17 March 2023: Original Paper
Critical Evaluation of Discarded Donor Livers in the Eurotransplant Region: Potential Implications for Machine Perfusion
Falk Rauchfuß1ABCDEF*, Hans-Michael TautenhahnDOI: 10.12659/AOT.938132
Ann Transplant 2023; 28:e938132
Abstract
BACKGROUND: There are still many offered donor livers that are declined during the allocation process. Machine perfusion offers the option to evaluate (especially marginal) donor organs and to better decide whether a graft has the potential of being transplanted or not. There is a lack of clear detailed data on why organs are declined and how many donor livers would have the potential of being evaluated in the machine.
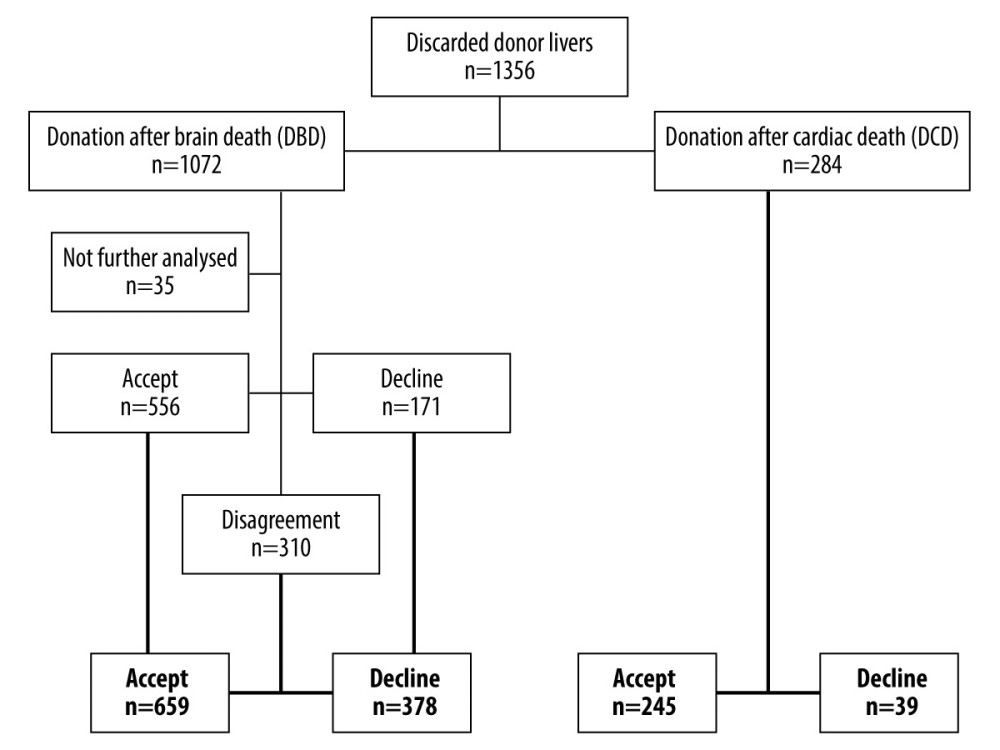
MATERIAL AND METHODS: We retrospectively reviewed 1356 donor livers between 2016 and 2018, which were offered by Eurotransplant and were declined during the allocation process; 284 grafts were from donor after cardiac death (DCD) and 1072 donations were from after brain death (DBD). The analysis was performed independently and blinded by senior transplant surgeons.
RESULTS: There were 904 (66.6%) donor livers with potential to be evaluated as suitable grafts in machine perfusion, whereas 417 (30.8%) organs were definitely not-transplantable, mainly due to liver cirrhosis, (untreated) donor malignancy, cardiac diseases of the donor leading to a hepatic congestion, and/or systemic infections in the donor. Donors in blood group “AB” were disproportionally often rejected. Due to missing data, 35 (2.6%) organs could not be sufficiently evaluated.
CONCLUSIONS: Our data suggest that many declined donor livers have potential of being evaluated by machine perfusion. Comprehensive use of machine perfusion is necessary and useful to improve the current organ shortage.
Keywords: Liver Transplantation, Tissue and Organ Procurement, Humans, Living Donors, Tissue Donors, Perfusion, Liver, Organ Preservation
Background
The potential value of machine perfusion, either hypothermic [1] or normothermic [2], has been shown recently. Beside logistical advantages, there were lower risks of non-anastomotic biliary strictures, especially in donation after cardiac death (DCD) donors [1], as well as a lower level of graft injury reflected by the liver enzymes [2]. Markmann et al showed a significant decrease of ischemic biliary complications applying a portable liver machine perfusion, especially in DCD donors [3].
