01 July 2020: Case Report
Successful Treatment of Pseudomembranous Colitis with Fecal Microbiota Transplantation – A Case Study on A Patient Rescued by Extracorporeal Cardiopulmonary Resuscitation After Cardiac Arrest
Guang-Qing Huang1BC, Yong Bai1CD, Ze-Qun Sun2D, Jie Liu1AE*DOI: 10.12659/AOT.923283
Ann Transplant 2020; 25:e923283
Abstract
BACKGROUND: Pseudomembranous colitis (PMC) is an opportunistic, nosocomial infection caused by Clostridium difficile.
CASE REPORT: Here we described a patient who developed PMC during her recovery from cardiac arrest. A 16-year-old female high school student experienced sudden cardiac arrest. Spontaneous circulation was not returned by standard cardiopulmonary resuscitation. After her admission to the emergency unit, her cardiac function and neurologic function were finally resumed by extracorporeal cardiopulmonary resuscitation (ECPR); however, after 14 days, her recovery was complicated with excessive diarrhea and shock. Colonoscopy confirmed the diagnosis of PMC. Metronidazole and vancomycin were immediately administered; however, the treatment did not result in any improvement. Fecal microbiota transplantation was then performed, and after 4 transplantations, her diarrhea was significantly ameliorated. After hospital stay for 135 days, the patient was finally discharged with grade II brain function. She later recovered self-care ability in follow-up.
CONCLUSIONS: The patient suffered from a long-term gastrointestinal ischemia-hypoxia resulting from cardiac arrest. The use of broad-spectrum antibiotics in the later treatment led to refractory PMC, which was successfully managed by multiple fecal microbiota transplantation.
Keywords: case reports, Death, Sudden, Cardiac, Enterocolitis, Pseudomembranous, Adolescent, Anti-Bacterial Agents, Cardiopulmonary Resuscitation, Clostridioides difficile, Fecal Microbiota Transplantation, Heart Arrest, metronidazole, Vancomycin
Background
Cardiac arrest represents a major cause of death in well-developed countries. In the United States and Canada, cardiac arrest causes more than 300 000 deaths, while in China, according to the epidemiological data of the World Health Organization, there are nearly a half million cases of cardiac arrest-related deaths.
The 2015 American Heart Association (AHA) Guidelines for Cardiopulmonary Resuscitation indicates that extracorporeal cardiopulmonary resuscitation (ECPR) may be considered in patients who cannot recover spontaneous circulation or have repeated episodes of cardiac arrest after conventional cardiopulmonary resuscitation. Indeed, it has been reported that prompt ECPR would rescue ~36% of the hospitalized patients with cardiac arrest [1].
However, the recovery of resuscitated patients is always complicated with pseudomembranous colitis (PMC). The administration of antibacterial agents in resuscitated patients can cause an imbalance of intestinal flora, leading to an uncontrolled propagation of
Case Report
A 16-year-old female who weighted 60 kg suddenly lost consciousness when she was running in her physical education class (at ~11: 20 on April 16, 2018). CPR was immediately applied before the patient was admitted to the Emergency Department of our hospital around ~11: 40. CPR was continuously applied; however, spontaneous circulation was not returned. At noon, ECPR was performed using femoral cannula kit (Medtronics) combined with Stöckert centrifugal pump and D905 EOS membrane oxygenator. At 13: 00, extracorporeal membrane oxygenation (ECMO) was successfully established with a speed of 2650 rpm and a flow rate of 3.6 L/minute. Heparin was administered to maintain an activated clotting time (ACT) of 160–200 seconds. Around 14: 00, spontaneous heart rate returned, and an hour later, the patient was transferred to the Intensive Care Unit (ICU) because of respiratory and cardiac arrest.
The patient had no history of drug or food allergy. Admission examination indicated a body temperature of 35°C (rectal), a heart rate of 112 bpm, and blood pressure of 85/52 mm Hg. Under ECMO and ventilator-care, the patient was under deep coma and upon examination, no pupillary reflex was observed, with both eyes showing a pupil size of 6 mm. No other abnormalities were observed in the examination. The patient was given balanced salt together with lansoprazole and anti-infective (i.e., meropenem and vancomycin). There was no urine output in 6 hours. Continuous renal replacement therapy (CRRT) in series with ECMO was then used from April 16 to April 18.
