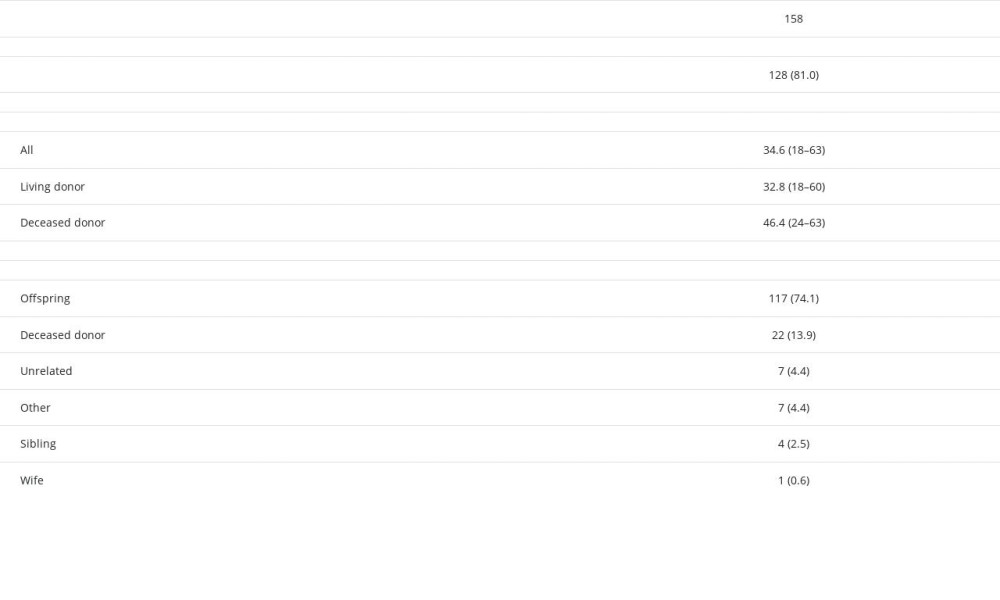
A total of 158 patients were included in this study. Among these, 73% were male, and 86% received kidneys from LDs (Table 1). The mean age at the time of transplantation was 69 (65–84) years old. In our cohort, 53% of the patients had developed ESRD due to diabetes, and 17% due to hypertension. However, almost all patients were hypertensive, and one-quarter had ischemic heart disease (Table 1). Immunologically, almost 73% of the patients had ≤3 HLA mismatches with their donors, and most of them had negative flow crossmatches (89%) (Table 1). The most common induction agent was ATG (60%), followed by basiliximab (38%); 2 patients did not receive any induction agent (Table 1). The donors were young (mean 35 years), 81% were male, and 74% were offspring of the recipients (Table 2).
OUTCOMES:
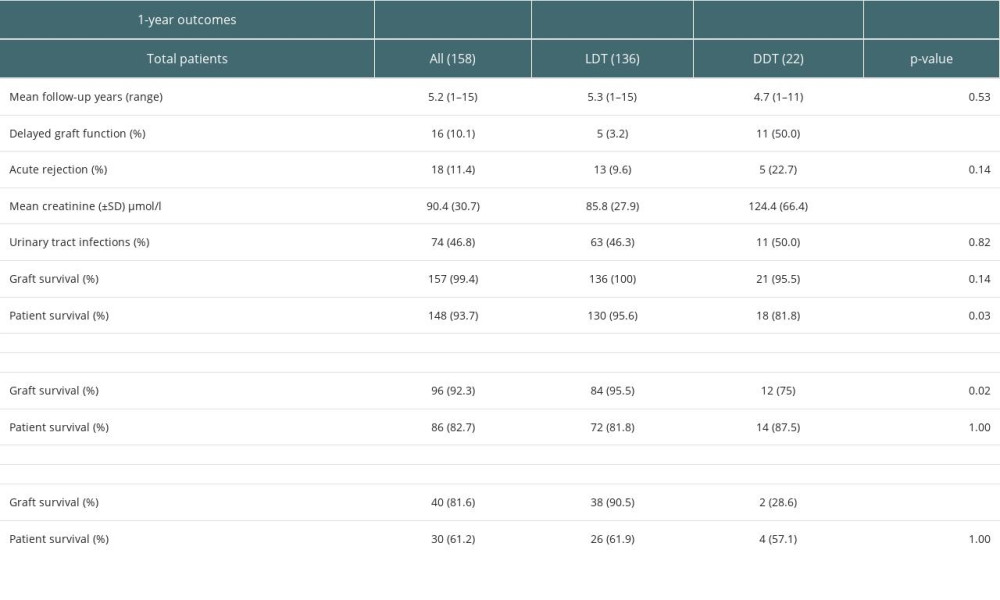
Of the 158 recipients, 136 received kidneys from LD and 22 from DD. The mean follow-up period was 5.2 years. Sixteen patients (10%) developed DGF. The DGF rates were significantly higher in the DD group than in the LD group (P<0.01) (Table 3). Acute rejection was recorded in 11% of the total patients, 10% of the LD, and 23% of the DD groups (P=0.14). The serum creatinine level at the end of the first year was significantly higher in the DD group than in the LD group (124 vs 86 μmol/l, P<0.01). The graft survival in the first year was 99.4%. None of the LD grafts were lost in the first year. Ten patients died in the first year; more patients died in the DD group than in the LD group (P=0.03) (Table 3, Figure 1).
There were 104 patients who completed 5 years of follow-up (including those who either died or lost grafts during this period). Five-year graft survival was 92%; graft loss was higher in the DD group (P=0.02) (Table 3). Patient survival was 83%, and there was no difference in survival rates between the DD and LD groups (P=1.00) (Figure 1).
Forty-nine patients completed 10 years of follow-up (including those who either died or lost grafts during this period). The 10-year graft survival was 82%, and graft survival was significantly lower in the DD group (Table 3). Patient survival was 61%, and survival rates were similar between the 2 groups (P=1.00) (Table 3, Figure 1).