However, machine perfusion becomes a more and more important technique in modern transplantation programs. One reason for being restrictive in establishing a machine perfusion program might be the immense cost per application, which are, depending on the cost coverage system of the individual countries, often not clarified and are a matter of debate. On the contrary, Raigani et al found that the costs for machine perfusion in an US cohort of extended-criteria and subsequently discarded livers were comparable to the monthly cost of care for waiting list patients with high MELD scores [4].
The organ demand in the Eurotransplant area is still high: in 2021, 2411 patients were registered on the waiting list vs 1514 performed liver transplantations from deceased donors (data provided in the Annual Report 2021 by Eurotransplant).
In recent years, the percentage of discarded livers within the Eurotransplant region varied from 18.4% to 26.7% (see Table 1, data from the “Annual reports” provided by Eurotransplant). However, it is unclear why a particular liver was discarded. The questions in this regard are what were the reasons for discarding the livers and do the discarded livers have a theoretical potential for evaluation in machine perfusion?
The aim of the study was to provide a practical evaluation of the discarded liver within the Eurotransplant region for absolute reasons for liver declining or for the eventual justification evaluating this liver during machine perfusion.
Material and Methods
DATA ANALYSIS:
The data were analyzed descriptively. A statistical analysis was not provided since the character of the data was unsuited to statistical comparison.
Results
Analysis of Donor Livers – Donation After Brain Death
ANALYSIS OF DONOR LIVERS – DONATION AFTER BRAIN DEATH:
From the 1072 DBD livers, we could not sufficiently judge 35 since there was a lot of missing information in the electronic database from donations outside the Eurotransplant area (n=34) and 1 potentially good donor liver could not be procured since the donor had massive intrabdominal adhesions due to previous operations. In the first analysis, 556 livers were assessed as suitable for machine perfusion, whereas 171 livers were declined. That resulted in 310 organs, but the initial investigators disagreed. After evaluation of the third investigator, 659 DBD livers were finally found to be suitable for machine perfusion and 378 were definitely declined.
REASONS FOR DECLINING ORGANS – DONATIONS AFTER BRAIN DEATH:
There were 378 donor livers not suitable for any liver transplantation. Reasons for declination were:
EVALUATION OF POTENTIALLY SUITABLE LIVERS – DONATIONS AFTER BRAIN DEATH:
From the donor organs that were assessed to be suitable for machine (n=659), there were 17 livers without any criteria for marginality. These grafts were considered adequate for transplantation according to our analysis but the reasons for denial could not be identified.
From the remaining donor organs, 139 had a severe steatosis or F2-fibrosis, 11 had an HCV-positive state with corresponding slight fibrosis, 13 were organs from donors with an age of “0” (donor weight between 2.6 and 6 kg) and the remaining 496 livers had a combination of increased age and/or long-lasting resuscitation episodes and/or significantly elevated liver enzymes and/or significantly increased sodium and/or steatosis in ultrasound and/or no available frozen section in time.
REASONS FOR DECLINING ORGANS – DONATIONS AFTER CARDIAC DEATH:
There were 39 donor livers not suitable for any liver transplantation. Reasons for declination were:
EVALUATION OF POTENTIALLY SUITABLE LIVERS – DONATIONS AFTER CARDIAC DEATH:
From the potential donor organs after cardiac death, 245 livers could have been transplanted on the basis of the available data but the reasons for declining the organs were not available for this study. Furthermore, 67 donor livers would have had the potential for an evaluation in the machine. Reasons for this were:
Steatosis ± elevated transaminases (n=18); highly elevated transaminases after resuscitation (n=17); alcohol abuse and steatosis ± resuscitation (n=4); high BMI and elevated transaminases ± resuscitation (n=3); alcohol abuse and hepatitis B or C (n=3); highly elevated transaminases (n=2); unclear histology of suspected malignancy (n=2); prolonged resuscitation (n=2); child <5 kg (n=1); high BMI and older donor (n=1); normal liver enzymes but ischemic cardiomyopathy (n=1); COPD and cardiac revascularization (n=1); other reasons (n=12).