On April 17, shivering and left lower extremity edema (the side where the tube was placed) were observed. Ultrasonography indicated a reduction in the arterial blood flow of the left lower extremity, so papaverine was administered. Thermotherapy was also applied. Both eyes resumed pupillary reflex, with the pupils constricted to a diameter of 3 mm. Sedative and analgesic drugs were stopped; however, both were continued after the patient exhibited painful expression and limb expression.
On April 18, left lower extremity swelling became more severe and pale, and more importantly, the blood flow into the left lower extremity completely restricted on ultrasonography. Echocardiography indicated an ejection fraction (EF) of 42%. At 17: 50 on the same day, ECMO was stopped (total duration of ECMO was about 50 hours). Blood flow to the left lower extremity subsequently resumed; however, no urine output was seen. Therefore, CRRT was performed with the right internal jugular vein as the vascular access (during the period from April 18 to May 21).
On April 19, enteral nutrition was started, and on April 23 anti-infective therapy was switched to cefoperazone/sulbactam. On April 25, the patient breathed spontaneously, although she was still in a shallow coma with diminished coughing. Percutaneous dilatation tracheostomy was therefore performed. The ventilator was withdrawn on April 26. On April 30, the patient developed diarrhea (light-yellow stools) accompanied with high fever (40°C) and shock. Sputum culture was positive for
On May 2, considering the possibility of PMC, the combined regimen of vancomycin (0.5 g, every 6 hours via nasogastric tube) and metronidazole (0.5 g, every 6 hours intravenous medical drip) was applied. Diarrhea was not mitigated, with a frequency of 20–40 times a day and a volume of 3000–4000 mL. On May 5, bedside colonoscopy suggested PMC (Figure 1). To this end, the original anti-infectives were changed to piperacillin/tazobactam and at the same time, treatment strategy was adjusted to protect the integrity of the intestinal mucosa, to modulate intestinal flora and to ensure water-electrolyte balance. Disappointedly, these approaches did not ameliorate diarrhea in a significant manner.
On May 15, dark red diarrhea was observed. Hematochezia and poisoning symptoms became more severe. In view of this, the first fecal microbiota transplantation (5 U) using the microbiota from the Chinese FMT Bank was performed. Thereafter, diarrhea was slightly improved, with the volume reduced to about 1500–2000 mL. Two additional FMTs were done on May 20 and May 22. The patient’s diarrhea was further mitigated, and the stool color changed from red to yellow. On May 23, nasogastric feeding of lactose-free formula milk started, and since then, the number of diarrheas was reduced to 10 times a day with a volume of 1000 mL. The fourth FMT was done on June 2. After this transplantation, diarrhea was further significantly improved to 2–4 times a day with a volume of 300–600 mL. Gradual transition to total enteral nutrition started on June 3.
On June 5, the tracheotomy was closed. On June 18, the patient was significantly improved and coronary computed tomography angiography (CTA) was performed to determine the cause of cardiac arrest. CTA suggested that the origin of the right coronary artery was at the top of the sinus in this patient (Figure 2). Due to functional impairment of the left lower limb, starting from June 21, the patient received rehabilitation therapy. On August 29, the patient was finally discharged with grade II brain function. After 6 months of follow-up, the patient restored her self-care ability.
Discussion
The right coronary artery originates normally in the middle of the adjacent aortic sinus. Abnormality in the origin of the coronary artery can be seen in 0.3% to 2% of the population, and among them, extremely rare cases show that the right coronary artery originates from the top of the sinus [5,6]. Most patients with an anomalous coronary origin have no obvious clinical symptoms with good prognosis, but some can be inflicted with heart failure, myocardial infarction, arrhythmia, and sudden cardiac death [7–9]. This study presented a case of sudden cardiac death that was attributed to the rare coronary origin at the top of the sinus. Fortunately, prompt CPR was applied, allowing the patient to be further rescued using ECMO.
