09 April 2024: Original Paper
Impact of Blood Products Transfusion on Patients in the Immediate Post-Lung Transplant Period: A Cohort Study
Atif S. Siddiqui12ABCDEF*, Jawairia ShakilDOI: 10.12659/AOT.943652
Ann Transplant 2024; 29:e943652
Abstract
BACKGROUND: Anemia is common in post-transplant patients. Blood product transfusion is associated with mortality and rejection in solid organ transplants. In lung transplant recipients, transfusion predisposes to primary graft dysfunction (PGD). The adverse effects and associated mortality of perioperative transfusions in lung transplant recipients have not been evaluated. This study examined the effects of perioperative blood transfusions in lung transplant recipients.
MATERIAL AND METHODS: We conducted a retrospective study of the effects of blood product transfusions in patients who received single- or double-lung transplantation at Houston Methodist Hospital between August 2017 and September 2019. Univariable and multiple logistic regression modeling were used to determine the characteristics associated with single events as well as a composite outcome within 30 days (including mortality, acute myocardial infarction, acute stroke, lower respiratory tract infection, urinary tract infection, surgical site infections, or PGD).
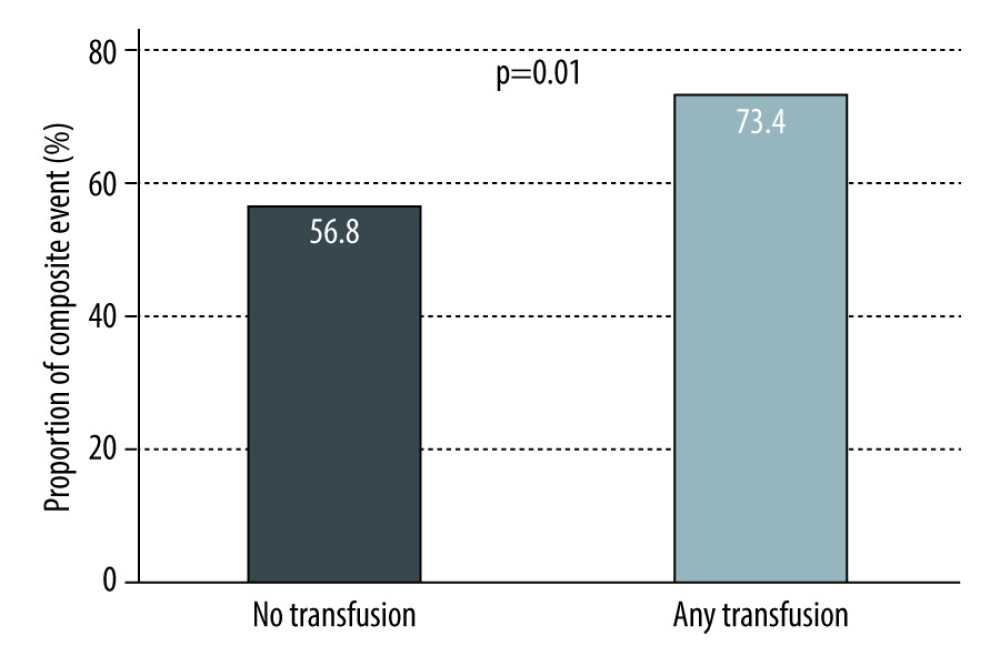
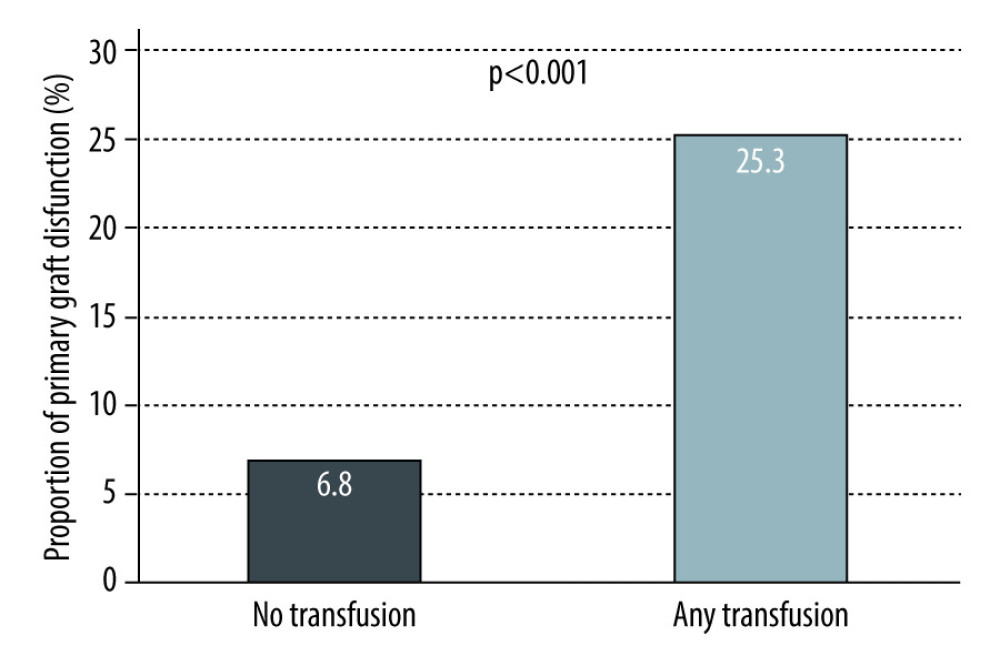
