07 April 2023: Original Paper
Postoperative Outcomes in 415 Patients Following Liver Transplantation Using Extended Donor Criteria: A Study from a Single Center in Germany
Aladdin Ali Deeb1ACE*, Utz Settmacher1D, Johannes Fritsch1BC, Felix Dondorf1AD, Oliver Rohland1F, Falk Rauchfuß1DEDOI: 10.12659/AOT.939060
Ann Transplant 2023; 28:e939060
Abstract
BACKGROUND: Because of the massive organ shortage worldwide, marginal organs are increasingly being considered. The aim of this study was to present a comprehensive analysis of donor-related factors clinically supposed to influence the outcome after liver transplantation. This study from a single center in Germany aimed to evaluate postoperative outcomes in 415 patients following liver transplantation using extended donor criteria.
MATERIAL AND METHODS: Extended donor criteria (EDC) were considered according to the official guidelines issued through the German Medical Association. Other factors and the Eurotransplant Donor Risk Index (ET-DRI) were also considered. Correlation studies, logistic regression, and Kaplan-Meier-estimator were used to evaluate the outcome.
RESULTS: The postoperative outcomes with or without EDC were comparable. Other factors had an impact on early allograft failure (EAD), including male donors (χ²=14.135, P=0.0001). Other donor-unrelated factors, like cold ischemia time, also had an impact on EAD (r=0.135, P=0.010), especially in patients with model for end-stage liver disease (MELD) <25 (β=0.001, P=0.008). ET-DRI was a crucial factor in estimating overall and allograft survival after liver transplantation.
CONCLUSIONS: The findings from this study support the possibility of liver transplantation using organs obtained by EDC. Other factors, like donor sex and cold ischemic time, are not part of the EDC, although they have an impact on EAD. Organs obtained by EDC continue to be an option to address the organ shortage.
Keywords: cold ischemia, Liver Transplantation, Humans, Male, End stage liver disease, Severity of Illness Index, Tissue Donors, Germany, Graft Survival, Risk Factors, Treatment Outcome
Background
Since the first liver transplantation by Thomas Starzl in 1963, many medical advances enable this to be a feasible procedure with remarkable benefits on overall survival and quality of life, liver transplantation is now the criterion standard therapy in many indications, from end-stage liver diseases and acute liver failure to benign and malignant liver tumors [1–3]. Expanding the indications for liver transplantation correlates, however, with an ever-growing worldwide shortage of donor grafts. Therefore, the transplant community is forced to take so-called marginal organs into account [4]. There is no worldwide consensus about the definition of a “marginal organ, synonym: organ with extended donor criteria, EDC” and controversies about the particular extended donor criteria appear clearly in the literature [5,6]. Furthermore, there is still no evidence-based strategy to evaluate allografts according to such criteria, although many studies addressed the EDC and its impact on organ survival after liver transplantation. Feng et al analyzed donor characteristics that significantly impact the outcome after liver transplantation in a large cohort [7]. This was validated by Block et al [8] and then developed as the Donor Risk Index for Eurotransplant Region (ET-DRI) by Braat et al [9]. However, this has still not been implemented in the allocation of liver grafts in the Eurotransplant region and is just used for educational purposes.
Experience using EDC donation has increased because of the organ shortage, and it is meaningful to put the EDC as used into question to better understand their impact on organ quality. The liver donor pool could thus be expanded, with comparable postoperative outcomes after liver transplantation.
Therefore, this study from a single center in Germany aimed to evaluate postoperative outcomes in 415 patients following liver transplantation using extended donor criteria and to present a comprehensive analysis of the currently used extended donor criteria for liver grafts in Germany and other donor-related factors clinically supposed to influence the outcome after liver transplantation.
Material and Methods
PATIENTS:
Patient consent for data collection and analysis was obtained before registration on our waiting list. The study is registered and approved by the Ethics Committee of Friedrich-Schiller-University, Jena on 12.05.2015 under the following code (4428-05/15). Between 2007 and 2019, a total of 689 adults patients underwent liver transplantation in our center. All donations were after brain death since donation after circulatory death is not allowed by law in Germany. Exclusion criteria were as follows: combined organ transplantation, partial liver graft, and retransplantation. Recipients with “High Urgent – HU” status were excluded since the outcome could be more affected by the underlaying concomitant disease than through EDC. HU-status is indicated for patients with acute life-threatening liver failure without pre-existing liver disease. A chronic liver disease does not justify HU-status, such as acute-on-chronic liver failure. For the same reason, patients who developed a surgical technical complication after transplantation were also excluded. A total of 274 liver transplantations were excluded and 415 were analyzed (Figure 1). Data collection and analysis were performed retrospectively after patient consent. As part of registration on the waiting list for liver transplantation, the patients were informed about the possibility of using EDC liver grafts. Only patients with written consent could become eligible for EDC. To estimate the urgency of liver transplantation, the model for end-stage liver disease (MELD) score was used [10] . Na-MELD has no clinical role in Germany, therefore it was not considered. We considered the rules according to the official guidelines issued through the German Medical Association, in which MELD score must be upgraded after 12 months in case of MELD ≤10, after 3 months in case of MELD ≤11 to ≤18, after 1 month in case of MELD >18 to ≤25, and after 1 week in case of MELD ≥25. However, lab-MELD is not the only priority estimating factor in organ allocation, since there is so-called “exceptional MELD” according to Eurotransplant [11]. This exceptional MELD results in “standard exception - SE” or “nonstandard exception - NSE” rules in organ allocation. For specific disease situations in which the severity of disease is not reflected in MELD, SE criteria are precisely defined by the German Medical Association [12]. In any other undefined similar situation, a request “NSE” could be sent to Eurotransplant to acquire an exceptional MELD. There were122 patients transplanted with exceptional MELD score; 102 with SE (79 with HCC, 15 with polycystic degeneration, 8 with primary sclerosing cholangitis “PSC”), and 20 with NSE.
All liver transplantations were performed according to our center standard. A standardized surgical approach and postoperative immunosuppression were preformed according to center protocols.
EXTENDED DONOR CRITERIA:
The extended donor criteria are described in the official guidelines issued through the German Medical Association [12]. Accordingly, EDC are divided into general criteria, which are valid for all types of organs: own history of malignancy, drug abuse, viral hepatitis, sepsis, and meningitis, and liver specific criteria: age >65 years old, intensive care unit stay >7 days, obesity (BMI >30 kg/m2), microvesicular hepatic steatosis (>40%) proven by frozen section parallel to the continuation of the organ retrieval, serum sodium >165 mmol/l, serum GOT or GPT >3×cutoff value and serum bilirubin >3 mg/dl. Fulfilling at least 1 of any these, the organ must be declared a marginal organ. Furthermore, the sum of EDC, which the donor fulfills, was analyzed as an ordinal scaled variable. We called this sum the “EDC score”, since there is EDC score. It is simply defined as the sum of EDC, which the donor fulfills. This score is used only for scientific purposes, not clinically. Thereafter, other criteria that could influence the outcome after transplantation were analyzed: donor resuscitation, donor’s sex, and cold ischemia time. A precise period of donor resuscitation was lacking in donor reports, which is why this was analyzed only in the nominal scale. Cold ischemia time was defined as the period from the beginning of intracorporal allograft perfusion in donor until the beginning of intracorporal allograft implantation in recipient.
ENDPOINTS:
To explore the impact of EDC-incidence on outcome after liver transplantation, a primary endpoint called “allograft failure” was considered. This was divided into acute and chronic allograft failure:
–
Allograft failure and each of its stratifications was considered as a composite or separate primary endpoint, respectively.
Early allograft dysfunction (EAD) was a secondary endpoint, defined as the presence of 1 or more of the following postoperative laboratory analyses reflective of liver injury and function: bilirubin ≥10 mg/dL on day 7, international normalized ratio ≥1.6 on day 7, and alanine or aspartate aminotransferases >2000 IU/L within the first 7 days [15].
Furthermore, we analyzed the impact of EDC on 90-day mortality and overall and allograft survival. Graft survival was censored to either death or retransplantation.
:
Braat et al described a donor risk index for the Eurotransplant region containing parameters that impair organ survival: age, cause of death, graft type, cold ischemia time, gamma glutamyl transpeptidase (GGT), donor location, and allocation type. ET-DRI was considered in the correlation the same as in overall and organ survival studies. We used the formula:
According to Braat et al, lower ET-DRI is associated with better outcomes after liver transplantation. Nevertheless, ET-DRI is still used only for educational purposes, not clinically.
STATISTICAL STUDIES:
Statistical analysis was performed with IBM SPSS Statistics 25 software (IBM, Armonk, New York, USA). To prove causality, we used the Pearson’s chi-square test (χ2) and Fisher’s exact test for categorical variables (EDC yes/no, EDC score sum, Age > 65 years old, ICU stay >7 days, BMI >30 kg/m2, sNa 165 mmol/, sGOT/sGPT > 3× cutoff value, viral hepatitis yes/no, resuscitation, and donor’s sex). Pearson’s and Spearman’s tests were used in correlation studies. Spearman’s correlation was used for nominal/ordinal variables (Age, ICU stay, BMI, sNa, sGPT, sBilirubin, and cold ischemia time). To determine how large the correlation is, we referred to Cohen’s classification (1992) as follows:
Kaplan-Meier-estimator was used in overall and organ survival studies. The log rank test was used to compare survival. Thereafter, multivariate analysis was performed. In this part of the study, EAD was considered a dependent variable. We considered independent variables that previously showed statistical significance. A MELD stratification was done, since the pretransplantation recipient’s state could also have an influence on allograft dysfunction. ROC analysis was used to determine a valid ET-DRI cutoff for the study cohort. A linear regression model was used, using the Gauss–Markov theorem. The significance level was determined with a P value <0.05.