ECMO-supported CPR is commonly named as ECPR. It has been indicated that the success rate of ECPR for hospitalized patients is 34% to 36%, and the success rate of out-of-hospital cardiac arrest patients ranges 4% to 36% [1]. For CPR, for every 1-minute increase in the duration, the probability of spontaneous recovery and survival of the patient is reduced by 1% and 4%, respectively. Stub et al. concluded from his findings from multiple centers that the survival rate of patients with cardiac arrest would drop to zero if the duration elapsed before ECMO establishment was longer than 60 minutes [10]. In this case, despite the time-to-ECMO of nearly 100 minutes, the patient was successfully discharged from hospital after treatment with different complications. Similar cases, to our best knowledge, are rarely seen in ECPR reports.
Unfortunately, although our patient resumed a good neurological outcome after ECPR, she suffered from excessive diarrhea and shock, which are the clinical presentation of PMC. The underlying cause of PMC was attributed to the imbalance of the intestinal flora that resulted from the administration of antibacterial agents. The uncontrolled propagation of
Comparing to the brain and heart, the digestive organs can tolerate a longer duration of ischemia and hypoxia. However, if digestive organs were widely distributed anatomically, the full recovery from dysfunctions would be a slow process. This would substantially affect the prognosis of patients after cardiac arrest. In ECPR, in addition to early cardiopulmonary and cerebral resuscitation, the functional recovery of the digestive system is a key determinant of patient’s survival. Broad-spectrum antibiotics are often administered as a prophylactic approach for infection; however, its excessive use has been identified as a risk factor for PMC.
Conclusions
In this report we presented a patient who suffered from prolonged gastrointestinal ischemia-hypoxia due to cardiac arrest. The use of broad-spectrum antibiotics in subsequent treatment led to refractory PMC, which was successfully managed by multiple rounds of fecal microbiota transplantation.
Figures
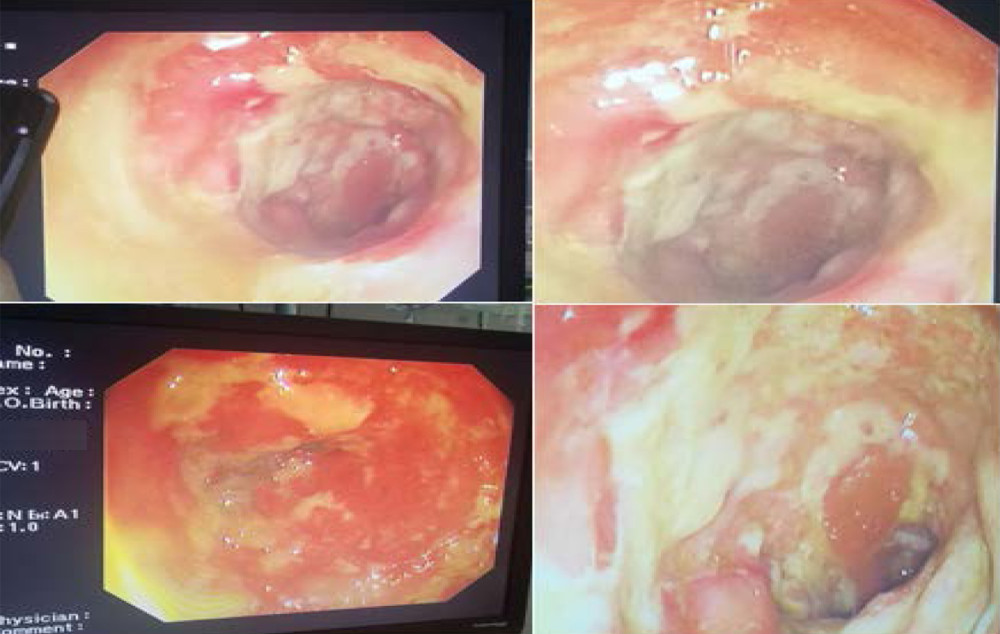 Figure 1. Bedside colonoscopy confirmed the diagnosis of pseudomembranous colitis in our patient.
