28 April 2023: Original Paper
Effect of Sodium Bicarbonate Ringer’s Solution on Intraoperative Blood Gas Analysis and Postoperative Recovery Time in Liver Transplantation: A Single-Center Retrospective Study
Haiyan Xian1BDF, Qiuwen Xie1BCE, Ke Qin1AG, Xiangfei Ma1CE, Xueke Du1AEG*DOI: 10.12659/AOT.939097
Ann Transplant 2023; 28:e939097
Abstract
BACKGROUND: Sodium bicarbonate Ringer’s solution (BRS) is the latest generation of balanced crystal solutions. BRS does not increase the liver burden, but its impact in liver transplantation is unclear. The aim of this study was to investigate the effect of BRS as a fluid therapy on intraoperative blood gas analysis and postoperative recovery time in orthotopic liver transplantation (LT) patients.
MATERIAL AND METHODS: The study included 101 patients who received classical in situ liver transplantation at the Second Affiliated Hospital of Guangxi Medical University from November 2019 to January 2022. The patients were divided into 2 groups according to the intraoperative fluid infusion: the BRS group and the sodium lactate Ringer’s solution group (LRS group). Intraoperative blood gas analysis, including pH, base excess (BE), bicarbonate, and lactic acid levels of radial artery blood, were collected after induction (T0), 30 min before opening (T1), 30 min after no liver period (T2), 30 min after opening (T3), and at the end of the operation (T4). Postoperative ICU catheter time, ICU stay time, and total hospitalization days were also recorded and compared between the 2 groups.
RESULTS: Lactic acid levels were decreased significantly at T3 in the BRS group (P<0.05). ICU catheter time, ICU hospitalization days, and total hospitalization days were significantly shorter in the BRS group (P<0.05).
CONCLUSIONS: BRS can decrease the lactic acid level at 30 min after opening, reducing the postoperative recovery time. BRS is more effective than LRS in liver transplantation.
Keywords: Liver Transplantation, Retrospective Studies, Ringer's Solution, Sodium Bicarbonate, Humans, Isotonic Solutions, China, Lactic Acid, Blood Gas Analysis
Background
Liver transplantation (LT) is the most effective and radical treatment for end-stage liver disease [1,2]. Perioperative fluid therapy is very important and complex and can affect the prognosis of patients [3,4]. LT is associated with large trauma, and bleeding and severe hemodynamic fluctuations may occur during the perioperative period, leading to a water-electrolyte disorder [5,6]. Therefore, liquid treatment is particularly important in LT.
At present, the commonly used crystal solutions for LT during the perioperative period are normal saline and lactate Ringer’s solution. The massive infusion of normal saline is likely to cause hyperchloremia and renal vasoconstriction, leading to hyperchloremic acidosis [7]. In a prospective, randomized, controlled study of liver transplantation, sodium bicarbonate Ringer’s solution was found to reduce the incidence and severity of AKI after classical orthotopic liver transplantation compared with normal saline [8]. Under normal circumstances, to prevent lactic acidosis, 70% of LA is rapidly metabolized by the liver as a substrate for aerobic energy fuel or glucose production. Lactic acid (LA) in LRS is metabolized in the liver and multiple intakes can lead to hyperlactatemia and increase the burden of the new liver after transplantation [9–11]. In a retrospective study of liver transplant recipients, elevated arterial LA levels after liver transplantation were associated with increased intraoperative blood loss, prolonged ICU stays, and increased mortality [12]. Therefore, it is very important to select the appropriate fluid rehydration method for liver transplantation patients.