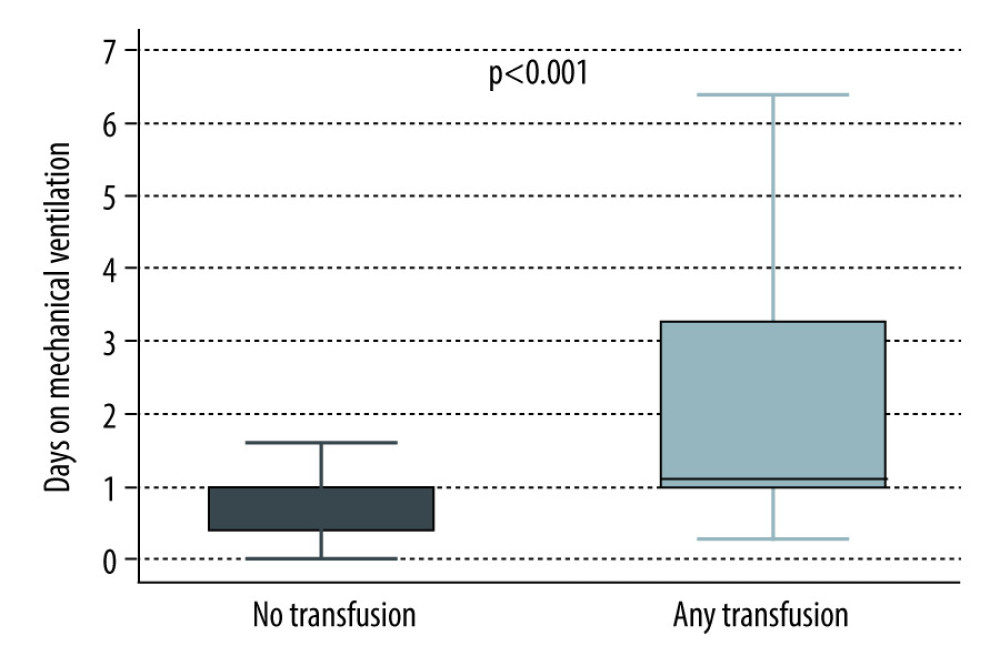
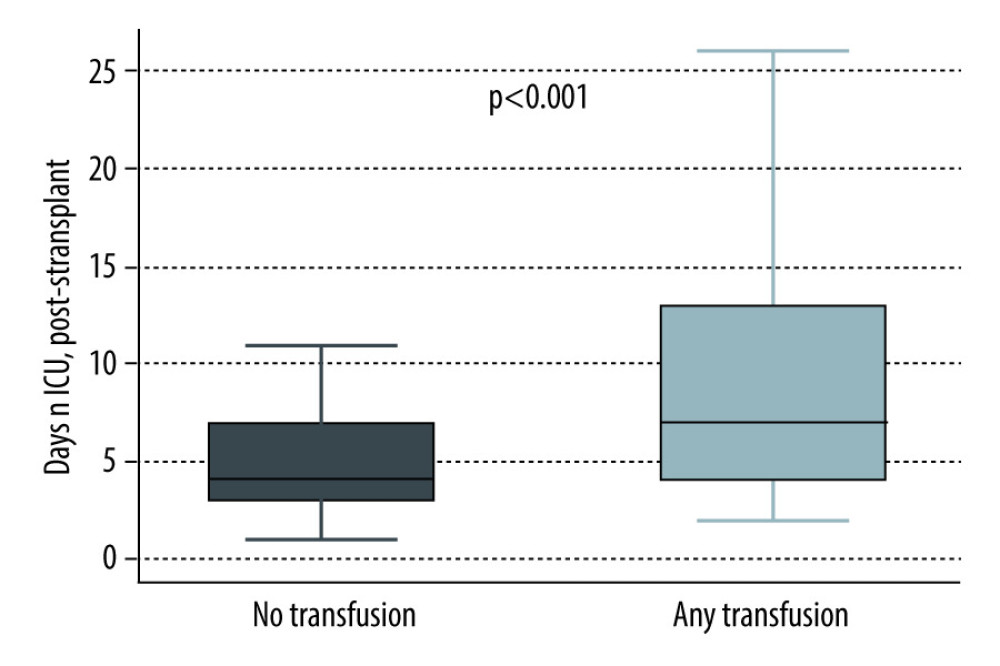
RESULTS: A total of 232 patients received lung transplants between December 2015 and September 2019 at our center. Univariable analysis revealed an increased risk of PGD (P<0.001), more mechanical ventilation days (P<0.001), more ICU days post-transplant (P<0.001), and greater need for ECMO support (P=0.001) in patients who received blood product transfusions. In univariate analysis, the composite outcome was also more common (P=0.01) in patients who received any transfusion perioperatively. A total of 7 patients died within 30 days from transplant, and they were all in the transfused group.
CONCLUSIONS: Among lung transplant recipients, PGD, ICU days, need for mechanical ventilation and ECMO support, and total composite events were significantly greater in patients who received blood transfusion perioperatively.
Keywords: Blood Transfusion, Lung Transplantation, Primary Graft Dysfunction
Introduction
More than 15 million units of red blood cells are transfused annually in the United States [1]. Blood transfusion is associated with many established risks, including transfusion-related acute lung injury, transfusion-associated circulatory overload, infections, increased occurrence of renal failure, neurologic complications, and prolonged intensive care unit stay [2–5].