Figure 1. Bedside colonoscopy confirmed the diagnosis of pseudomembranous colitis in our patient. 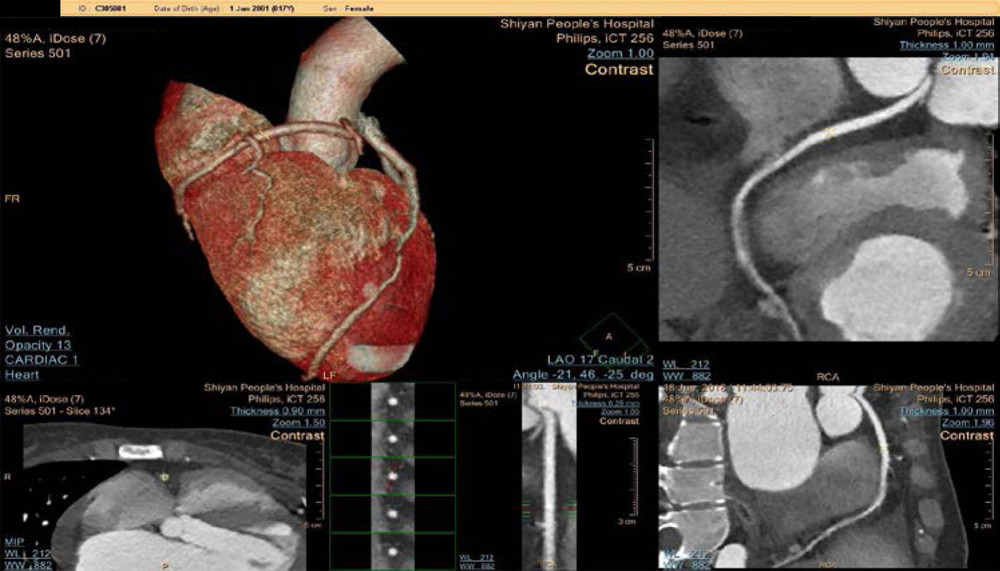 Figure 2. Coronary computed tomography angiography (CTA) was performed to delineate the underlying cause of cardiac arrest. The imaging finding suggests that the origin of the right coronary artery is at the top of the sinus. In the CTA, anomaly of origin of the right coronary artery was observed, in which the right coronary artery origin was above the intersinus ridge. The right coronary artery traveled between the aortic root and the right ventricular outflow tract. During strenuous exercise, the patient’s right ventricular outflow tract would thicken, compressing the right coronary artery origin, leading to myocardial ischemia and cardiac arrest.
Figure 2. Coronary computed tomography angiography (CTA) was performed to delineate the underlying cause of cardiac arrest. The imaging finding suggests that the origin of the right coronary artery is at the top of the sinus. In the CTA, anomaly of origin of the right coronary artery was observed, in which the right coronary artery origin was above the intersinus ridge. The right coronary artery traveled between the aortic root and the right ventricular outflow tract. During strenuous exercise, the patient’s right ventricular outflow tract would thicken, compressing the right coronary artery origin, leading to myocardial ischemia and cardiac arrest. References
1. Massetti M, Gaudino M, De Paulis S, Extracorporeal membrane oxygenation for resuscitation and cardiac arrest management: Heart Fail Clin, 2014; 10(1 Suppl); S85-93
2. Surawicz CM, Brandt LJ, Binion DG: Am J Gastroenterol, 2013; 108(4); 478-98 quiz 499
3. Kelly CR, de Leon L, Jasutkar N: J Clin Gastroenterol, 2012; 46(2); 145-49