Mortality was higher in female patients (38%) in comparison to male patients (29%) but this difference was not statistically significant in the univariate (
Nineteen patients (12%) developed malignancies during the follow-up period. The malignancy rate during the first year was 4%. Ten patients were diagnosed with solid organ/tissue cancers, 6 with Kaposi sarcoma, 2 with lymphoma, and 1 with skin cancer.
MORTALITY AND GRAFT LOSS:
During the follow-up period, 50 patients died. Of these, 20 (40%) died of cardiac causes, 9 (18%) due to malignancy, 9 (18%) due to sepsis, 6 (12%) due to COVID-19, and 6 (12%) due to other causes.
Excluding graft loss due to death, 9 grafts were lost during the follow-up period. Four grafts were lost due to chronic allograft nephropathy, 3 due to unresolved acute kidney injury after an acute illness, and 1 due to BK nephropathy. One graft was lost because of primary non-function.
MULTIVARIATE ANALYSIS:
In the multivariate analysis, ischemic heart disease (OR 3.0, p<0.01) and kidneys from DDs (OR 2.9, P=0.04) were independent risk factors for mortality (Table 4). Patients with more HLA mismatches had higher risk of acute rejection (P<0.01). Age, sex, kidneys used from DDs, and DGF were not associated with acute rejection (Table 4).
Discussion
Our study showed that older patients had good short- and long-term outcomes after kidney transplantation. Therefore, utilizing kidneys from younger donors is a reasonable option for older patients. Patient and graft survival rates were better in patients who received kidneys from LDs.
The USRDS database has reported that the number of elderly patients starting dialysis is consistently increasing, which exceeded 1500 per million per year in 2018 [19]. The median age at dialysis initiation of patients in the United States is 64 years [20]. The cost of dialysis in elderly patients is approximately 10–35% higher than in younger patients [21]. As the prevalence of ESRD in adults aged >65 years increases worldwide [22], the number of older candidates for kidney transplantation also increases [23]. Older patients with ESRD often have multiple co-morbid conditions, including cardiovascular disease and diabetes, which may affect their outcomes after transplantation. Despite this, outcomes in older patients after kidney transplantation remain better than those in patients with other modalities of renal replacement therapy [11,24].