The Transfusion Requirement in Critical Care (TRICC) trial compared a liberal (target hemoglobin 10–12 gram per deciliter [g/dL]) with a restrictive (target hemoglobin 7–9 g/dL) strategy of transfusion in critically ill patients [6], showing that the 30-day all-cause mortality rate was not significantly different between the restrictive strategy and the liberal strategy. Liberal transfusion was not associated with shorter ICU or hospital stay or less organ failure. Furthermore, longer mechanical ventilation duration and cardiac events were more frequent in the liberal strategy group [6].
A randomized clinical trial investigating septic shock demonstrated that hemoglobin thresholds of 7 g/dL and 9 g/dL had similar rates of 90-day mortality, use of life support, ischemic events, and severe adverse reactions to blood transfusion [7].
Blood transfusions are frequently administered to surgical patients [8]. Perioperative anemia is common after cardiac surgery and is associated with significant increases in morbidity and mortality [9–11]. A randomized, controlled clinical trial in cardiac surgery patients compared transfusion thresholds of hematocrit less than 30% with hematocrit less than 24% from the start of surgery through the ICU stay [12], finding no difference in the composite outcome of 30-day all-cause mortality and severe morbidity between the liberal and restrictive strategies, and fewer blood products were administered in the restrictive group. The liberal transfusion threshold for hemoglobin 9 g/dL after cardiac surgery was not superior to the restrictive transfusion threshold for postoperative hemoglobin level of less than 7.5 g/dL with respect to postoperative morbidity or total costs [13]. Comparable results were also described in hip surgery patients. Crason and colleagues showed that a liberal transfusion strategy, as compared with a restrictive strategy, did not reduce rates of death or inability to walk independently at 60-day follow-up or reduce in-hospital morbidity in elderly patients at high cardiovascular risk [14].
Anemia is a common finding in post-lung transplant patients. Mechanisms include blood loss, immune-mediated hemolysis, drug-induced hemolysis and bone marrow suppression (particularly related to immunosuppressive medications), and non-immune-mediated hemolysis [15–24]. Blood transfusion has been associated with increased mortality in other solid organ transplant recipients, including liver and kidney [25].
Blood transfusion has also been proposed as a possible lung transplant recipient-related risk factor for primary graft dysfunction (PGD) [24]. The impact of intraoperative transfusion on postoperative mortality in lung transplant recipients is still unclear. Ong et al demonstrated that blood transfusion had no effect on all-cause mortality, but greater administration of platelets was associated with higher adjusted 1-year mortality [26]. We therefore sought to examine whether blood product transfusions in the perioperative period are associated with adverse outcomes in lung transplant recipients. We hypothesized that a restrictive strategy of blood transfusion with lower hemoglobin transfusion threshold of less than 8 g/dL is associated with improved short-term survival and decreased postoperative complications in patients who underwent lung transplant as compared to a liberal strategy of blood transfusion with higher hemoglobin transfusion threshold of less than 10 g/dL.
Material and Methods
STUDY DESIGN:
We conducted a single-center, retrospective, observational cohort study of adult patients who underwent lung transplant at Houston Methodist Hospital J.C. Walter JR Transplant Center from December 2015 to September 2019. We included patients aged 18 years and older who received single- or double-lung transplants and had a postoperative nadir hemoglobin level below 10.0 g/dL. We excluded patients who were pregnant, received heart-lung or lung-liver transplants, were prevented from having blood and blood products according to a belief system (eg Jehovah’s Witnesses), and patients with congenital or acquired platelet, red cell, or clotting disorders. Eligible patients were followed for 30 days after transplant. Primary disease groups were categorized into idiopathic pulmonary fibrosis, chronic obstructive pulmonary disease, cystic fibrosis, and pulmonary arterial hypertension. Other disease processes were placed in a miscellaneous category. Lowest hemoglobin level, lowest platelet count, and highest international normalized ratios (INR) were recorded during intraoperative and postoperative periods until day 7 postoperatively. The number of units of each blood product transfused (pack red blood cells, platelets, cryoprecipitate, and fresh frozen plasma) was recorded until postoperative day 6 of lung transplant. The study was conducted with approval of the institutional review board. De-identified information was maintained in the secure database on protected servers at Houston Methodist Hospital.
ENDPOINTS:
Our primary endpoint was 30-day mortality after lung transplantation. The pre-determined secondary outcome within 30 days was a composite of either mortality, acute myocardial infarction, acute stroke, lower respiratory tract infection, urinary tract infection, surgical site infections, or primary graft dysfunction.
STATISTICAL ANALYSIS:
Descriptive data are reported as median (interquartile range, IQR) for continuous variables, and as frequencies and proportions for categorical variables. Differences between groups (having no transfusion versus having any transfusion) were compared using the Kruskal-Wallis test for continuous variables and the chi-square or Fisher’s exact tests for categorical variables, as appropriate. Bar charts and box plots were used to present the outcomes of interest. Multivariable logistic regression modeling was used to determine the characteristics associated with the composite outcome within 30 days (of either mortality, acute myocardial infarction, acute stroke, lower respiratory tract infection, urinary tract infection, surgical site infections, or primary graft dysfunction). Variables for the multivariable models were selected based on the clinical importance and by the Stata’s LASSO technique with the cross-validation (CV) selection option. The performance of the models was determined by the area under the receiver operating characteristic curve (AUC). All analyses were performed on Stata version 16.1 (StataCorp LLC, College Station, TX, USA). A
Results
CLINICAL CHARACTERISTICS:
A total of 232 adult patients were included in this study. A total of 158 patients (68%) received any blood product transfusion in the 7 perioperative days. The median age was 62 years, and 54.7% of patients were men. Single lung transplant was performed in 26.3% of the patients, and 73.7% received a double-lung transplant. Baseline hemoglobin was significantly different, in that the no-transfusion group had a higher baseline (13.0 vs 11.4; P<0.001). However, the baseline platelets and INR were similar in both groups. There were more smokers and patients with previous malignancies in the no-transfusion group, whereas the other comorbidities, including diabetes and chronic kidney disease, were present in similar proportions in both groups. Of note, in the no-transfusion cohort, there were no patients on mechanical ventilation or ECMO support prior to the transplant, whereas in the transfusion cohort, there were 9 (5.7%) on mechanical ventilation and 7 (4.4%) on ECMO. Additionally, the median ischemic time was higher (4.3 vs 3.8 h; P=0.01) in the transfusion group. Every patient was followed up for 30 days to assess the pre-defined endpoints. The baseline characteristics of patients are detailed in Table 1. All patients were included in the analysis.