Results
Descriptive Studies
RECIPIENTS: We included 415 recipients, with a median age of 58 years (range: 25–76). Figure 1 shows the derivation of our study cohort. Table 1 shows the demographics of the included recipients; 300 patients were male (72.3%) and 115 were female (27.7%). The median waiting time to transplantation was 159 days (<1 to 4685). The most common cause of transplantation was alcoholic cirrhosis (229, 55.2%), and 142 (34.2%) had a hepatocellular carcinoma. There were other causes of end-stage liver disease, as shown in Table 1. The median lab-MELD was 17 (6 to 40); 161 (38.8%) patients had a MELD ≥25, 29 (7%) had MELD ≥19 to 24, 109 (26.3%) had MELD ≥11 to 18, and 116 (28%) had MELD ≤10. Patients with lower MELD scores were mostly allocated through the above-mentioned exceptional MELD rules; 122 patients were transplanted with exceptional MELD score; 102 with SE (79 with HCC, 15 with polycystic degeneration, and 8 and 20 with NSE.
DONORS: Table 2 shows the incidence of described EDC through German Medical Association and other related factors in the study cohort. Accordingly, only 81 (19.5%) donors did not have any of EDC. Otherwise, the incidence of EDC score was as follow: EDC(1) in 206 (49.6%), EDC(2) in 92 (22.2%), EDC(3) in 31 (7.5%), and EDC(4) in 5 (1.2%) patients.
DEFINED EDC THROUGH GERMAN MEDICAL ASSOCIATION: Table 3 shows an overview of the incidence of defined endpoints and correlated chi-square-test (χ2) in the case of at least 1 EDC. Some EDC were excluded from the analysis for statistical reasons when its incidence was seen in less than 10 donors. Considering EDC score, there was no statistically significant correlation between these and the defined endpoints after liver transplantation. However, when the EDC are considered separately, only donor’s age and ICU stay seem to have a statistically significant correlation with ITBL (P=0.0004) and EAD (P=0.009), respectively. Furthermore, the interval-scalable EDC were reanalyzed and considered as categorical variables and not as nominal variables based on the defined cutoff values. Thereby, the correlation between donor’s age and incidence of ITBL seemed statistically significant too (r=0.174, P=0.0004). ICU stay and EAD were correlated significantly (r=0.138, P=0.005). Donor’s BMI and sGPT, which before showed no correlation considering the predefined cutoff values, were also correlated with EAD (r=0.145, P=0.003) and (r=0.121, P=0.014), respectively. Importantly, EAD was correlated with worse organ survival in the study collective (P=0.003) (Figure 2). All other survival studies did not show any correlation between EDC and outcome after transplantation.
OTHER FACTORS:
Donor resuscitation had no correlation with outcome after liver transplantation. Interestingly, donor’s male sex was significantly correlated with EAD incidence after transplantation (χ2=14.135, P=0.0001). On the other hand, sex mismatch was not significant after being combined with more EAD incidence (χ2=3.965, P=0.055). Consequently, the male-to-female donor/recipient sex status was combined with most EAD incidence (χ2=8.9, P=0.003), which supports the finding that male donor sex is the crucial factor beyond sex mismatch. Cold ischemia time showed a significant correlation with incidence of EAD (r=0.135, P=0.010).
MULTIVARIATE ANALYSIS: Table 4 shows the correlation between EAD as a dependent variable and the independent variables, which showed a statistical significance in the previous correlation studies (3.2.). It is remarkable that the influence of the involved independent variables varies substantially when MELD is considered. This refers to the rule of preoperative recipient’s state on allograft dysfunction. This phenomenon could be influenced through the significant difference (χ2=36.483, P=0.00027) in organ acceptance in the different MELD categories (Figure 3).
ET-DRI: The median ET-DRI was 2.0 (range: 1.1 to 2.82). Correlation studies showed a significant correlation between interval scaled ET-DRI and ITBL-incidence (r=0.116, P=0.029). Otherwise, there were no significant correlations with the other defined endpoints. Cutoff was defined at ET-DRI = 1.9050 through ROC analysis considering ITBL as the endpoint. This cutoff meets a sensitivity of 93.8%. Accordingly, 42.3% of donors had an ET-DRI <1.9050 and 57.7 ET-DRI >1.9050. Consequently, correlation studies were performed between nominal scaled ET-DRI, considering the defined cutoff, and the described endpoints. This showed a significant correlation between ET-DRI and allograft failure (AF) in general (r=0.110, P=0.039), and especially with ITBL (r=0.159, P=0.003). Kaplan-Meier-estimator showed a difference in overall and organ survival considering ET-DRI, which were significant in log rank test (χ2=5.693, P=0.017) and (χ2=5.045, P=0.025), respectively (Figures 4, 5).
Discussion
Mortality on waiting lists is increasing worldwide [16]. According to the German Foundation for Organ Transplantation, a total of 826 livers were transplanted in year 2020, while 1413 patients were registered for liver transplantation and 226 patients died on the waiting list in the same year [17]. The use of organs obtained by EDC is needed to meet the demand, which is reflected in this study, as over 80% of the used grafts did have at least 1 EDC. The current literature concerning this matter is nevertheless not promising and unfortunately is sparce and conflicting. Many single-center experiences suggest that the use of organs obtained by EDC could have an additional risk of delayed allograft function [18,19], while others, like Schemmer et al, suggest that EDC has no negative impact on early outcome after liver transplantation [5].
In this study, we present a comprehensive single-center experience of a large series of patients who underwent a liver transplantation, mostly from donor’s with at least 1 EDC according to the German Medical Association. More than 80% of donors included in this study had at least 1 EDC. This reflects the urgent demand for these organs to cover organ scarcity on the waiting list. Only deceased donations after brain death, and only single primary whole-organ liver transplantations were included. In general, the early outcomes after donation – defined through the acute liver failure or 90 days mortality – with or without EDC were comparable. This is contrary to the situation in clinical practice, in which such organs could be used only after patient consent. Further factors were analyzed, like resuscitation of donor and donor’s sex, which generally also had comparable outcomes. However, there were some limitations to explore each EDC separately. An important one was the limited incidence of some EDCs. This was due to the organ acceptance policy in our center. We have a strict policy regarding some criteria, like history of malignancy, sepsis, meningitis, severe hepatic steatosis, elevated bilirubin, and history of drug addiction. Such organs would be accepted individually only in rescue situations according to risk-benefit assessment. However, some EDC (donor age, ICU stay, BMI, sGPT, CIT, and male sex) seemed to have a negative impact on some defined endpoints (ITBL and EAD), when these were analyzed separately. The most distinct one was the donor’s age, which correlates significantly with the incidence of “ischemic type biliary lesions – ITBL”. This point disagrees with many experiences suggesting that using elderly liver allografts does not impair the outcome following transplantation [20–22]. To evaluate the outcome after liver transplantation, EAD [15] is an appropriate variable in the study cohort, since this correlates with worse organ survival according to Kaplan-Meier-estimator. Therefore, EAD was a great concern in this study. We found that donor’s BMI, ICU stay, cold ischemia time, and, interestingly, donor’s sex were correlated with EAD. Male sex was correlated with EAD incidence. Lai et al described a similar effect in a systemic review of donor-to-recipient sex mismatch, which was a risk factor for poor graft survival after liver transplantation, and male-to-female mismatch was the worst constellation [23]. This disagrees with our finding, in which the male donor’s sex, beyond donor-to-recipient sex mismatch, is a risk factor for worse outcome after liver transplantation. In this way, sex is another controversy about donor criteria and its impact on outcome after liver transplantation.
In general, the above-mentioned results varied extremely in stratification according to MELD. Therefore, the preoperative recipient’s state should be considered too in dealing with the matter of organs obtained by EDC. In patients with MELD <25, only cold ischemia time and donor’s BMI seemed to correlate with EAD. In this context, a bias of getting organ with lower EDC for recipients with higher MELD was remarkable in our analysis, which could influence the analysis of EDC without considering the MELD category.
Braat et al described use of the Eurotransplant Donor Risk Index in liver transplantation [9]. Our findings support the effect of ET-DRI on allograft outcome after liver transplantation, since the overall and organ survival were significantly better in patients after donation with ET-DRI <1.9050. Although ET-DRI contains factors, most of these are not included in the current applicable EDC, and ET-DRI seems to have an important role in estimating liver allografts before transplantation. Factors like cause of death, type of graft, and type of allocation could have a crucial role in the allocation process. Despite all that, ET-DRI does not have a role in the clinical allocation process.
According to our study results, defined EDC in this form needs to be edited and improved based on prospective multicenter trials, and some EDC could perhaps be excluded, such as cured hepatitis B. Other EDC could be included such as sex. The predefined cutoff values could be edited, and other things should also be considered, such as cold ischemia time and recipient’s condition.
Finally, there are other adequate solutions to the dilemma of organ scarcity. Living donation is surely one of these but requires a huge effort and puts a healthy donor at potential risk. Machine perfusion is a current focus of attention because cold ischemia time is more important than all EDC. Furthermore, machine perfusion could be used to treat organs obtained by EDC, aiming to improve allograft dysfunction.
Conclusions
The findings from this study support the possibility of liver transplantation using organs obtained by EDC. Other factors like donor sex and cold ischemic time are not part of the EDC, but they have an impact on EAD. Organs obtained by EDC continue to be an option to address the organ shortage. Organs obtained by EDC could expand the liver donor pool, since outcomes after liver transplantation using organs with or without EDC are comparable. Nevertheless, prospective multicenter studies are required.