Due to the shorter life expectancies of older people and shortages in the donor pool, patients may be either denied kidney transplantation, especially from LDs, or waitlisted for extended criteria donors. Unfortunately, many patients die while on the waiting list [25]. Stevens et al reported that the probability of being listed for DD transplants within 1 year of commencing RRT was 4% for patients aged between 65 and 74.9 years and 0.8% for patients aged ≥75 years [14]. If listed, the probabilities of receiving a DD transplant within 5 years of starting RRT were 8% and 0%, respectively. Therefore, kidney transplantation from DDs is limited for elderly patients. In our program, most kidney donations are from living kidney donors because the deceased kidney donation program is not well-developed. Approximately 80% of our patients receive kidneys from LDs. In contrast, around 22% of kidney donations in the USA come from LDs [26]. One of the main reasons for this contrast is the extended family system and the willingness of people in Saudi Arabia to donate kidneys to their relatives. Approximately 75% of the elderly patients at our center receive kidneys from their offspring. The donation rates from close relatives in the USA are much lower; approximately 150 out of 5000 donors are close relatives of the recipients. Furthermore, our donor population was much younger (mean age 35 years at the time of donation) than that in the USA (more than 60% of the LDs are aged 40 or above) [26]. Because our donors are young, it is important to ensure that the outcomes of older patients justify kidney donation from younger donors.
Owing to advanced age and co-morbidities, mortality rates are higher in elderly transplant patients than in younger recipients [27]. A study from Colombia reported that the survival rates of older kidney transplant recipients were 89%, 70%, and 55% at 1, 5, and 10 years, respectively [28]; in our study, patient survival rates were 94%, 83%, and 61%, respectively. The 10-year mortality rate is not surprisingly high owing to advanced age and co-morbid conditions. However, the prognosis of elderly patients undergoing dialysis is worse [4,29]. A meta-analysis of 89 studies (294 921 elderly patients) reported a 1-year survival rate of 73% after dialysis initiation [30]. A study of Medicare beneficiaries of elderly patients has shown mortality rates of >50% within 1 year of starting dialysis [4]. The 1-year mortality rate after dialysis initiation for adults >65 years of age, based on the USRDS registry, was reported to be around 30% [4]. Our study found a 10-year mortality rate of around 40%, which equates to an annual mortality rate of approximately 4% in the elderly transplant population. The annual mortality on dialysis in Saudi Arabia is reported to be 12%, regardless of age [31]. In comparison, the annual mortality rate in the elderly USA population (≥65 years) is approximately 3% [32]. Therefore, although the annual mortality rate in our cohort is slightly higher than in the general population, it remains significantly lower than in the dialysis population.
The options for older patients with ESRD are limited; either they receive extended criteria kidneys or remain on the waiting list. Therefore, kidney transplantation from younger patients is a viable option, as shown by the outcomes of this study.
Our study results showed that graft survival rates were 99%, 96%, and 94% after 1, 5, and 10 years, respectively. Our study also showed better graft survival rates in patients who received kidneys from LDs than in those who received kidneys from DDs. Dempster et al reported high DGF rates and poor graft survival in elderly patients, which were associated with older donors [2]. The DGF rates in the DD group in our study were significantly lower (
The most common causes of death in our cohort were cardiovascular disease, malignancy, sepsis, and COVID-19. Ischemic heart disease was identified as an independent risk factor for mortality in the elderly transplant population. Similarly, ischemic heart disease is the most common cause of death in non-transplant elderly populations [35]. A previous study showed that cardiovascular disease was the most common cause of death in transplant patients, particularly in the early post-transplant period, while cancer-related deaths were more frequent at later time points [36]. A study from the UK showed that the 3 most common causes of death in older transplant recipients were cardiac-related conditions (21%), infection (21%), and malignancy (20%) [37]. Therefore, careful patient selection is important to achieve better long-term outcomes.