END POINTS:
Overall, there was a trend towards worse outcomes in patients who received transfusions (Table 2). A total of 7 patients died within 30 days from transplant and these were all in the transfused group. There was a statistically significant increase in the composite outcome (73.4% vs 56.8%; P=0.01), PGD (25.3% vs 6.8%; P<0.001), days on mechanical ventilation (1.1 [1.0, 3.3] vs 1.0 (0.4, 1.0); P<0.001), ICU days after transplant (7.0 [4.0, 13.0] vs 4.0 [3.0, 7.0]; P<0.001) (Figures 1–4), and need for ECMO support (11.4% vs 0; P=0.001) in transfused patients. There was a higher incidence of acute myocardial infarction (7.6% vs 2.7%; P=0.24), acute stroke (4.4% vs 0%; P=0.1), lower respiratory tract infections (56.3% vs 51.4%; P=0.48), and acute kidney injury (42% vs 35.6%; P=0.35) in patients who received transfusions, but the differences were not statistically significant. Univariable logistic regression analysis showed that having any transfusion was significantly associated with the composite outcome (OR 2.1 [1.18–3.76]; P=0.01) (Table 3).
Discussion
CLINICAL IMPLICATIONS:
From the data analyzed, we provide further evidence to support a conservative transfusion approach in the perioperative period of lung transplantation to decrease the risk of PGD, minimizing the time on mechanical ventilatory support and overall duration of hospital stay. There is a general trend to more adverse outcomes in patients with more liberal transfusion strategies, which may become statistically significant given a larger sample size.
STUDY STRENGTHS AND LIMITATIONS:
Although this was a single-center retrospective cohort study, our study population represents the general population of patients who undergo lung transplantation. The study included patients who received lung transplants for all major primary disease groups and had various comorbidities. The results of our study are generalizable to patients undergoing lung transplantation at a large transplant center with extensive experience. Future studies are needed to identify further modifiable factors that are associated with poor outcomes in this population and to assess interventions targeting those variables.
Conclusions
Blood transfusions are common in all aspects of medicine, especially in surgeries and transplants. The present study shows that a more restrictive transfusion strategy is associated with improved patient outcomes. Further prospective studies can aid in providing causal evidence in this matter, as well as to provide transfusion targets in this population of patients.
References
1. Report of the Department of Health and Human Services: The 2009 national blood collection and utilization survey report, 2011, Washington, DC, Department of Health and Human Services, Office of the Assistant Secretary for Health
2. Gajic O, Gropper MA, Hubmayr RD, Pulmonary edema after transfusion: How to differentiate transfusion-associated circulatory overload from transfusion-related acute lung injury: Crit Care Med, 2006; 34; 109-13
3. Koch C, Li L, Figueroa P, Transfusion and pulmonary morbidity after cardiac surgery: Ann Thorac Surg, 2009; 88; 1410-18
4. Leal-Noval SR, Rincón-Ferrari MD, García-Curiel A, Transfusion of blood components and postoperative infection in patients undergoing cardiac surgery: Chest, 2001; 119(5); 1461-68
5. Engoren MC, Habib RH, Zacharias A, Effect of blood transfusion on long-term survival after cardiac operation: Ann Thorac Surg, 2002; 74(4); 1180-86
6. Hébert PC, Wells G, Blajchman MA, A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care: N Engl J Med, 1999; 340; 409-17
7. Holst LB, Haase N, Wetterslev J, Wernerman J, Lower versus higher hemoglobin threshold for transfusion in septic shock: N Engl J Med, 2014; 371(15); 1381-91