Discussion
STEATOSIS:
The demographic development and the increasing proportion of obese people lead naturally to more steatotic donor livers, which have to be assessed for their suitability for liver transplantation. In general, microsteatosis is mostly seen as uncritical and potentially reversible, whereby severe macrosteatosis is considered to be a risk factor for graft dysfunction up to life-threatening graft failure.
A recently published review by Lai et al showed that machine perfusion might attenuate the graft damage from macrosteatotic livers measured by the peak of transaminases. “Hard” outcome parameters like recipient’s death or need for retransplantation were rare events and therefore not sufficiently ratable in this study due to the relatively small number of included patients [8].
The future in this context will be a pharmacological modulation of the livers, as shown by Raigani et al in an animal model. They showed a better graft function after defatting initially steatotic livers [9]. As shown by the same group, metabolic and lipidomic profiling during normothermic machine perfusion might have the potential to guide the resuscitation and rehabilitation of steatotic donor livers [10]. Boteon et al manipulated the lipid metabolism of human livers and decreased the lipid content of the potential graft [11].
In our analysis, graft steatosis was obviously a major concern, which subsequently led to organ rejection. In our opinion, severe (macro-)steatosis is indeed a major reason for declining a donor organ. Therefore, we see a main application for the usage of machine perfusion in steatotic organs which are otherwise not transplanted with a clear conscience. Machine perfusion makes it on the one hand possible to assess the organ even if a severe steatosis was diagnosed and, on the other hand, will give the centers the opportunity to affect the steatosis in terms of a “defatting procedure”.
UNCLEAR FINDINGS IN FROZEN SECTIONS:
In some donors, there are unclear findings during organ procurement, in worst case suspicious for a malignant disease. In an Italian analysis of 11 271 organ donors, in 595 of these a malignant disease was already treated in the history or actually [12]. In an autopsy study, unsuspected neoplasia rate was 7% [13]. Organs with an unclear finding during an organ procurement are usually rejected if the histologic analysis does not come to an unambiguous benign result. In some cases, time-consuming histologic analysis is necessary. This time is, considering the cold ischemia time, often unavailable and could be bridged using machine perfusion.
ELEVATED LIVER ENZYMES/STATE AFTER PROLONGED RESUSCITATION:
A prolonged resuscitation associated with elevated liver enzymes are suspect for a significant hepatocellular damage due to the period of warm ischemia time, which often leads to rejection of the potential donor organ since the risk for primary non-function or ischemic cholangiopathy is considered to be too high. This is not only the case in DCD (see below) but also in DBD (with hypoxic brain damage as cause of death leading to organ donation). In these cases, machine perfusion can also be an option to assess the near-term graft function and therefore minimizing the risk of a fatal graft failure. Furthermore, the risk of non-anastomotic biliary strictures is minimized when machine perfusion is applied [1].
DONATION AFTER CARDIAC DEATH:
This is predominantly a domain for machine perfusion. However, the different allocation rules in Eurotransplant countries allowing or prohibiting DCD can make the allocation difficult. Furthermore, logistical reasons are easily conceivable in this particular mode of organ donation. Croome et al reported that ischemic cholangiopathy after non-heart beating donation as problematic, suggesting machine perfusion as a suitable tool for reduction of complications and improving prediction of risk after non-heart beating donation [14]. This is not only the case for donor livers after non-heart beating donation, but also for kidneys [15].
BLOOD GROUPS:
We found in our analysis a remarkable distribution of blood groups showing a higher proportion of discarded organs in blood group “AB” (9.5% of all discarded donor livers). Usually, blood group “AB” is found in around 5% of the Mid-European population [16]. Most centers are restrictive when accepting organs for “AB” recipients since the waiting list dynamic shows that the small number of AB recipients goes along with the highest probability getting transplanted in a MELD-based allocation system when having blood group “AB” [17]. Therefore, marginal organs for “AB” recipients are discarded more often as the centers take the chance of picking a better organ for a particular “AB” patient.
Machine perfusion can offer the following opportunities for “AB” donor livers:
LIMITATIONS:
Of course, a retrospective study designs always has limitations. In this particular study, we were faced with the following problems:
Conclusions
In summary, we showed that 904 declined donor livers would have had the potential to be evaluated with machine perfusion (donation after brain death: 659; non-heart beating donation: 245). Our data suggest that comprehensive use of machine perfusion is necessary and useful to improve the current organ shortage.