Figures
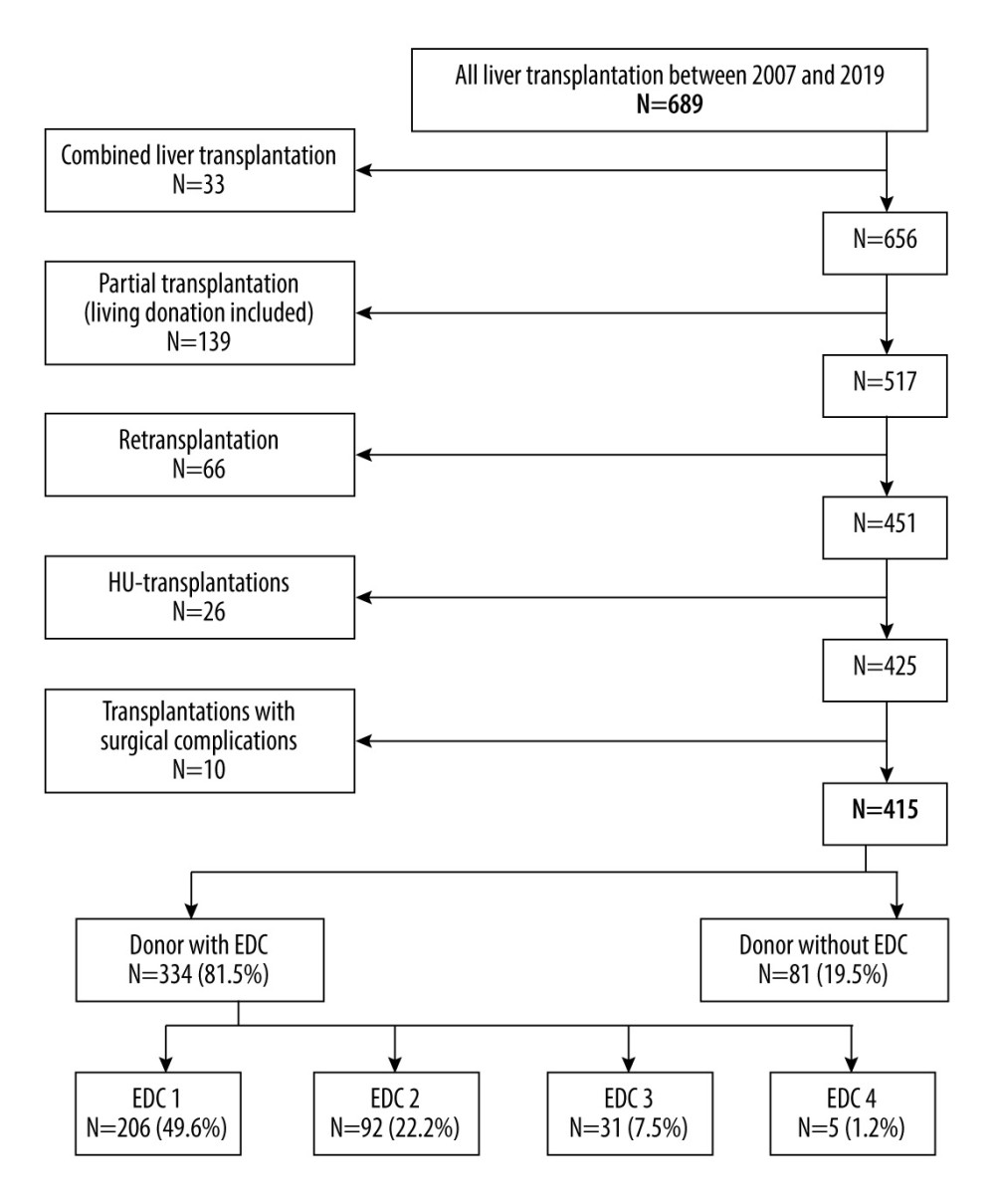 Figure 1. Flowchart showing the cohort derivation. EDC – extended donor criteria; HU – high urgency. Lucidchart: https://www.lucidchart.com/pages/examples/flowchart-maker.
Figure 1. Flowchart showing the cohort derivation. EDC – extended donor criteria; HU – high urgency. Lucidchart: https://www.lucidchart.com/pages/examples/flowchart-maker. 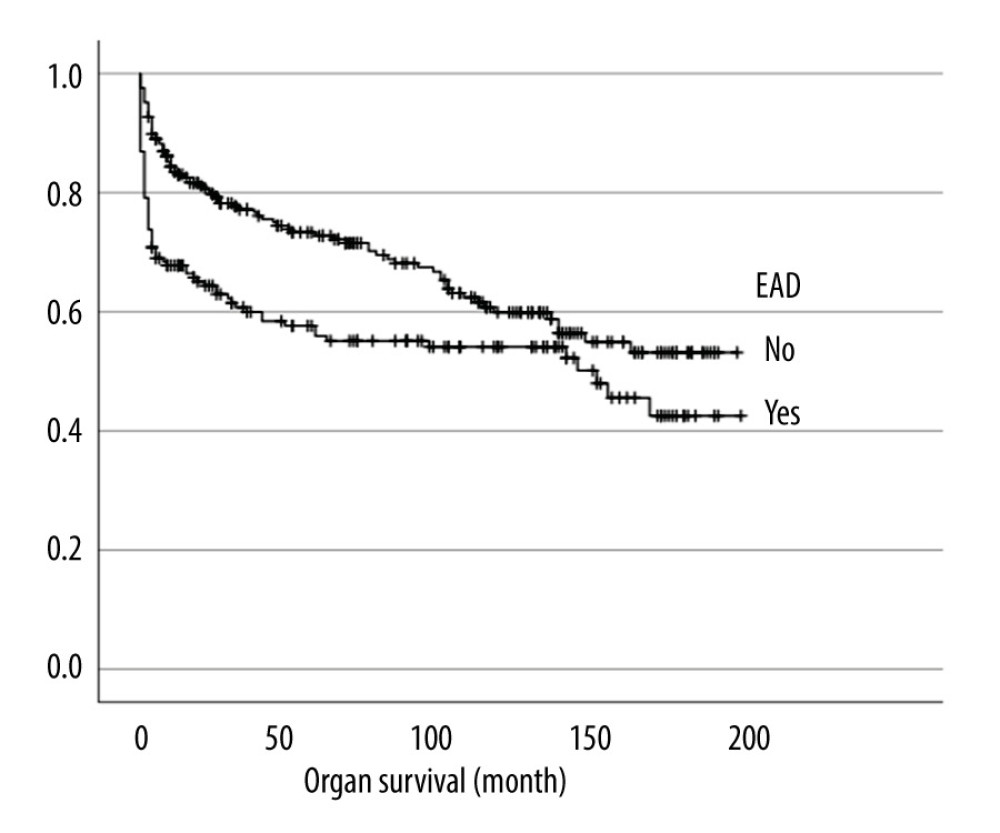 Figure 2. Impact pf early allograft dysfunction (EAD) on organ survival (P=0.003). EAD – early allograft dysfunction. IBM SPSS Statistics Version: 25.0.0.0 (IBM, Armonk, New York, USA).
Figure 2. Impact pf early allograft dysfunction (EAD) on organ survival (P=0.003). EAD – early allograft dysfunction. IBM SPSS Statistics Version: 25.0.0.0 (IBM, Armonk, New York, USA). 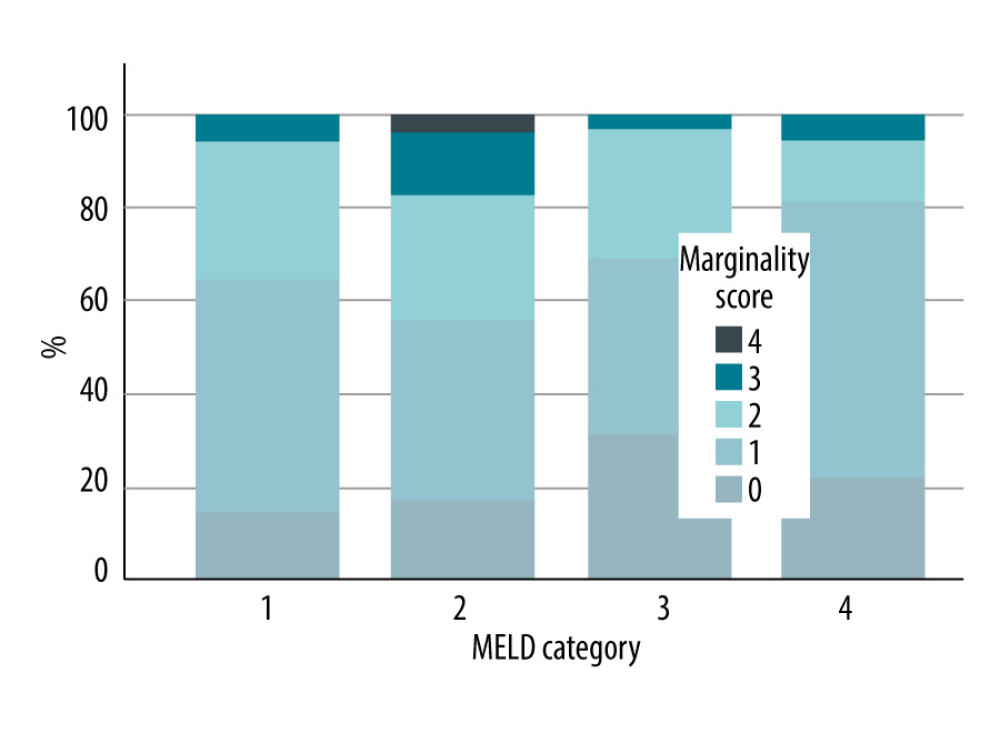 Figure 3. Distribution of EDC score in the different MRLD categories: Category 1: MELD ≤10; Category 2: MELD ≥11 to 18; Category 3: MELD ≥19 to 24; Category 4: MELD ≥25. EDC – extended donor criteria; MELD – model for end-stage liver disease. IBM SPSS Statistics Version: 25.0.0.0 (IBM, Armonk, New York, USA).