8. Cobain TJ, Vamvakas EC, Wells A, Titlestad K, A survey of the demographics of blood use: Transfus Med, 2007; 17; 1-15
9. Stover EP, Siegel LC, Parks RInstitutions of the Multicenter Study of Perioperative Ischemia Research Group, Variability in transfusion practice for coronary artery bypass surgery persists despite national consensus guidelines: A 24-institution study: Anesthesiology, 1998; 88(2); 327-33
10. Rogers MA, Blumberg N, Saint S, Hospital variation in transfusion and infection after cardiac surgery: BMC Med, 2009; 7; 37
11. Snyder-Ramos SA, Möhnle P, Weng YSInvestigators of the Multicenter Study of Perioperative Ischemia; MCSPI Research Group, The ongoing variability in blood transfusion practices in cardiac surgery: Transfusion, 2008; 48(7); 1284-99
12. Hajjar LA, Vincent JL, Galas FR, Transfusion requirements after cardiac surgery: JAMA, 2010; 304(14); 1559-67
13. Murphy GJ, Pike K, Rogers CA, Liberal or restrictive transfusion after cardiac surgery: N Engl J Med, 2015; 372; 997-1008
14. Carson JL, Terrin ML, Noveck H, Liberal or restrictive transfusion in high-risk patients after hip surgery: N Engl J Med, 2011; 365; 2453-62
15. Tager AM, Ginns LC, Complications of lung transplantation: Crit Care Nurs Clin North Am, 1996; 8; 273-92
16. Bapat AR, Schuster SJ, Dahlke M, Ballas SK, Thrombocytopenia and autoimmune hemolytic anemia following renal transplantation: Transplantation, 1987; 44; 157-59
17. Salerno CT, Burdine J, Perry EH, Donor-derived antibodies and hemolysis after ABO-compatible but nonidentical heart-lung and lung transplantation: Transplantation, 1998; 65; 261-64
18. Panaro F, DeChristopher PJ, Rondelli D, Severe hemolytic anemia due to passenger lymphocytes after living-related bowel transplant: Clin Transplant, 2004; 18; 332-35
19. Sokol RJ, Stamps R, Booker DJ, Posttransplant immune-mediated hemolysis: Transfusion, 2002; 42; 198-204
20. Balfour HH, Antiviral drugs: N Engl J Med, 1999; 340; 1255-68
21. The U. S. Multicenter FK506 Liver Study Group, A comparison of tacrolimus (FK 506) and cyclosporine for immunosuppression in liver transplantation: N Engl J Med, 1994; 331; 1110-15
22. Apperley JF, Dowding C, Hibbin J, The effect of cytomegalovirus on hemopoiesis: In vitro evidence for selective infection of marrow stromal cells: Exp Hematol, 1989; 17; 38-45
23. Eid AJ, Brown RA, Patel R, Razonable RR, Parvovirus B19 infection after transplantation: A review of 98 cases: Clin Infect Dis, 2006; 43; 40-48
24. Oberkofler CE, Dutkowski P, Stocker R, Model of end stage liver disease (MELD) score greater than 23 predicts length of stay in the ICU but not mortality in liver transplant recipients: Crit Care, 2010; 14(3); R117
25. Barr ML, Kawut SM, Whelan TPISHLT Working Group on Primary Lung Graft Dysfunction, Report of the ISHLT. Working Group on primary lung graft dysfunction part IV: Recipient related risk factors and markers: J Heart Lung Transplant, 2005; 24; 1468-82
26. Ong LP, Thompson E, Sachdeva A, Allogeneic blood transfusion in bilateral lung transplantation: impact on early function and mortality: Eur J Cardiothorac Surg, 2016; 49(2); 668-74
27. Diamond JM, Lee JC, Kawut SM, Clinical risk factors for primary graft dysfunction after lung transplantation: Am J Respir Crit Care Med, 2013; 187(5); 527-34
28. Syrett A, Huang A, Transfusion and primary graft dysfunction after lung transplantation: All about the ratio?: J Cardiothorac Vasc Anesth, 2020; 34(11); 3033-35
29. Weber D, Cottini SR, Locher P, Association of intraoperative transfusion of blood products with mortality in lung transplant recipients: Perioper Med (Lond), 2013; 2(1); 20
Figures
Tables
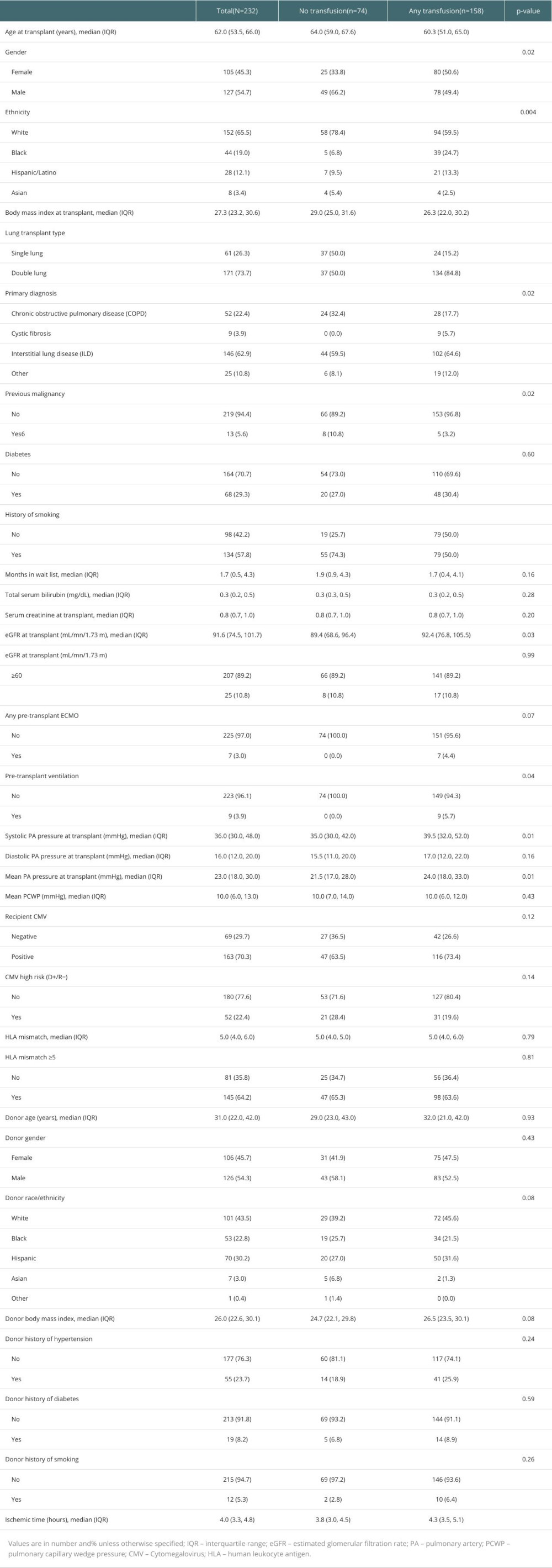 Table 1. Baseline demographics and clinical characteristics.