4. Burke KE, Lamont JT: J Am Geriatr Soc, 2013; 61(8); 1394-98
5. Jacobs JP, Introduction: December 2015 heart week issue of cardiology in the young – highlights of heartweek 2015: Challenges and dilemmas of pediatric cardiac care including heart failure in children and congenital abnormalities of the coronary arteries: Cardiol Young, 2015; 25(8); 1441-55
6. Yeh DD, Ghoshhajra B, Inglessis-Azuaje I, Massive pulmonary artery aneurysm causing left main coronary artery compression in the absence of pulmonary hypertension: Tex Heart Inst J, 2015; 42(5); 465-67
7. Turiy Y, Douglas W, Balaguru D, Anomalous origin of coronary artery from main pulmonary artery in hypoplastic left heart syndrome: Ann Thorac Surg, 2015; 100(6); 2346-48
8. Llerena-Butron S, Sevilla T, Revilla-Orodea A, San Roman JA, Anomalous origin of the left coronary artery from the right sinus of valsalva: Two abnormal courses in one patient: Eur Heart J Cardiovasc Imaging, 2016; 17(2); 231
9. Suryanarayana P, Kollampare S, Movahed MR, Anomalous origin of the right coronary artery from the left anterior descending artery with anomalous course between the great vessels: A case for conservative management with review of the literature: Rev Cardiovasc Med, 2015; 16(3); 221-24
10. Stub D, Bernard S, Pellegrino V, Refractory cardiac arrest treated with mechanical CPR, hypothermia, ECMO and early reperfusion (the CHEER trial): Resuscitation, 2015; 86; 88-94
11. McDonald LC, Gerding DN, Johnson S: Clin Infect Dis, 2018; 66(7); e1-48
12. Bauer MP, van Dissel JT: Int J Antimicrob Agents, 2009; 33(Suppl 1); S51-56
Figures
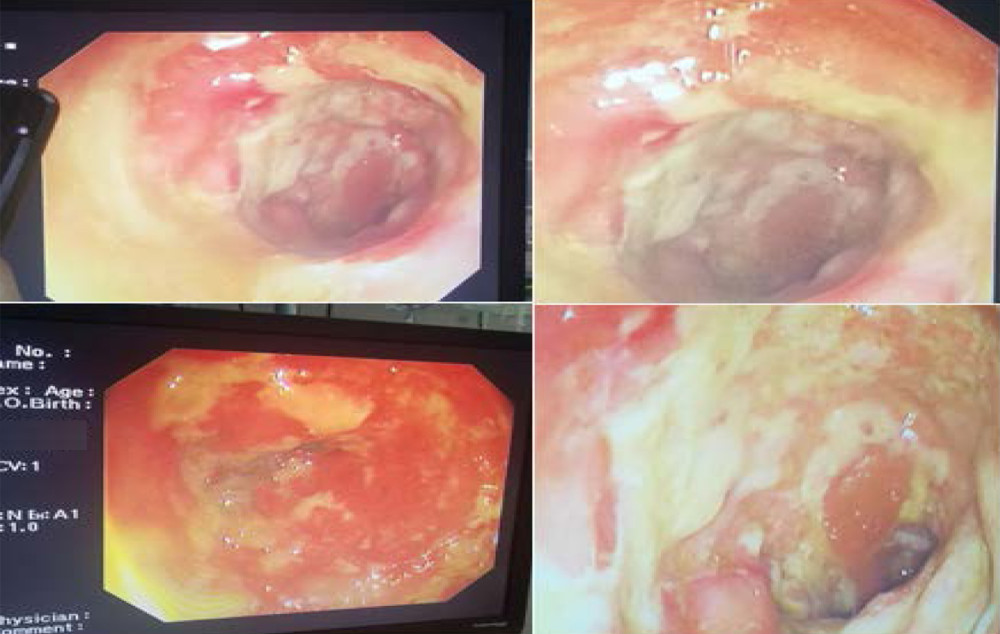 Figure 1. Bedside colonoscopy confirmed the diagnosis of pseudomembranous colitis in our patient.