Figure 3. Distribution of EDC score in the different MRLD categories: Category 1: MELD ≤10; Category 2: MELD ≥11 to 18; Category 3: MELD ≥19 to 24; Category 4: MELD ≥25. EDC – extended donor criteria; MELD – model for end-stage liver disease. IBM SPSS Statistics Version: 25.0.0.0 (IBM, Armonk, New York, USA). 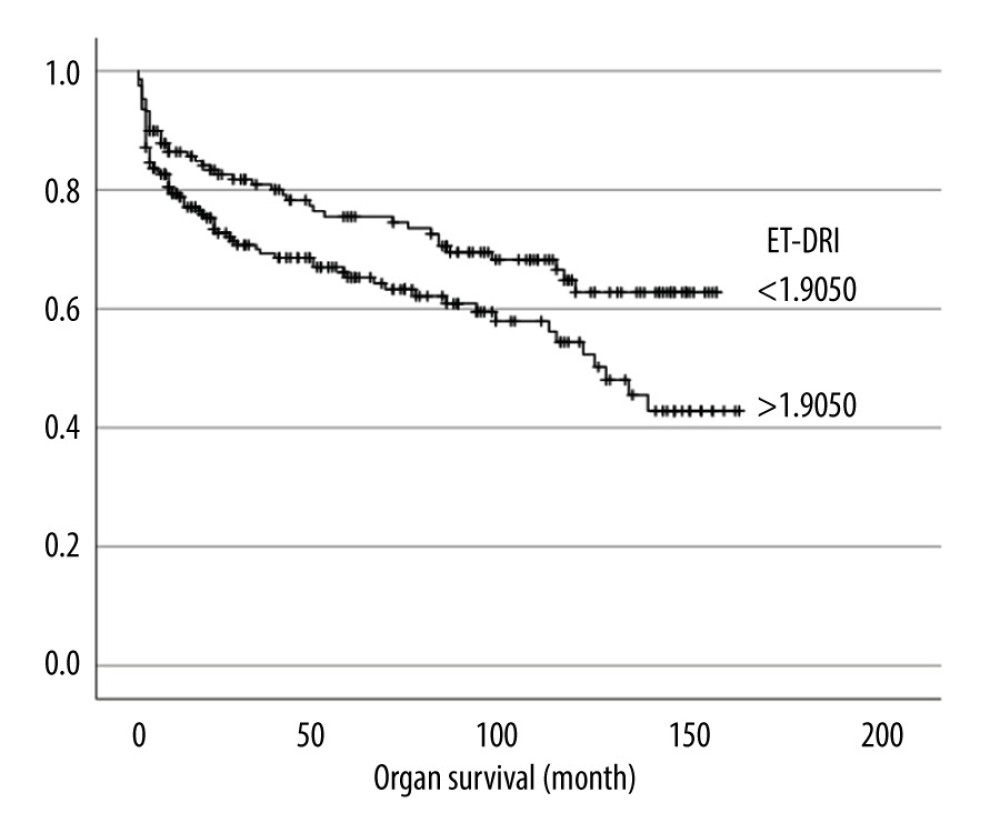 Figure 4. Overall survival in comparison based on Eurotransplant Donor Risk index (ET-DRI). IBM SPSS Statistics Version: 25.0.0.0 (IBM, Armonk, New York, USA).
Figure 4. Overall survival in comparison based on Eurotransplant Donor Risk index (ET-DRI). IBM SPSS Statistics Version: 25.0.0.0 (IBM, Armonk, New York, USA). 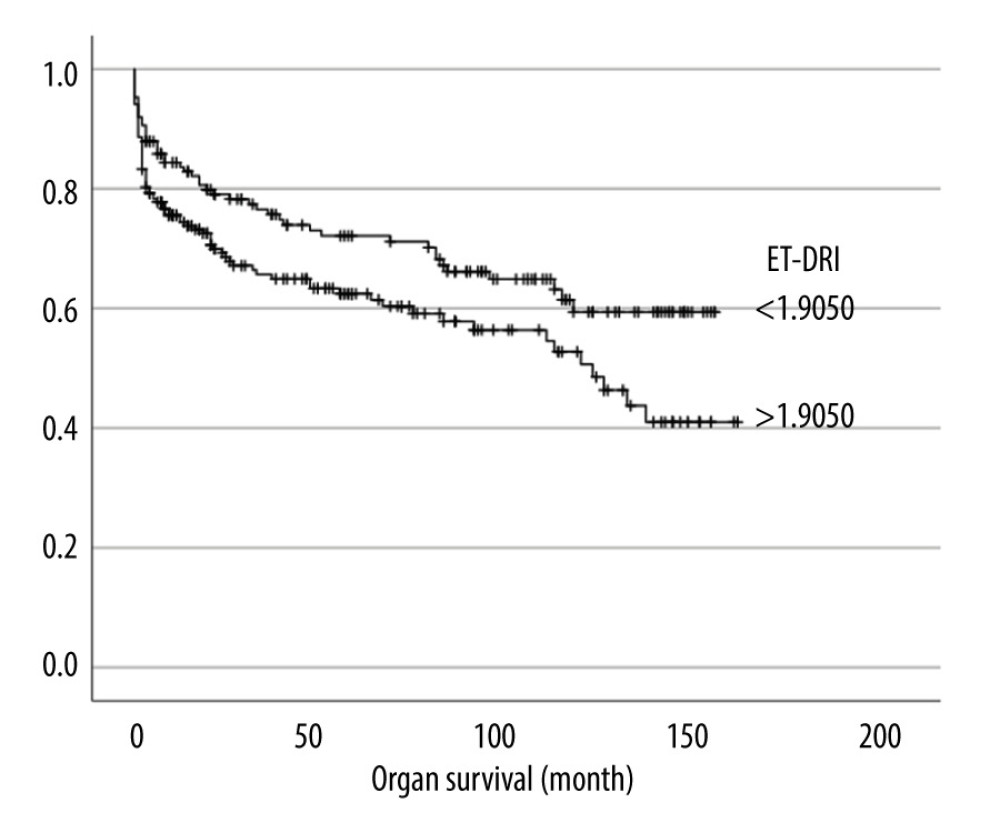 Figure 5. Organ survival in comparison based on Eurotransplant Donor Risk Index (ET-DRI). IBM SPSS Statistics Version: 25.0.0.0 (IBM, Armonk, New York, USA).