BRS is the latest generation of balanced crystal solutions, containing bicarbonate ions and electrolyte ions (eg, sodium, potassium, calcium) in physiological concentrations, similar to extracellular fluids, without lactic acid (LA) [13]. As a buffer system, hydrogen carbonate can rapidly combine with H + to correct acidosis, and does not increase the liver burden through respiratory metabolism [14]. Paul et al demonstrated that BRS significantly reduced acetate rush in cardiac surgery patients compared to Ringer acetate. Recently, Lv et al showed that BRS could better maintain pH status in liver transplant patients [15]. To sum up, BRS has advantages in liquid treatment of liver transplantation compared with commonly used crystal solutions [16]. However, the effect of BRS on fluid therapy for liver transplantation remains unclear due to the few studies reported to date. The purpose of this study was to compare the effects of LRS and BRS on intraoperative blood gas analysis and postoperative recovery time of orthotopic LT, so as to provide a basis for the selection of appropriate fluid replacement methods.
Material and Methods
PATIENTS:
We retrospectively analyzed patients aged >18 years old with ASA grade III–IV who underwent a classical in situ liver transplant at the Second Affiliated Hospital of Guangxi Medical University from November 2019 to January 2022. There was no significant difference in MELD scores. The following patients were excluded from the analysis: patients who received both LRS and BRS; those with a split, piggyback, live LT; simultaneous liver and kidney transplantation; donor-related data missing; and diagnosis of hepatolenticular degeneration, liver failure, or acute severe viral hepatitis. This was a retrospective study and all aspects of the study design were retrospective. All data were extracted from the medical records system. This study was approved by the Ethics Committee of the Second Affiliated Hospital of Guangxi Medical University, Nanning, China.
PERIOPERATIVE MANAGEMENT:
The patients were forbidden to drink and eat before surgery. Multiple groups of upper limb venous pathways were opened after the patient entered the operating room. ECG, invasive blood pressure (IBP), noninvasive blood pressure (NIBP), oxygen saturation (SpO2), and patients were routinely monitored. Etomidate 0.2–0.3 mg/kg, sufentanil 0.3–0.6 μg/kg, and rocuronium 0.6 mg/kg were injected intravenously. Mechanical ventilation parameters: tidal volume 6–8 ml/kg, respiratory rate (RR) 10–13 times/min, oxygen flow 2 L/min, and end-expiratory carbon dioxide partial pressure (PETCO2) 35–45 mmHg. Anesthesia was maintained by inhalation combined with intravenous anesthesia, continuous infusion of propofol 4–12 mg/(kg·h), remifentanil 0.5–2 μg/kg/min, cisatracurium 3 μg/kg/min, and inhalation of 1–2% sevoflurane.
Sodium bicarbonate Ringer’s solution was used in the sodium bicarbonate Ringer’s solution (BRS) group. Sodium lactate Ringer’s solution was used for the sodium lactate Ringer’s solution (LRS) group. Free hemodynamic management was used during the operation to guide intravenous crystal infusion. At the same time, blood transfusion was performed according to blood transfusion guidelines. Perioperative blood management of patients followed the WS/T 623–2018 Guidelines for Transfusion of Whole Blood and Blood Components. There was no significant difference in the use of vasoactive drugs and coagulation factors. After the operation, tracheal intubation was retained and the patient was transferred to the ICU.
SURGICAL TECHNIQUE AND POSTOPERATIVE CARE:
Type of surgical technique: classical orthotopic liver transplantation. Four surgeons performed the operation. All the operations were performed by the same group of surgeons.
STUDY OUTCOMES:
INTRAOPERATIVE BLOOD GAS ANALYSIS DATA:
Arterial blood gas: pH, base excess (BE), bicarbonate (HCO3−), and LA levels in radial artery blood were recorded after induction (T0), 30 min before opening (T1), 30 min after no liver period (T2), 30 min after opening (T3), and the end of the operation (T4).
POSTOPERATIVE RECOVERY TIME:
Postoperative ICU catheter time, ICU stay time, and total hospitalization days.