References
1. van Rijn R, Schurink IJ, de Vries Y, Hypothermic machine perfusion in liver transplantation – a randomized trial: N Engl J Med, 2021; 384(15); 1391-401
2. Nasralla D, Coussios CC, Mergental H, A randomized trial of normothermic preservation in liver transplantation: Nature, 2018; 557(7703); 50-56
3. Markmann JF, Abouljoud MS, Ghobrial RM, Impact of portable normothermic blood-based machine perfusion on outcomes of liver transplant: The OCS Liver PROTECT Randomized Clinical Trial: JAMA Surg, 2022; 157(3); 189-98
4. Raigani S, De Vries RJ, Carroll C, Viability testing of discarded livers with normothermic machine perfusion: Alleviating the organ shortage outweighs the cost: Clin Transplant, 2020; 34(11); e14069
5. European Directorate for the Quality of Medicines & HealthCare: Guide to the quality and safety of organs for transplantation, 2022
6. Mergental H, Perera MT, Laing RW, Transplantation of declined liver allografts following normothermic ex-situ evaluation: Am J Transplant, 2016; 16(11); 3235-45
7. Clavien PA, Dutkowski P, Mueller M, Transplantation of a human liver following 3 days of ex situ normothermic preservation: Nat Biotechnol, 2022; 40(11); 1610-16
8. Lai Q, Ruberto F, Pawlik TM, Use of machine perfusion in livers showing steatosis prior to transplantation: A systematic review: Updates Surg, 2020; 72(3); 595-604
9. Raigani S, Carroll C, Griffith S, Improvement of steatotic rat liver function with a defatting cocktail during ex situ normothermic machine perfusion is not directly related to liver fat content: PLoS One, 2020; 15(5); e0232886
10. Raigani S, Karimian N, Huang V, Metabolic and lipidomic profiling of steatotic human livers during ex situ normothermic machine perfusion guides resuscitation strategies: PLoS One, 2020; 15(1); e0228011
11. Boteon YL, Attard J, Boteon A, Manipulation of lipid metabolism during normothermic machine perfusion: Effect of defatting therapies on donor liver functional recovery: Liver Transpl, 2019; 25(7); 1007-22
12. Eccher A, Lombardini L, Girolami I, How safe are organs from deceased donors with neoplasia? The results of the Italian Transplantation Network: J Nephrol, 2019; 32(2); 323-30
13. Sens MA, Zhou X, Weiland T, Cooley AM, Unexpected neoplasia in autopsies: Potential implications for tissue and organ safety: Arch Pathol Lab Med, 2009; 133(12); 1923-31
14. Croome KP, Taner CB, The changing landscapes in DCD liver transplantation: Curr Transplant Rep, 2020; 7(3); 194-204
15. Jochmans I, Brat A, Davies L, Oxygenated versus standard cold perfusion preservation in kidney transplantation (COMPARE): A randomised, double-blind, paired, phase 3 trial: Lancet, 2020; 396(10263); 1653-62
16. Chandler T, Hiller J, Peine S, Stargardt T, Blood donation and donors: Insights from a large German teaching hospital (2008–2017): Vox Sang, 2020; 115(1); 27-35
17. Barone M, Avolio AW, Di Leo A, ABO blood group-related waiting list disparities in liver transplant candidates: Effect of the MELD adoption: Transplantation, 2008; 85(6); 844-49
Tables
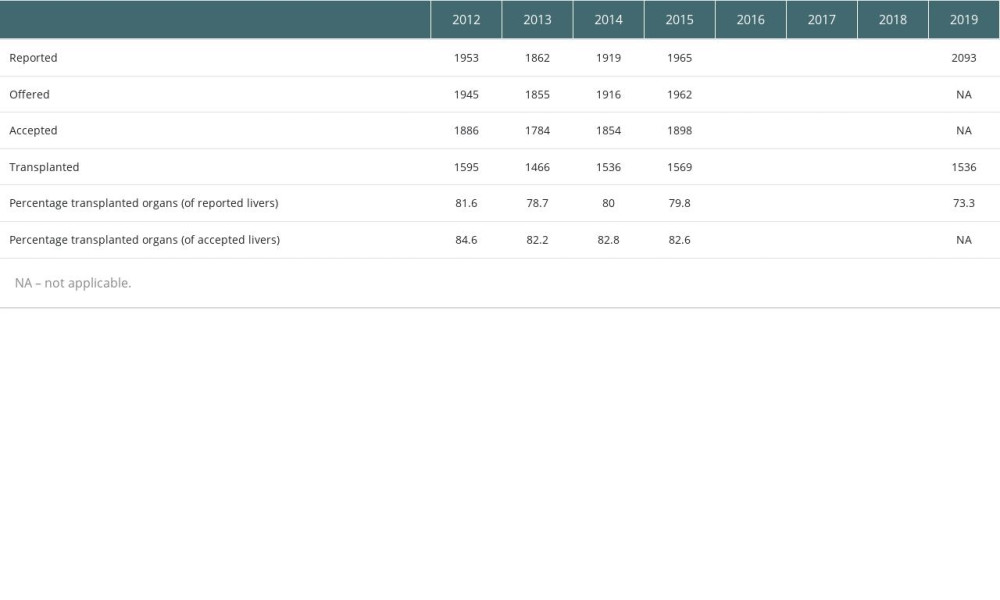 Table 1. Numbers and percentage of reported, offered, accepted and transplanted donor livers per year between 2012 and 2019 within the Eurotransplant region (study period in bold letters).