Our study had some limitations. The first is the retrospective nature of the study; however, the data collection was thorough and complete, as all patients were followed up at our center. Second, we did not include a control group in this study, so it was not possible to compare the outcomes of elderly patients with those of young recipients. A better comparison could have been made with the patients who remained active on the waiting list. However, previous studies have shown clear benefits of transplantation over other RRT methods. Our study is unique because young donors donated kidneys to elderly recipients. As the outcomes of elderly recipients were reasonably good, this seems to be a justified practice.
Conclusions
In conclusion, the present study showed good short- and long-term outcomes of older patients who received kidneys from young donors. The outcomes in our cohort were significantly better in the LD group than in the DD group. Therefore, young people should be encouraged to donate their kidneys to older patients.
Figures
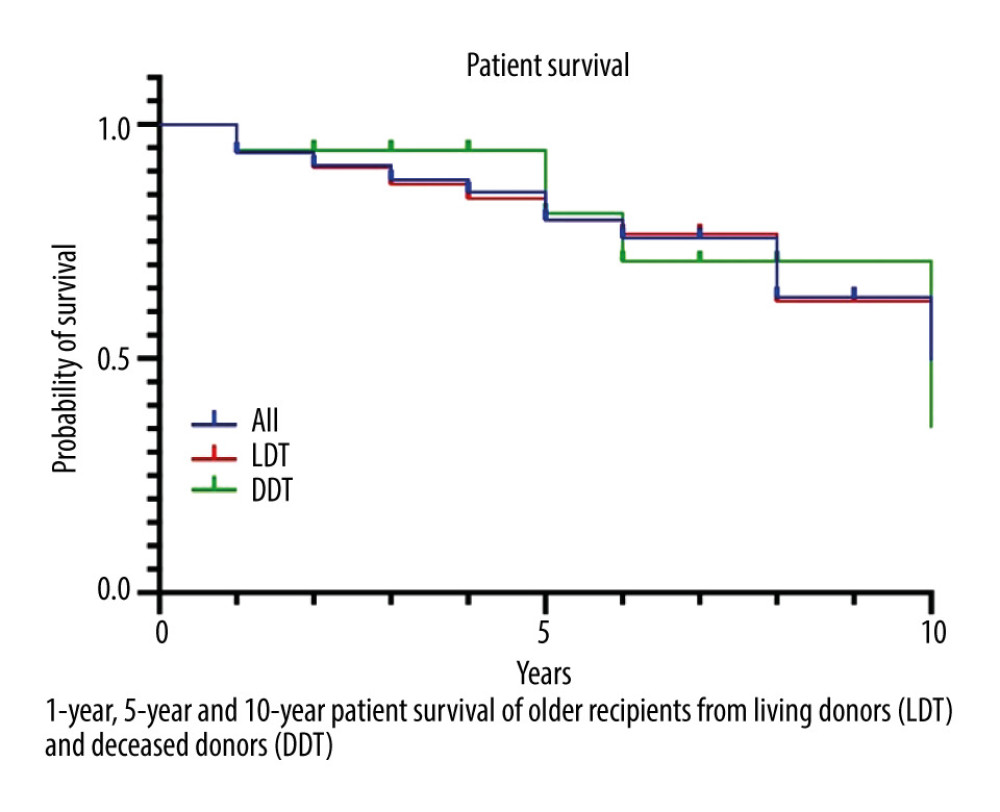 Figure 1. Patient survival.