Figure 5. Organ survival in comparison based on Eurotransplant Donor Risk Index (ET-DRI). IBM SPSS Statistics Version: 25.0.0.0 (IBM, Armonk, New York, USA). References
1. Pichlmaye R, Indications for liver transplantation in hepatobiliary malignancy: Hepatology, 1994; 20(1); S33-S40
2. Molmenti EP, Klintmalm GB, Liver transplantation in association with hepatocellular carcinoma: An update of the International Tumor Registry: Liver Transpl, 2002; 8(9); 736-48
3. Dueland S, Syversveen T, Solheim JM, Survival following liver transplantation for patients with nonresectable liver-only colorectal metastases: Ann Surg, 2020; 271(2); 212-18
4. Agnes S, Avolio AW, Magalini SC, Marginal donors for patients on regular waiting lists for liver transplantation: Transplant Int, 1996; 9(Suppl 1); S469-S71
5. Schemmer P, Nickkholgh A, Hinz U, Extended donor criteria have no negative impact on early outcome after liver transplantation: A single-center multivariate analysis: Transplant Proc, 2007; 39(2); 529-34
6. Silberhumer GR, Pokorny H, Hetz H, Combination of extended donor criteria and changes in the Model for End-Stage Liver Disease score predict patient survival and primary dysfunction in liver transplantation: A retrospective analysis: Transplantation, 2007; 83(5); 588-92
7. Feng S, Goodrich NP, Bragg-Gresham JL, Characteristics associated with liver graft failure: The concept of a donor risk index: Am J Transplant, 2006; 6(4); 783-90
8. Blok JJ, Braat AE, Adam R, Validation of the donor risk index in orthotopic liver transplantation within the Eurotransplant region: Liver Transpl, 2012; 18(1); 112-19
9. Braat AE, Blok JJ, Putter H, The Eurotransplant donor risk index in liver transplantation: ET-DRI: Am J Transplant, 2012; 12(10); 2789-96
10. Malinchoc M, Kamath PS, Gordon FD, A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts: Hepatology, 2000; 31(4); 864-71
11. : Eurotransplant: An international non-profit organization. [ET Liver Allocation System (ELAS)]; 63 section 5.7.1.1. https://my.eurotransplant.org/wp-content/uploads/2022/10/H5-ELAS-MELD-October-2022.pdf
12. German Medical Association: Guideline according to § 16 paragraph 1 sentence 1 numbers 2 and 5 TPG for waiting list management and organ procurement for liver transplantation
13. Mazzaferro V, Regalia E, Doci R, Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis: N Engl J Med, 1996; 334(11); 693-99
14. Uemura T, Randall HB, Sanchez EQ, Liver retransplantation for primary nonfunction: Analysis of a 20-year single-center experience: Liver Transpl, 2007; 13(2); 227-33
15. Olthoff KM, Kulik L, Samstein B, Validation of a current definition of early allograft dysfunction in liver transplant recipients and analysis of risk factors: Liver Transpl, 2010; 16(8); 943-49
16. Jochmans I, van Rosmalen M, Pirenne J, Samuel U, Adult liver allocation in Eurotransplant: Transplantation, 2017; 101(7); 1542-50
17. German Foundation for Organ Transplantation: Annual report, 2020
18. Briceno J, Lopez-Cillero P, Rufian S, Impact of marginal quality donors on the outcome of liver transplantation: Transplant Proc, 1997; 29(1–2); 477-80
19. Mirza D, Gunson B, Da Silva R, Policies in Europe on “marginal quality” donor livers: Lancet, 1994; 344(8935); 1480-83
20. Chapman WC, Vachharajani N, Collins KM, Donor age-based analysis of liver transplantation outcomes: Short- and long-term outcomes are similar regardless of donor age: J Am Coll Surg, 2015; 221(1); 59-69
21. Gastaca M, Valdivieso A, Pijoan J, Donors older than 70 years in liver transplantation: Transplant Proc, 2005; 37(9); 3851-54
22. Rauchfuss F, Voigt R, Dittmar Y, Liver transplantation utilizing old donor organs: A German single-center experience: Transplant Proc, 2010; 42(1); 175-77
23. Lai Q, Giovanardi F, Melandro F, Donor-to-recipient gender match in liver transplantation: A systematic review and meta-analysis: World J Gastroenterol, 2018; 24(20); 2203-10
Figures
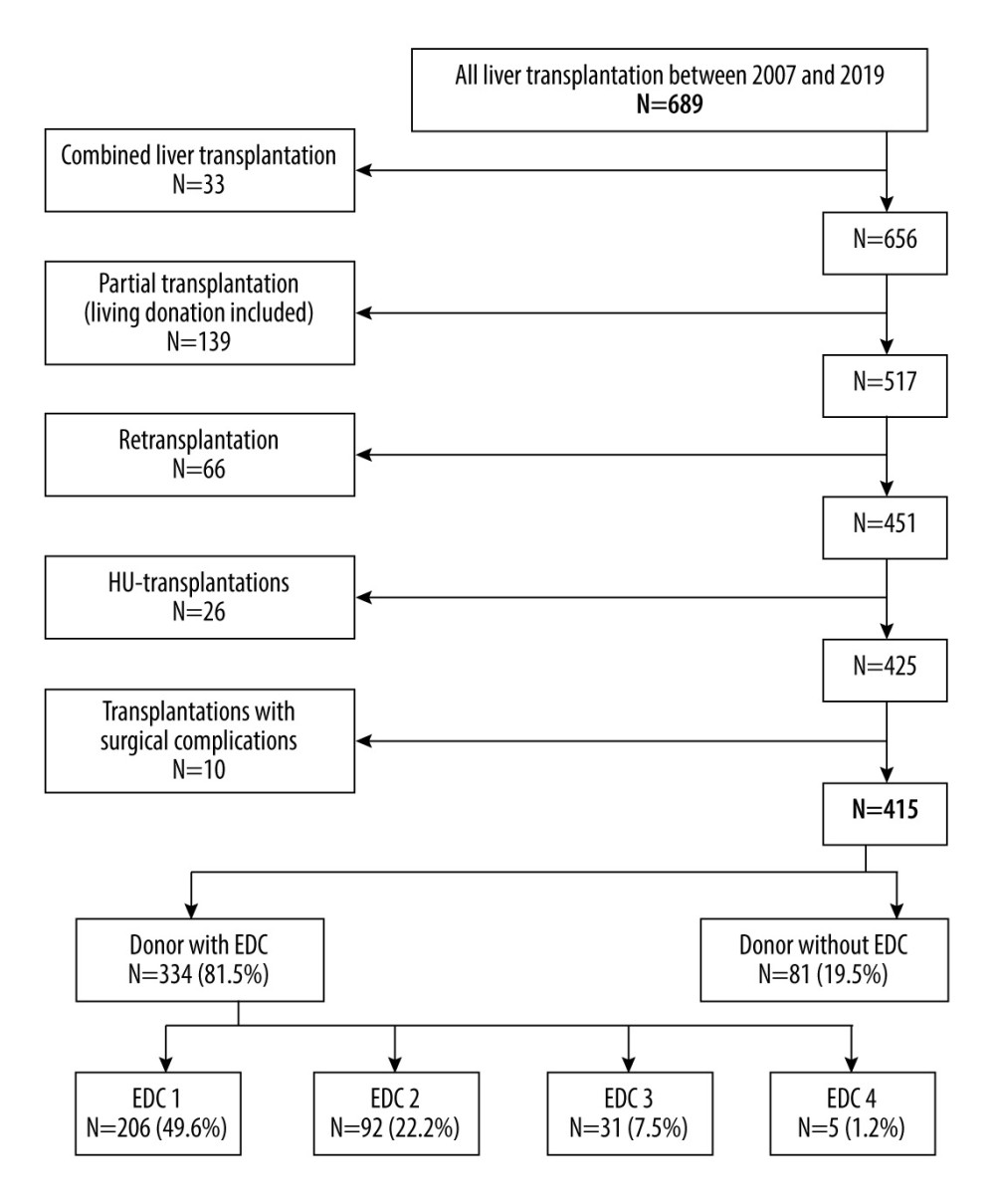 Figure 1. Flowchart showing the cohort derivation. EDC – extended donor criteria; HU – high urgency. Lucidchart: https://www.lucidchart.com/pages/examples/flowchart-maker.
Figure 1. Flowchart showing the cohort derivation. EDC – extended donor criteria; HU – high urgency. Lucidchart: https://www.lucidchart.com/pages/examples/flowchart-maker.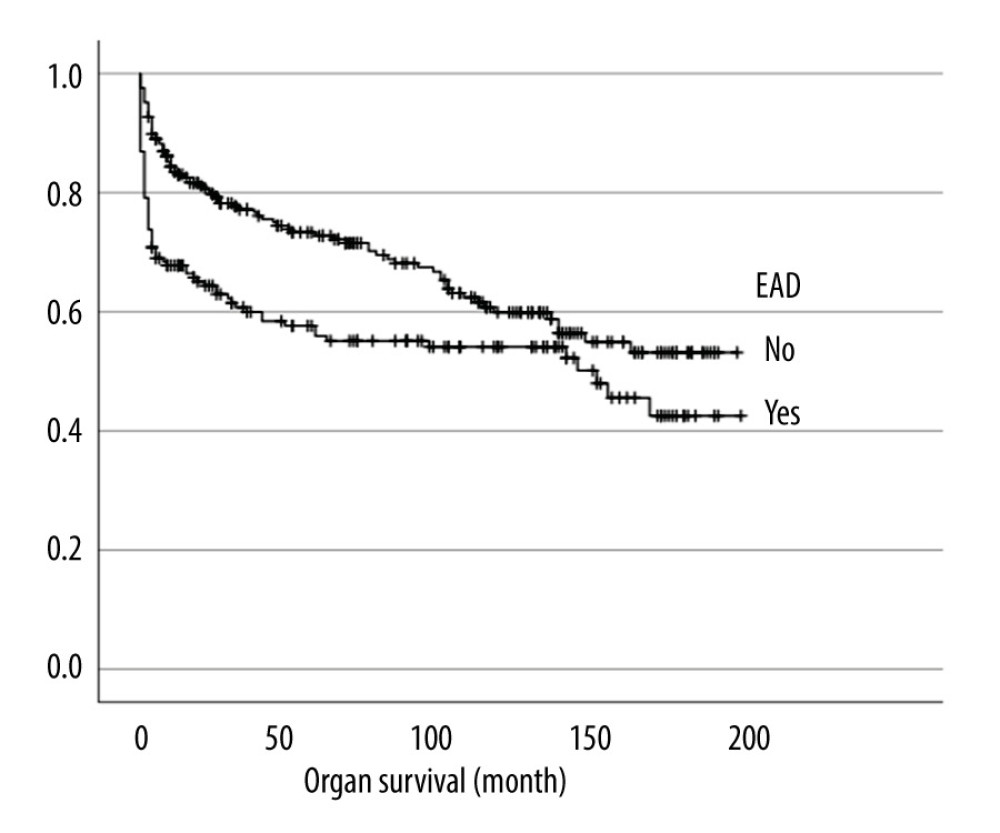 Figure 2. Impact pf early allograft dysfunction (EAD) on organ survival (P=0.003). EAD – early allograft dysfunction. IBM SPSS Statistics Version: 25.0.0.0 (IBM, Armonk, New York, USA).