STATISTICAL ANALYSIS:
Data analysis was performed using GraphPad prism8.0 software. Assuming that the missing data was random, multiple interpolation methods were used to fill in the missing value. Measurement data with a normal distribution were expressed as mean±standard deviation and compared between the 2 groups using the independent sample
Results
There was no statistically significant difference between the 2 groups for age, gender, operation time, bleeding volume, urine volume, blood transfusion volume, and sodium bicarbonate crystal usage (
There was no significant difference in pH, BE, and HCO3− between the 2 groups from T0 to T4 or LA between T0–T2 and T4 (
Compared with the LRS group, postoperative ICU catheter time (Figure 2A), hospital stay (Figure 2B), and ICU stay (Figure 2C) were significantly shorter in the BRS group (
Discussion
Here, we retrospectively analyzed perioperative fluid therapy in 101 patients with orthotopic liver transplantation. We primarily found that BRS reduced LA levels during LT, and reduced postoperative extubation time, ICU stay, and total hospital stay. Our results suggest that BRS can be safely used for intraoperative fluid replacement in patients with in situ LT, with superior efficacy to LRS.
After opening during LT, a large number of ischemic products and large amounts of potassium, acidic substances, cryoprotectant, and vasoactive substances in the transplanted liver and intestinal veins rapidly enter the circulation. This results in obvious hemodynamic changes, which can easily lead to a water-electrolyte disorder and accumulation of LA in the patients [17–20]. Therefore, for liver transplant patients, intraoperative input of LRS will increase liver and kidney load and is not an ideal crystal solution. BRS is a physiological alkaline buffer with HCO3, which is a direct alkaline effect by binding with H + to quickly correct the acidosis and maintain acid-base balance [21,22]. BRS is a new type of balanced crystal buffered by bicarbonate rather than organic anions, in which case it may perform better at preserving the acid-base state [23]. This was consistent with the results of our retrospective study, in which we found that the LA level in the BRS group was significantly lower than that in the LRS group at T3. This was also shown in the prospective study of liver transplant recipients conducted by Lv et al. BRS could better maintain pH status in liver transplant patients. Therefore, we speculate that the use of BRS solution during liver transplantation can quickly correct acidosis, reduce LA accumulation, and maintain acid-base balance.
Perioperative fluid balance and different fluid management strategies are associated with postoperative complications. Different fluid management strategies can improve intraoperative bleeding, mechanical ventilation time, and ICU stays time [24–26]. Our retrospective study showed that time spent in the ICU, length of stay in ICU, and total length of stay in ICU were reduced with BRS. This may be due to the fact that bicarbonate is completely independent of liver metabolism, relieving the burden of liver transplantation. Moreover, compared with other crystal solutions, sodium bicarbonate Ringer’s solution is closer to the plasma component, which can not only effectively supplement the circulating blood volume, but also correct metabolic acidosis, and shorten the postoperative recovery time of patients with liver transplantation, which is conducive to the postoperative recovery of patients. Similar phenomena were also observed in animal experiments. The introduction of BRS in rabbits improved metabolic acidosis caused by hemorrhagic shock, maintained acid-base balance, and improved organ and tissue damage caused by a hemorrhagic shock in different degrees [13]. Meanwhile, Wu et al also showed that the mechanical ventilation duration, ICU stay, and postoperative stay of liver transplant recipients receiving BRS Queen were shorter than those in the NS group [8]. Therefore, the effect of BRS in liver transplantation is better than that of LRS in shortening postoperative recovery time.
There are some limitations to this retrospective analysis. There are many factors that affect blood gas and LA levels during LT, including fluid use (crystallographic fluid infusion), the patient’s vital signs, hemoglobin levels, and pre- and postoperative liver function. Although there was no significant difference in the use of sodium bicarbonate between the 2 groups, we did not collect preoperative and intraoperative vital signs or preoperative and postoperative indicators of liver and kidney function. This is a limitation of the study and it is necessary for us to conduct further prospective controlled studies in the future. In addition, this was a single-center study.
Conclusions
In summary, BRS can decrease the lactic acid level 30 min after opening, and reduce the postoperative recovery time. BRS is more effective than LRS in liver transplantation.