Table 1. Numbers and percentage of reported, offered, accepted and transplanted donor livers per year between 2012 and 2019 within the Eurotransplant region (study period in bold letters).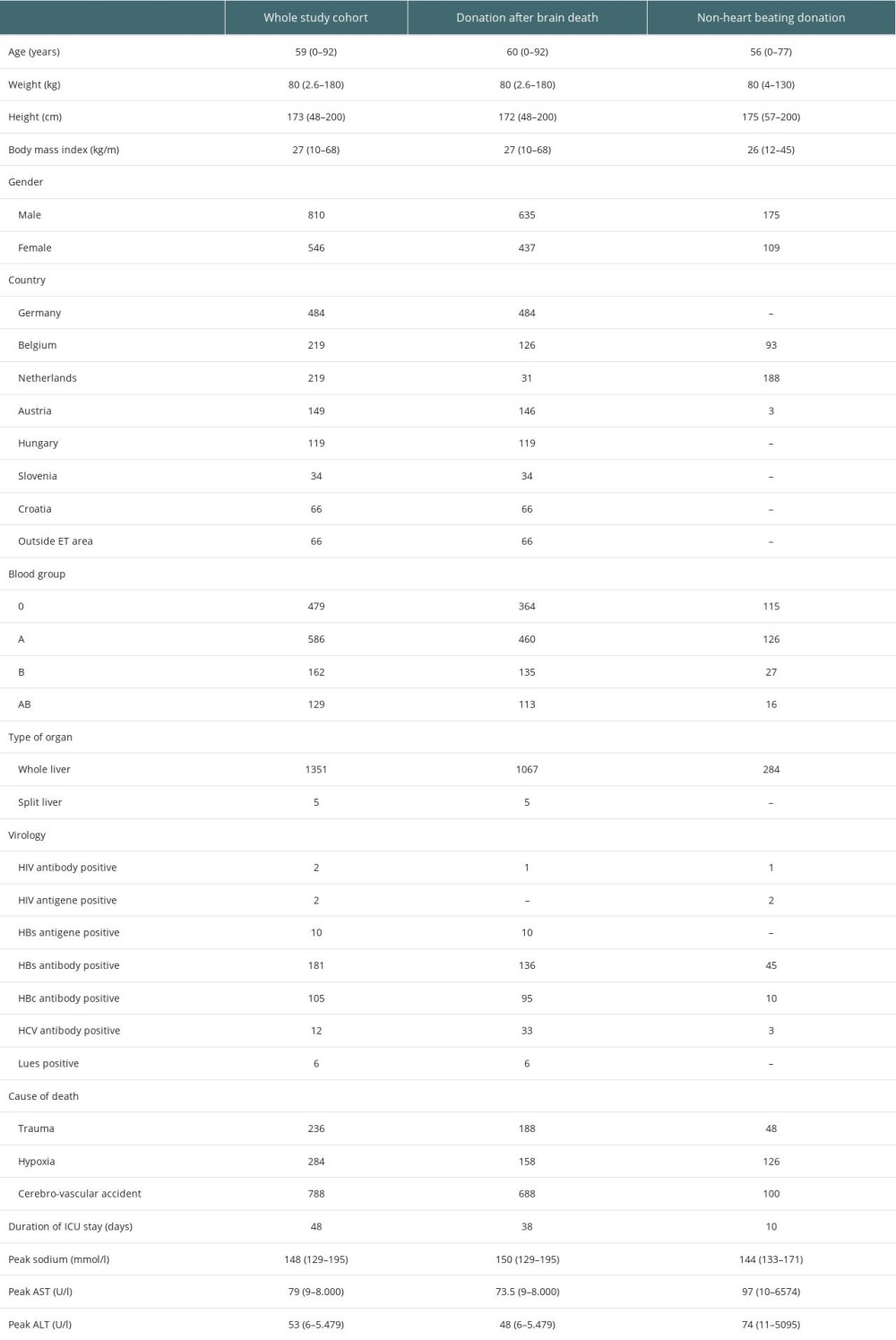 Table 2. Data of the whole study cohort.