Figure 1. Bedside colonoscopy confirmed the diagnosis of pseudomembranous colitis in our patient.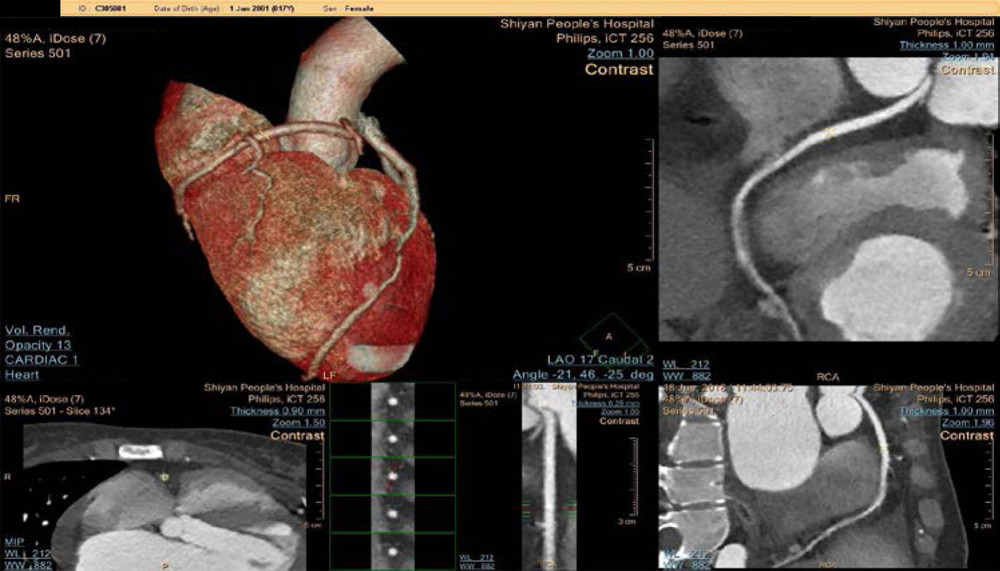 Figure 2. Coronary computed tomography angiography (CTA) was performed to delineate the underlying cause of cardiac arrest. The imaging finding suggests that the origin of the right coronary artery is at the top of the sinus. In the CTA, anomaly of origin of the right coronary artery was observed, in which the right coronary artery origin was above the intersinus ridge. The right coronary artery traveled between the aortic root and the right ventricular outflow tract. During strenuous exercise, the patient’s right ventricular outflow tract would thicken, compressing the right coronary artery origin, leading to myocardial ischemia and cardiac arrest.
Figure 2. Coronary computed tomography angiography (CTA) was performed to delineate the underlying cause of cardiac arrest. The imaging finding suggests that the origin of the right coronary artery is at the top of the sinus. In the CTA, anomaly of origin of the right coronary artery was observed, in which the right coronary artery origin was above the intersinus ridge. The right coronary artery traveled between the aortic root and the right ventricular outflow tract. During strenuous exercise, the patient’s right ventricular outflow tract would thicken, compressing the right coronary artery origin, leading to myocardial ischemia and cardiac arrest. In Press
18 Mar 2024 : Original article
Does Antibiotic Use Increase the Risk of Post-Transplantation Diabetes Mellitus? A Retrospective Study of R...Ann Transplant In Press; DOI: 10.12659/AOT.943282
20 Mar 2024 : Original article
Transplant Nephrectomy: A Comparative Study of Timing and Techniques in a Single InstitutionAnn Transplant In Press; DOI: 10.12659/AOT.942252
28 Mar 2024 : Original article
Association Between FEV₁ Decline Rate and Mortality in Long-Term Follow-Up of a 21-Patient Pilot Clinical T...Ann Transplant In Press; DOI: 10.12659/AOT.942823
02 Apr 2024 : Original article
Liver Transplantation from Brain-Dead Donors with Hepatitis B or C in South Korea: A 2014-2020 Korean Organ...Ann Transplant In Press; DOI: 10.12659/AOT.943588
Most Viewed Current Articles
05 Apr 2022 : Original article
Impact of Statins on Hepatocellular Carcinoma Recurrence After Living-Donor Liver TransplantationDOI :10.12659/AOT.935604
Ann Transplant 2022; 27:e935604
12 Jan 2022 : Original article
Risk Factors for Developing BK Virus-Associated Nephropathy: A Single-Center Retrospective Cohort Study of ...DOI :10.12659/AOT.934738
Ann Transplant 2022; 27:e934738
22 Nov 2022 : Original article
Long-Term Effects of Everolimus-Facilitated Tacrolimus Reduction in Living-Donor Liver Transplant Recipient...DOI :10.12659/AOT.937988
Ann Transplant 2022; 27:e937988
15 Mar 2022 : Case report
Combined Liver, Pancreas-Duodenum, and Kidney Transplantation for Patients with Hepatitis B Cirrhosis, Urem...DOI :10.12659/AOT.935860
Ann Transplant 2022; 27:e935860