Figure 1. Patient survival. References
1. Saran R, Robinson B, Abbott KC, US renal data system 2017 annual data report: Epidemiology of kidney disease in the United States: Am J Kidney Dis, 2018; 71; A7
2. Dempster NJ, Ceresa CD, Aitken E, Kingsmore D, Outcomes following renal transplantation in older people: A retrospective cohort study: BMC Geriatr, 2013; 13; 79
3. Knoll GA, Kidney transplantation in the older adult: Am J Kidney Dis, 2013; 61; 790-97
4. Wachterman MW, O’Hare AM, Rahman OK, One-year mortality after dialysis initiation among older adults: JAMA Intern Med, 2019; 179; 987-90
5. Johansen KL, Chertow GM, Jin C, Kutner NG, Significance of frailty among dialysis patients: J Am Soc Nephrol, 2007; 18; 2960-67
6. Cook WL, Jassal SV, Prevalence of falls among seniors maintained on hemodialysis: Int Urol Nephrol, 2005; 37; 649-52
7. Murray AM, Tupper DE, Knopman DS, Cognitive impairment in hemodialysis patients is common: Neurology, 2006; 67; 216-23
8. Griva K, Davenport A, Harrison M, Newman SP, The impact of treatment transitions between dialysis and transplantation on illness cognitions and quality of life – a prospective study: Br J Health Psychol, 2012; 17; 812-27
9. Oniscu GC, Brown H, Forsythe JL, How great is the survival advantage of transplantation over dialysis in elderly patients?: Nephrol Dial Transplant, 2004; 19; 945-51
10. Wong G, Howard K, Chapman JR, Comparative survival and economic benefits of deceased donor kidney transplantation and dialysis in people with varying ages and co-morbidities: PLoS One, 2012; 7; e29591
11. Lønning K, Heldal K, Bernklev T, Improved health-related quality of life in older kidney recipients 1 year after transplantation: Transplant Direct, 2018; 4; e351
12. Curtis JJ, Ageism and kidney transplantation: Am J Transplant, 2006; 6; 1264-66
13. Albugami MM, Panek R, Soroka S, Access to kidney transplantation: Outcomes of the non-referred: Transplant Res, 2012; 1; 22
14. Stevens KK, Woo YM, Clancy M, Deceased donor transplantation in the elderly – are we creating false hope?: Nephrol Dial Transplant, 2011; 26; 2382-86
15. Solez K, Colvin RB, Racusen LC, Banff 2005 Meeting Report. Banff ‘05 Meeting Report: Differential diagnosis of chronic allograft injury and elimination of chronic allograft nephropathy (‘CAN’): Am J Transplant, 2007; 7; 518-26
16. Solez K, Colvin RB, Racusen LC, Banff 07 classification of renal allograft pathology: updates and future directions: Am J Transplant, 2008; 8; 753-60
17. Haas M, Loupy A, Lefaucheur C, The Banff 2017 Kidney Meeting Report: revised diagnostic criteria for chronic active T cell-mediated rejection, antibody-mediated rejection, and prospects for integrative endpoints for next-generation clinical trials: Am J Transplant, 2018; 18; 293-307
18. Loupy A, Haas M, Roufosse C, The Banff 2019 kidney meeting Report (I) : Updates on and clarification of criteria for T cell- and antibody-mediated rejection [report]: Am J Transplant, 2020; 20; 2318-31
19. Saran R, Robinson B, Abbott KC, US renal data system 2019 annual data report: Epidemiology of kidney disease in the United States: Am J Kidney Dis, 2020; 75; A6-A7
20. Jassal SV, Trpeski L, Zhu N, Changes in survival among elderly patients initiating dialysis from 1990 to 1999: CMAJ, 2007; 177; 1033-38
21. Coresh J, Astor BC, Greene T, Prevalence of chronic kidney disease and decreased kidney function in the adult US population: third National Health and Nutrition Examination Survey: Am J Kidney Dis, 2003; 41; 1-12
22. Gupta R, Woo K, Yi JA, Epidemiology of end-stage kidney disease: Semin Vasc Surg, 2021; 34; 71-78
23. Hernández D, Alonso-Titos J, Armas-Padrón AM, Mortality in elderly waiting-list patients versus age-matched kidney transplant recipients: Where is the risk?: Kidney Blood Press Res, 2018; 43; 256-75