Table 1. Baseline demographics and clinical characteristics.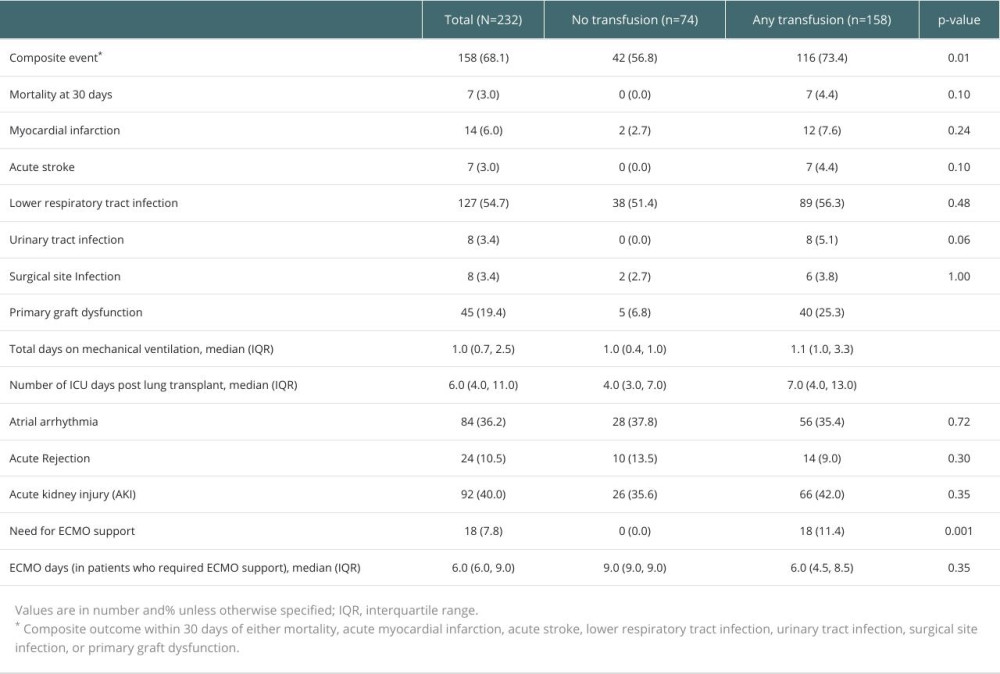 Table 2. Outcomes at 30 days after lung transplantation.
Table 2. Outcomes at 30 days after lung transplantation.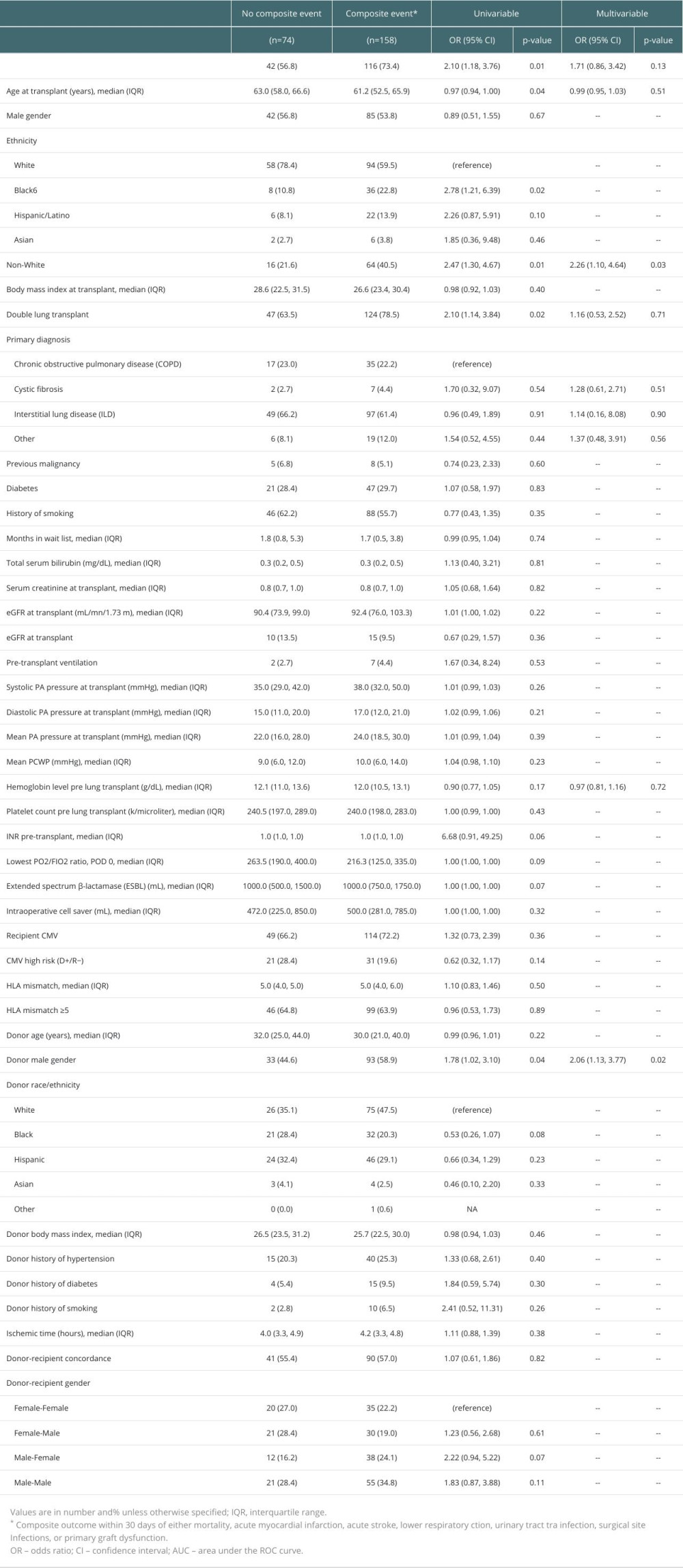 Table 3. Characteristics associated with the occurrence of composite events – univariable logistic regression.