Figure 2. Impact pf early allograft dysfunction (EAD) on organ survival (P=0.003). EAD – early allograft dysfunction. IBM SPSS Statistics Version: 25.0.0.0 (IBM, Armonk, New York, USA).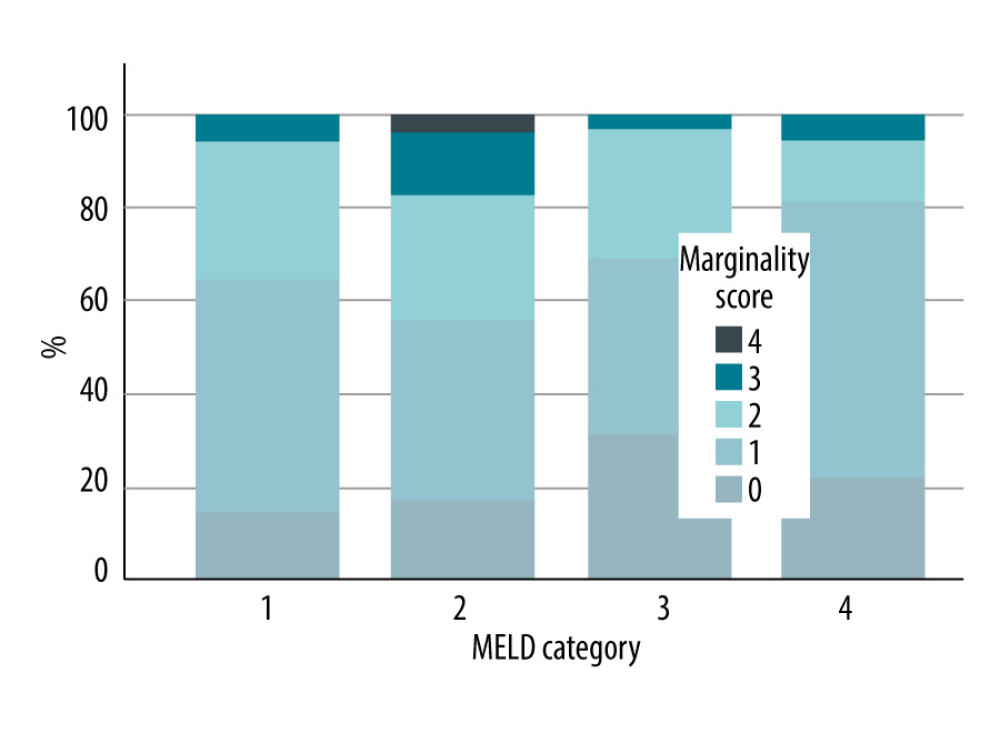 Figure 3. Distribution of EDC score in the different MRLD categories: Category 1: MELD ≤10; Category 2: MELD ≥11 to 18; Category 3: MELD ≥19 to 24; Category 4: MELD ≥25. EDC – extended donor criteria; MELD – model for end-stage liver disease. IBM SPSS Statistics Version: 25.0.0.0 (IBM, Armonk, New York, USA).
Figure 3. Distribution of EDC score in the different MRLD categories: Category 1: MELD ≤10; Category 2: MELD ≥11 to 18; Category 3: MELD ≥19 to 24; Category 4: MELD ≥25. EDC – extended donor criteria; MELD – model for end-stage liver disease. IBM SPSS Statistics Version: 25.0.0.0 (IBM, Armonk, New York, USA).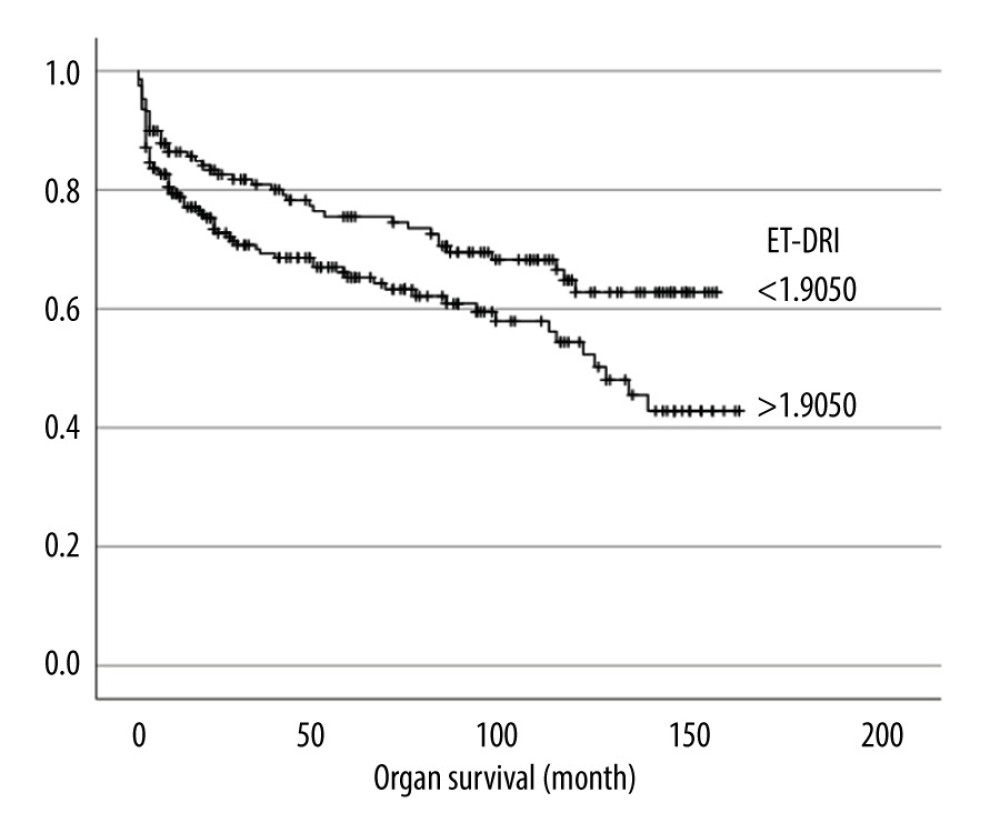 Figure 4. Overall survival in comparison based on Eurotransplant Donor Risk index (ET-DRI). IBM SPSS Statistics Version: 25.0.0.0 (IBM, Armonk, New York, USA).
Figure 4. Overall survival in comparison based on Eurotransplant Donor Risk index (ET-DRI). IBM SPSS Statistics Version: 25.0.0.0 (IBM, Armonk, New York, USA).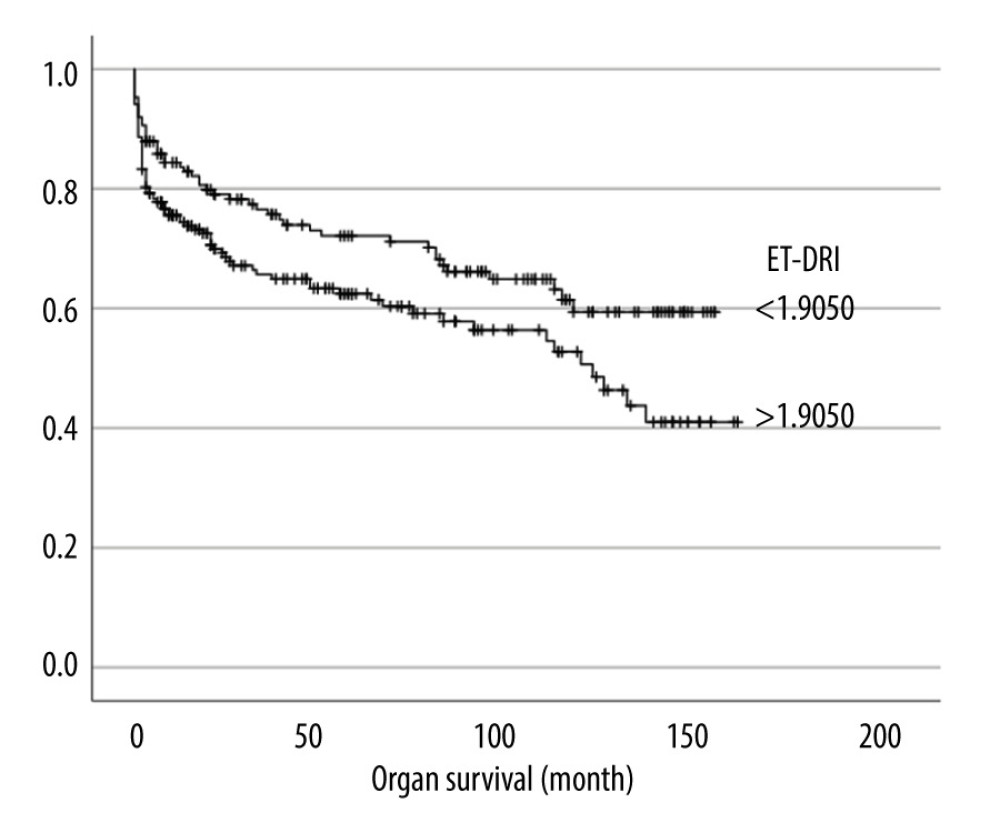 Figure 5. Organ survival in comparison based on Eurotransplant Donor Risk Index (ET-DRI). IBM SPSS Statistics Version: 25.0.0.0 (IBM, Armonk, New York, USA).