24. Fabrizii V, Winkelmayer WC, Klauser R, Patient and graft survival in older kidney transplant recipients: Does age matter?: J Am Soc Nephrol, 2004; 15; 1052-60
25. Rakké YS, Laging M, Kal-van Gestel JA, What happens to elderly patients on the waiting list for a renal transplantation? Transpl: Immunol, 2014; 31; 257
26. Lentine KL, Smith JM, Hart A, OPTN/SRTR 2020 Annual Data Report: Kidney: Am J Transplant, 2022; 22(Suppl 2); 21-136
27. Ozkul F, Erbis H, Yilmaz VT, Effect of age on the outcome of renal transplantation: A single-center experience: Pak J Med Sci, 2016; 32; 827-30
28. Yenifer SA, Nasly PA, Andrea GL, Fernando GL, Patient and graft survival of elderly kidney transplant recipients: A ten years follow-up: Transplantation, 2020; 104; S630-31
29. Ifudu O, Mayers J, Matthew J, Dismal rehabilitation in geriatric inner-city hemodialysis patients: JAMA, 1994; 271; 29-33
30. Foote C, Kotwal S, Gallagher M, Survival outcomes of supportive care versus dialysis therapies for elderly patients with end-stage kidney disease: A systematic review and meta-analysis: Nephrology (Carlton), 2016; 21; 241-53
31. Al-Sayyari A, Shaheen F, End stage chronic kidney disease in Saudi Arabia. A rapidly changing scene: Saudi Med J, 2011; 32(4); 339-46
32. Murphy S, Kochanek K, Xu J, Arias E, Mortality in the United States, 2020: NCHS Data Brief, 2021(427); 1-8
33. Tegzess E, Gomes Neto AW, Pol RA, Comparative survival of elderly renal transplant recipients with a living donor versus a deceased donor: A retrospective single center observational study: Transpl Int, 2021; 34; 2746-54
34. Hiramitsu T, Tomosugi T, Futamura K, Adult living-donor kidney transplantation, donor age, and donor-recipient age: Kidney Int Rep, 2021; 6; 3026-34
35. Lloyd-Jones D, Adams R, Carnethon M, Heart disease and stroke statistics--2009 update: A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee: Circulation, 2009; 119; 480-86
36. Ying T, Shi B, Kelly PJ, Death after kidney transplantation: An analysis by era and time post-transplant: J Am Soc Nephrol, 2020; 31; 2887-99
37. Karim A, Farrugia D, Cheshire J, Recipient age and risk for mortality after kidney transplantation in England: Transplantation, 2014; 97; 832-38
Figures
In Press
15 Mar 2024 : Review article
Approaches and Challenges in the Current Management of Cytomegalovirus in Transplant Recipients: Highlighti...Ann Transplant In Press; DOI: 10.12659/AOT.941185
18 Mar 2024 : Original article
Does Antibiotic Use Increase the Risk of Post-Transplantation Diabetes Mellitus? A Retrospective Study of R...Ann Transplant In Press; DOI: 10.12659/AOT.943282
20 Mar 2024 : Original article
Transplant Nephrectomy: A Comparative Study of Timing and Techniques in a Single InstitutionAnn Transplant In Press; DOI: 10.12659/AOT.942252
28 Mar 2024 : Original article
Association Between FEV₁ Decline Rate and Mortality in Long-Term Follow-Up of a 21-Patient Pilot Clinical T...Ann Transplant In Press; DOI: 10.12659/AOT.942823
Most Viewed Current Articles
05 Apr 2022 : Original article
Impact of Statins on Hepatocellular Carcinoma Recurrence After Living-Donor Liver TransplantationDOI :10.12659/AOT.935604
Ann Transplant 2022; 27:e935604
12 Jan 2022 : Original article
Risk Factors for Developing BK Virus-Associated Nephropathy: A Single-Center Retrospective Cohort Study of ...DOI :10.12659/AOT.934738
Ann Transplant 2022; 27:e934738
22 Nov 2022 : Original article
Long-Term Effects of Everolimus-Facilitated Tacrolimus Reduction in Living-Donor Liver Transplant Recipient...DOI :10.12659/AOT.937988
Ann Transplant 2022; 27:e937988
15 Mar 2022 : Case report
Combined Liver, Pancreas-Duodenum, and Kidney Transplantation for Patients with Hepatitis B Cirrhosis, Urem...DOI :10.12659/AOT.935860
Ann Transplant 2022; 27:e935860