Table 3. Characteristics associated with the occurrence of composite events – univariable logistic regression.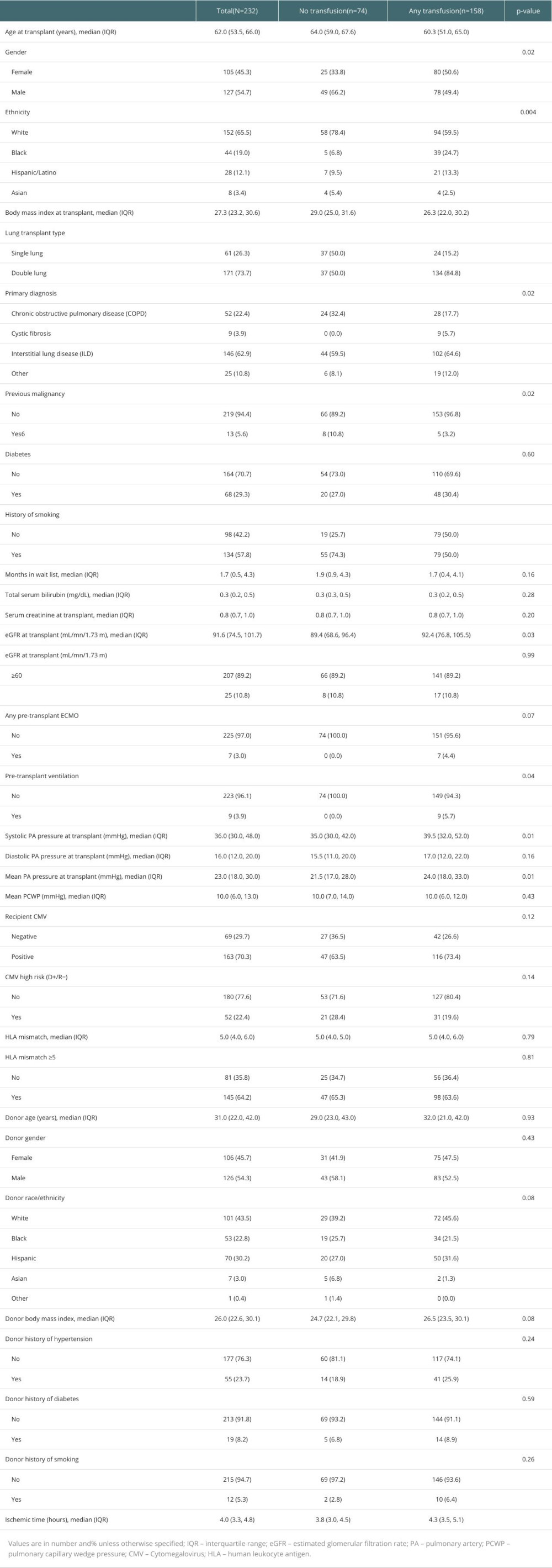 Table 1. Baseline demographics and clinical characteristics.
Table 1. Baseline demographics and clinical characteristics.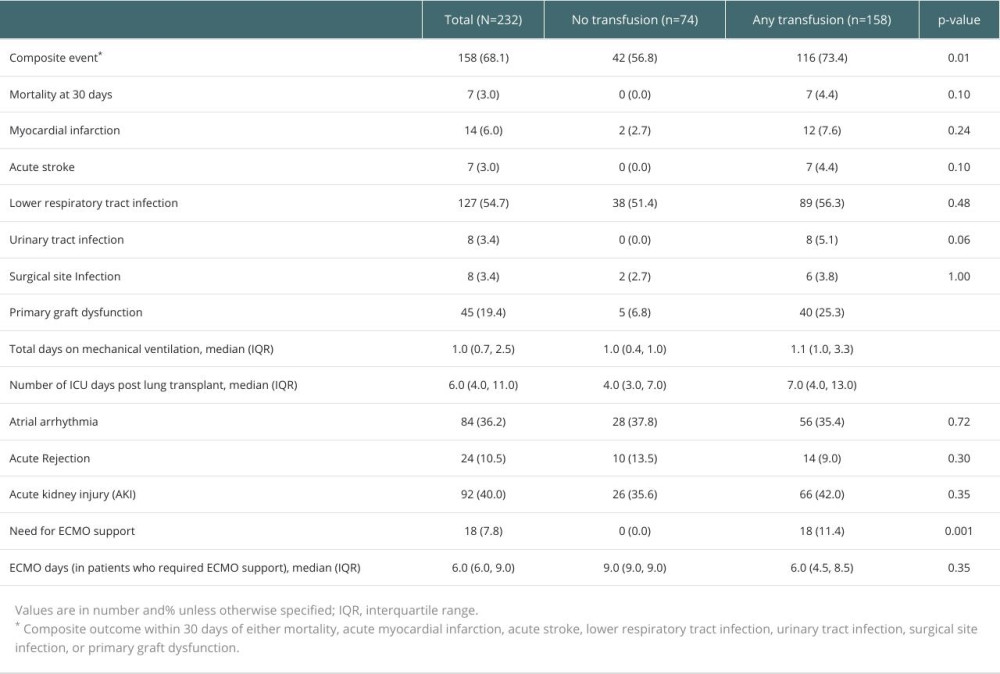 Table 2. Outcomes at 30 days after lung transplantation.