Table 2. Data of the whole study cohort.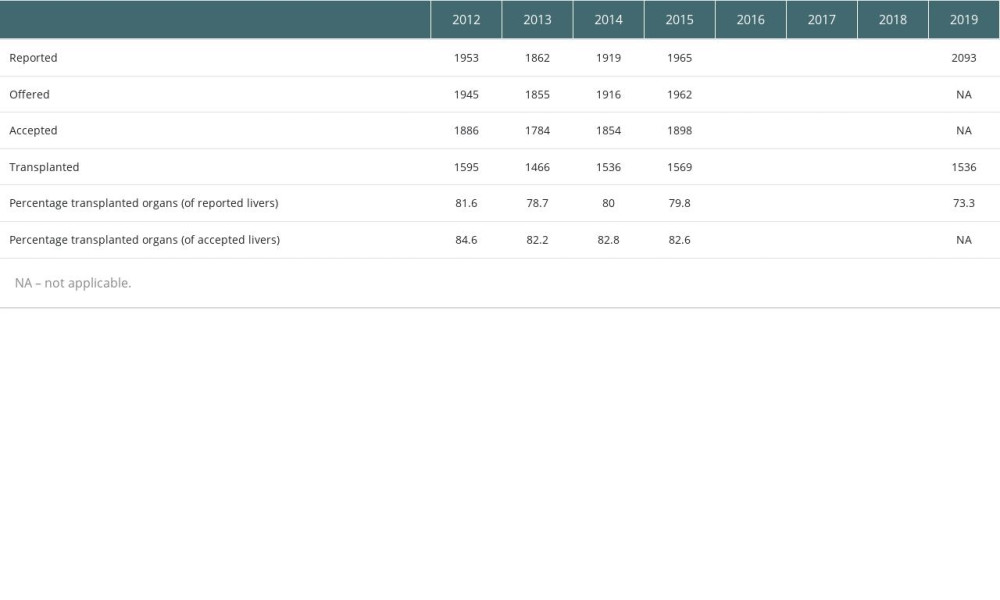 Table 1. Numbers and percentage of reported, offered, accepted and transplanted donor livers per year between 2012 and 2019 within the Eurotransplant region (study period in bold letters).
Table 1. Numbers and percentage of reported, offered, accepted and transplanted donor livers per year between 2012 and 2019 within the Eurotransplant region (study period in bold letters).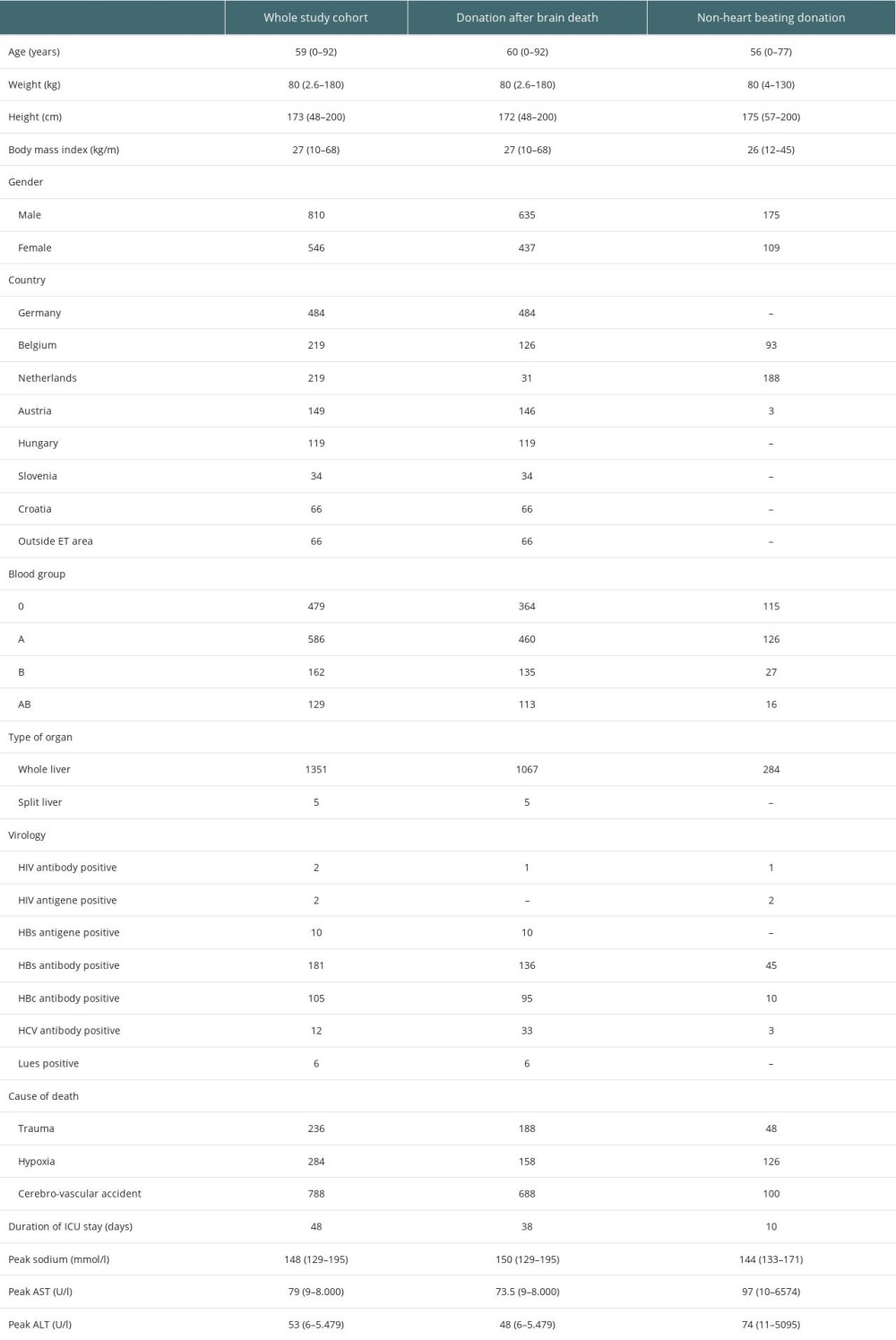 Table 2. Data of the whole study cohort.
Table 2. Data of the whole study cohort. In Press
15 Mar 2024 : Review article
Approaches and Challenges in the Current Management of Cytomegalovirus in Transplant Recipients: Highlighti...Ann Transplant In Press; DOI: 10.12659/AOT.941185
18 Mar 2024 : Original article
Does Antibiotic Use Increase the Risk of Post-Transplantation Diabetes Mellitus? A Retrospective Study of R...Ann Transplant In Press; DOI: 10.12659/AOT.943282
20 Mar 2024 : Original article