Figure 5. Organ survival in comparison based on Eurotransplant Donor Risk Index (ET-DRI). IBM SPSS Statistics Version: 25.0.0.0 (IBM, Armonk, New York, USA). Tables
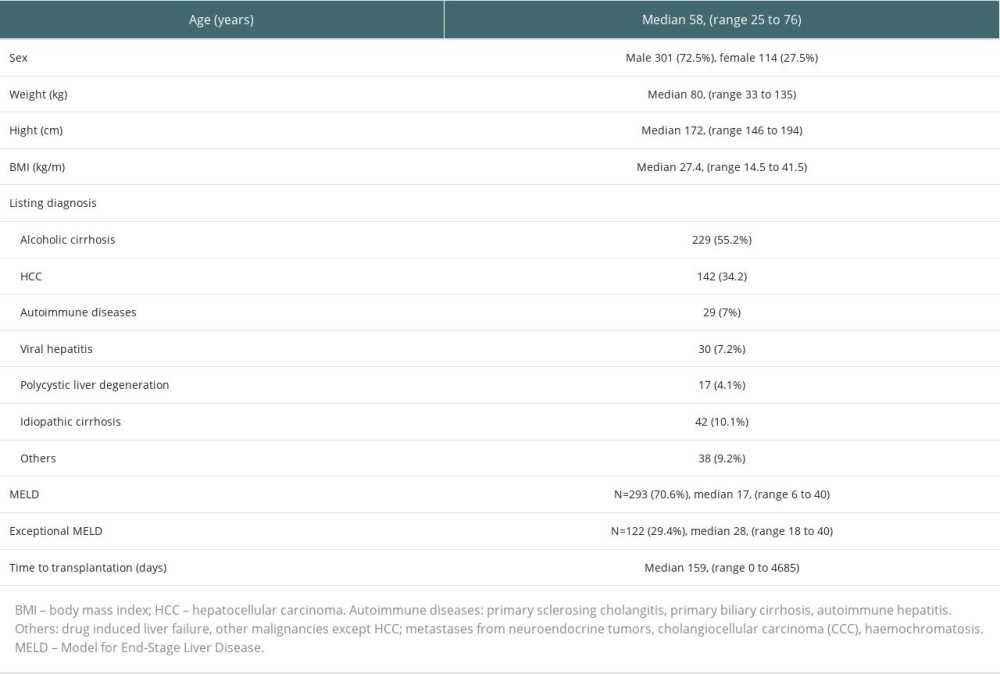 Table 1. Demographic results of all 415 included recipients.
Table 1. Demographic results of all 415 included recipients.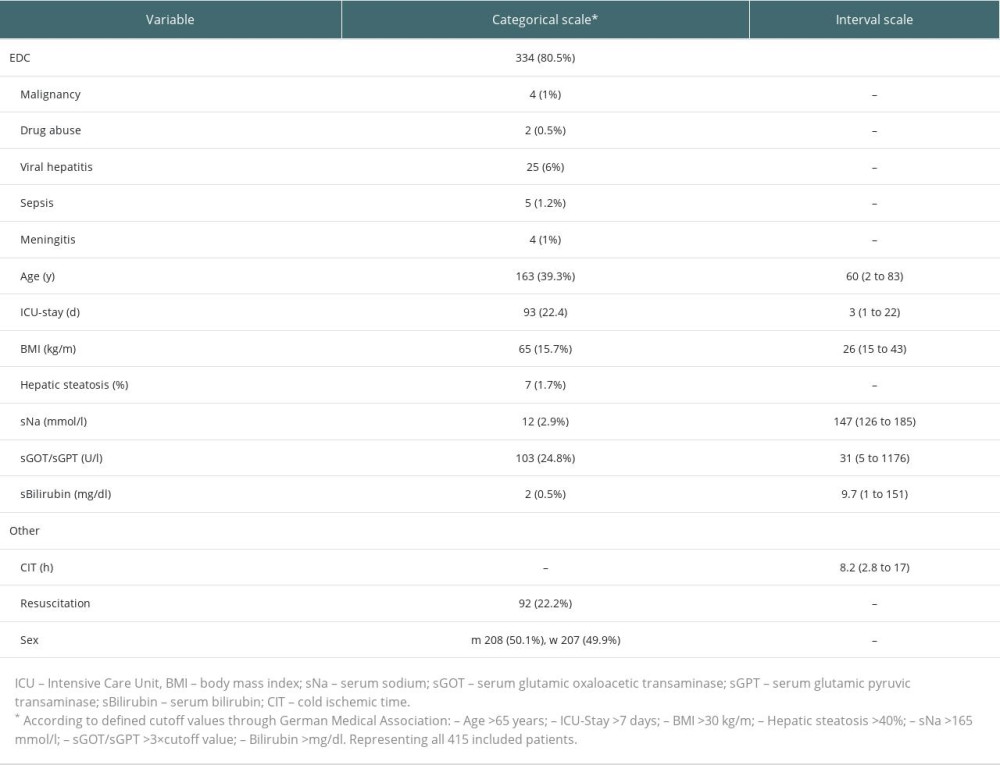 Table 2. Incidence of EDC and other related factors.
Table 2. Incidence of EDC and other related factors.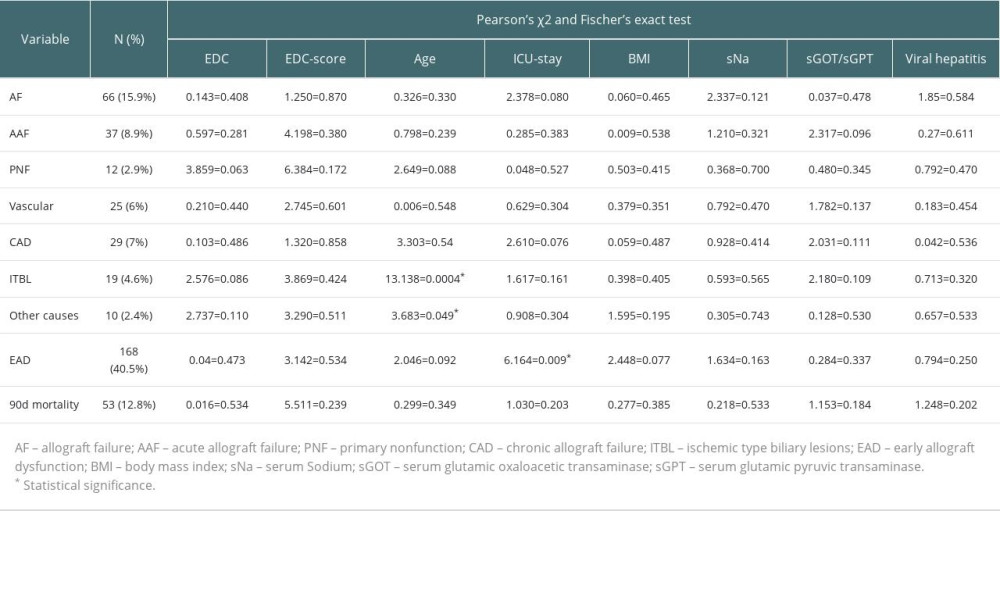 Table 3. Overview of incidence of study’s endpoints.
Table 3. Overview of incidence of study’s endpoints.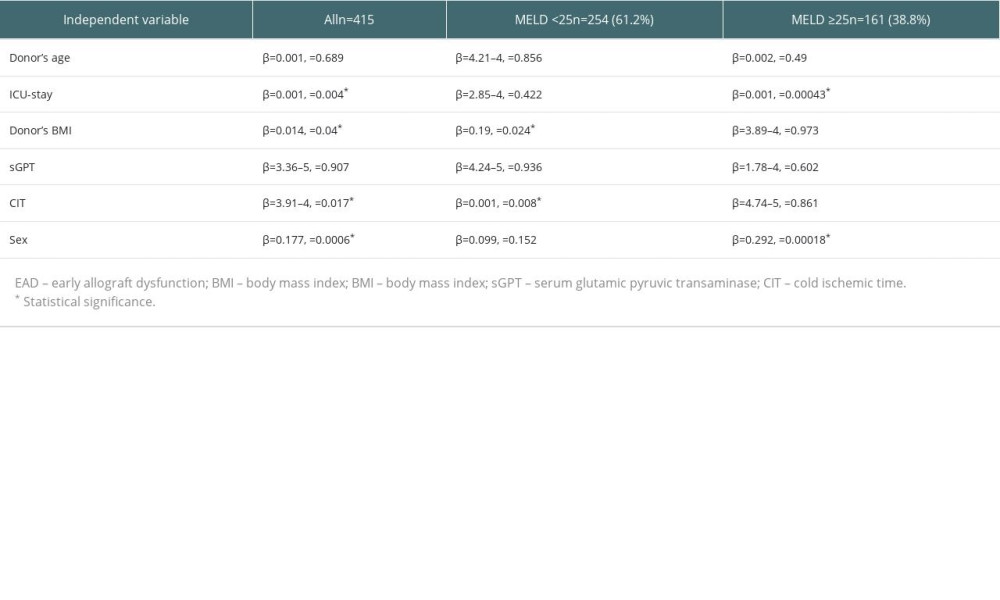 Table 4. Multiple regression; EAD as dependent variable.
Table 4. Multiple regression; EAD as dependent variable.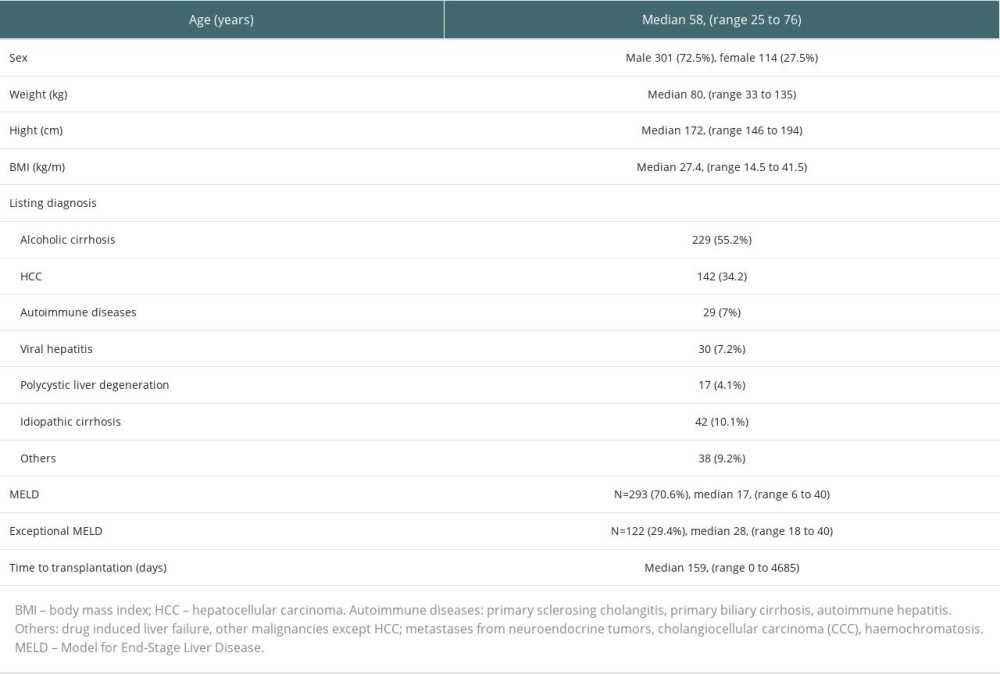 Table 1. Demographic results of all 415 included recipients.