Table 2. Outcomes at 30 days after lung transplantation.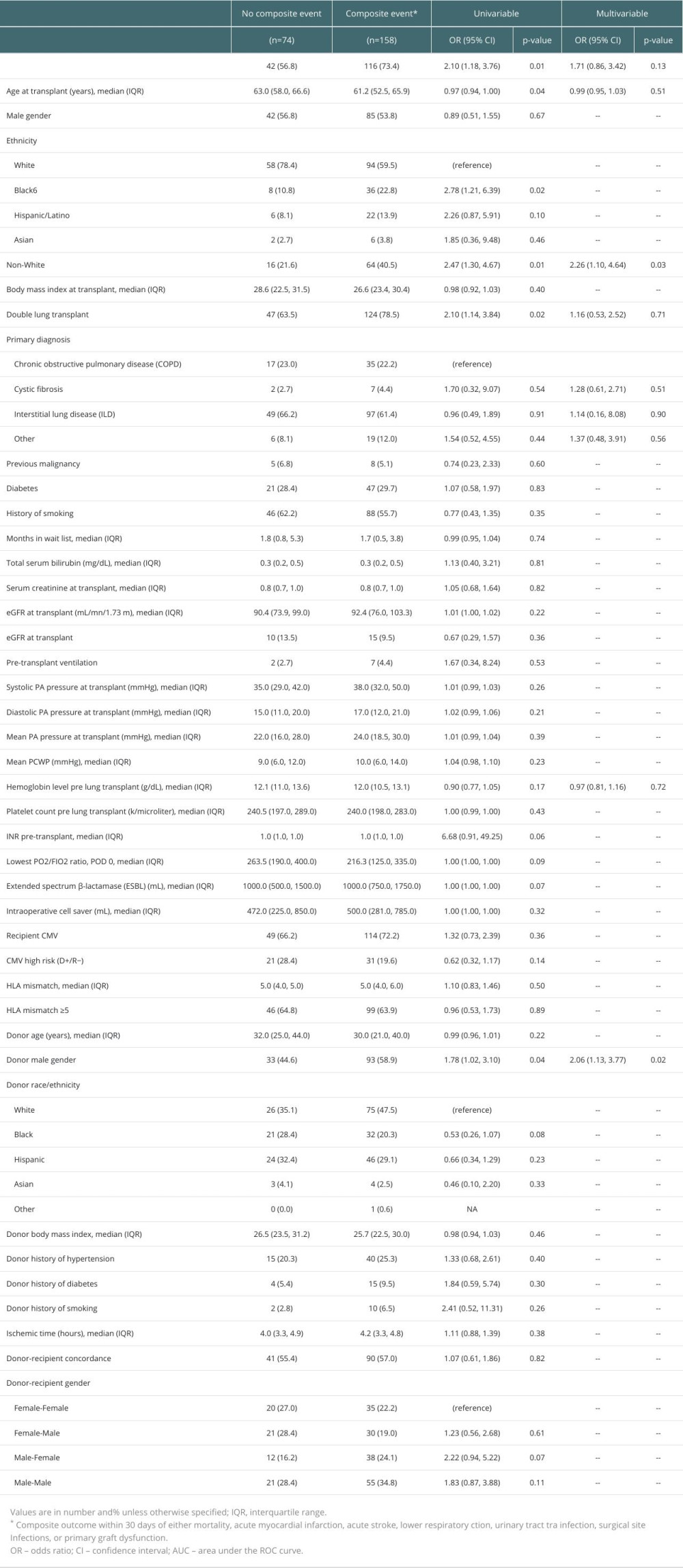 Table 3. Characteristics associated with the occurrence of composite events – univariable logistic regression.
Table 3. Characteristics associated with the occurrence of composite events – univariable logistic regression. In Press
18 Mar 2024 : Original article
Does Antibiotic Use Increase the Risk of Post-Transplantation Diabetes Mellitus? A Retrospective Study of R...Ann Transplant In Press; DOI: 10.12659/AOT.943282
20 Mar 2024 : Original article
Transplant Nephrectomy: A Comparative Study of Timing and Techniques in a Single InstitutionAnn Transplant In Press; DOI: 10.12659/AOT.942252
28 Mar 2024 : Original article
Association Between FEV₁ Decline Rate and Mortality in Long-Term Follow-Up of a 21-Patient Pilot Clinical T...Ann Transplant In Press; DOI: 10.12659/AOT.942823
02 Apr 2024 : Original article
Liver Transplantation from Brain-Dead Donors with Hepatitis B or C in South Korea: A 2014-2020 Korean Organ...Ann Transplant In Press; DOI: 10.12659/AOT.943588