Transplant Nephrectomy: A Comparative Study of Timing and Techniques in a Single InstitutionAnn Transplant In Press; DOI: 10.12659/AOT.942252
28 Mar 2024 : Original article
Association Between FEV₁ Decline Rate and Mortality in Long-Term Follow-Up of a 21-Patient Pilot Clinical T...Ann Transplant In Press; DOI: 10.12659/AOT.942823
Most Viewed Current Articles
05 Apr 2022 : Original article
Impact of Statins on Hepatocellular Carcinoma Recurrence After Living-Donor Liver TransplantationDOI :10.12659/AOT.935604
Ann Transplant 2022; 27:e935604
12 Jan 2022 : Original article
Risk Factors for Developing BK Virus-Associated Nephropathy: A Single-Center Retrospective Cohort Study of ...DOI :10.12659/AOT.934738
Ann Transplant 2022; 27:e934738
22 Nov 2022 : Original article
Long-Term Effects of Everolimus-Facilitated Tacrolimus Reduction in Living-Donor Liver Transplant Recipient...DOI :10.12659/AOT.937988
Ann Transplant 2022; 27:e937988
15 Mar 2022 : Case report
Combined Liver, Pancreas-Duodenum, and Kidney Transplantation for Patients with Hepatitis B Cirrhosis, Urem...DOI :10.12659/AOT.935860
Ann Transplant 2022; 27:e935860