Table 1. Demographic results of all 415 included recipients.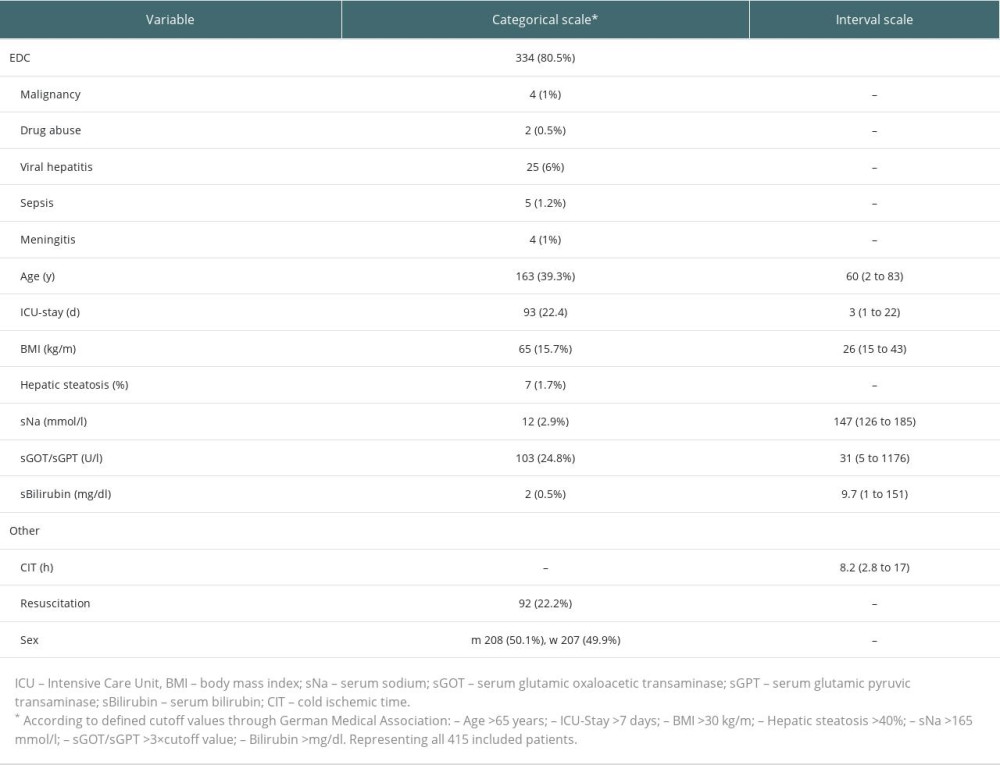 Table 2. Incidence of EDC and other related factors.
Table 2. Incidence of EDC and other related factors.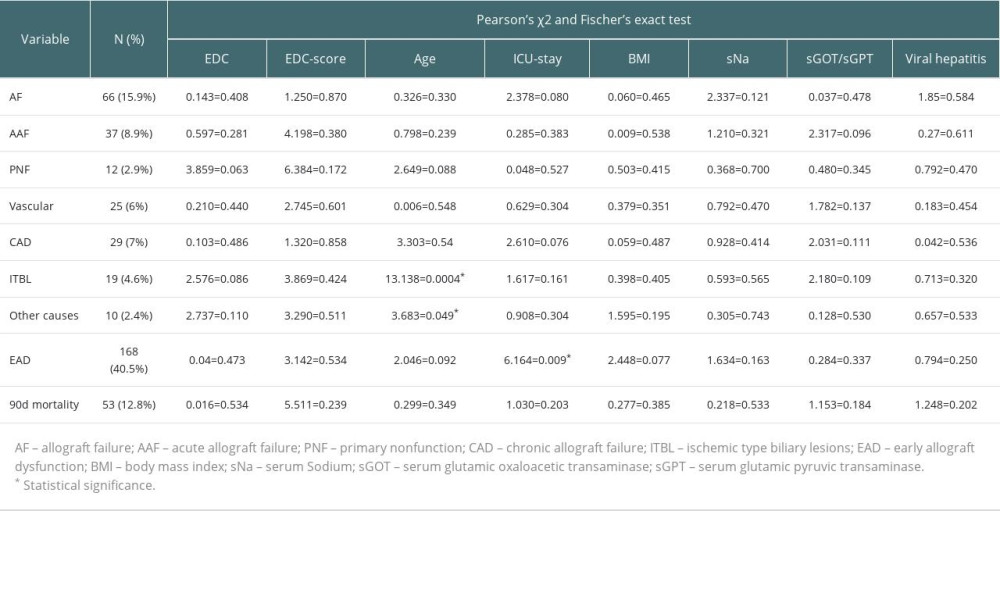 Table 3. Overview of incidence of study’s endpoints.
Table 3. Overview of incidence of study’s endpoints.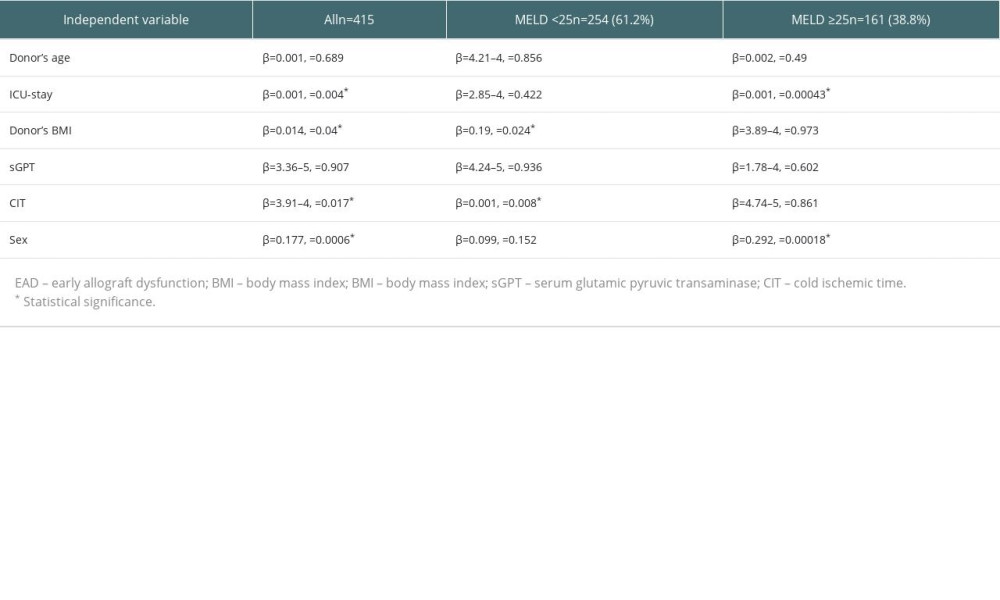 Table 4. Multiple regression; EAD as dependent variable.
Table 4. Multiple regression; EAD as dependent variable. In Press
15 Mar 2024 : Review article
Approaches and Challenges in the Current Management of Cytomegalovirus in Transplant Recipients: Highlighti...Ann Transplant In Press; DOI: 10.12659/AOT.941185
18 Mar 2024 : Original article
Does Antibiotic Use Increase the Risk of Post-Transplantation Diabetes Mellitus? A Retrospective Study of R...Ann Transplant In Press; DOI: 10.12659/AOT.943282
20 Mar 2024 : Original article
Transplant Nephrectomy: A Comparative Study of Timing and Techniques in a Single InstitutionAnn Transplant In Press; DOI: 10.12659/AOT.942252
28 Mar 2024 : Original article
Association Between FEV₁ Decline Rate and Mortality in Long-Term Follow-Up of a 21-Patient Pilot Clinical T...Ann Transplant In Press; DOI: 10.12659/AOT.942823
Most Viewed Current Articles
05 Apr 2022 : Original article
Impact of Statins on Hepatocellular Carcinoma Recurrence After Living-Donor Liver TransplantationDOI :10.12659/AOT.935604
Ann Transplant 2022; 27:e935604
12 Jan 2022 : Original article
Risk Factors for Developing BK Virus-Associated Nephropathy: A Single-Center Retrospective Cohort Study of ...DOI :10.12659/AOT.934738
Ann Transplant 2022; 27:e934738
22 Nov 2022 : Original article
Long-Term Effects of Everolimus-Facilitated Tacrolimus Reduction in Living-Donor Liver Transplant Recipient...DOI :10.12659/AOT.937988
Ann Transplant 2022; 27:e937988
15 Mar 2022 : Case report
Combined Liver, Pancreas-Duodenum, and Kidney Transplantation for Patients with Hepatitis B Cirrhosis, Urem...DOI :10.12659/AOT.935860
Ann Transplant 2022; 27:e935860