Figures
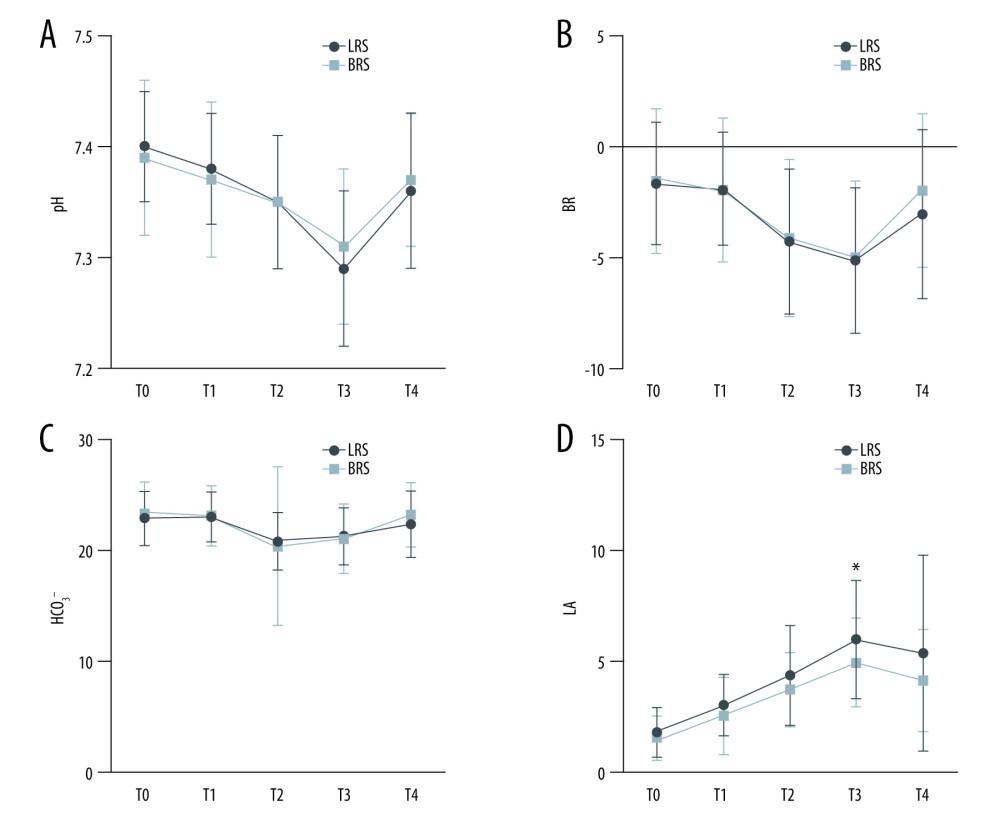 Figure 1. Changes of blood gas analysis at different time points during the operation. (A) pH value; (B) base excess (BE); (C) bicarbonate (HCO3−); (D) lactic acid (LA) levels. T0: post-induction monitoring; T1: 30 min before opening; T2: 30 min after anhepatic stage; T3: 30 min after opening; T4: No further action is required. T0: monitored after induction; T1: 30 min before opening; T2: 30 min after no liver period; T3: 30 min after opening; T4: the end of the operation. Data are the mean±SD. * P<0.05 between the 2 groups. LRS – sodium lactate Ringer’s solution; BRS – sodium bicarbonate Ringer’s solution; n – number of patients. Data analysis was performed using GraphPad prism8.0 software (GraphPad Software).
Figure 1. Changes of blood gas analysis at different time points during the operation. (A) pH value; (B) base excess (BE); (C) bicarbonate (HCO3−); (D) lactic acid (LA) levels. T0: post-induction monitoring; T1: 30 min before opening; T2: 30 min after anhepatic stage; T3: 30 min after opening; T4: No further action is required. T0: monitored after induction; T1: 30 min before opening; T2: 30 min after no liver period; T3: 30 min after opening; T4: the end of the operation. Data are the mean±SD. * P<0.05 between the 2 groups. LRS – sodium lactate Ringer’s solution; BRS – sodium bicarbonate Ringer’s solution; n – number of patients. Data analysis was performed using GraphPad prism8.0 software (GraphPad Software). 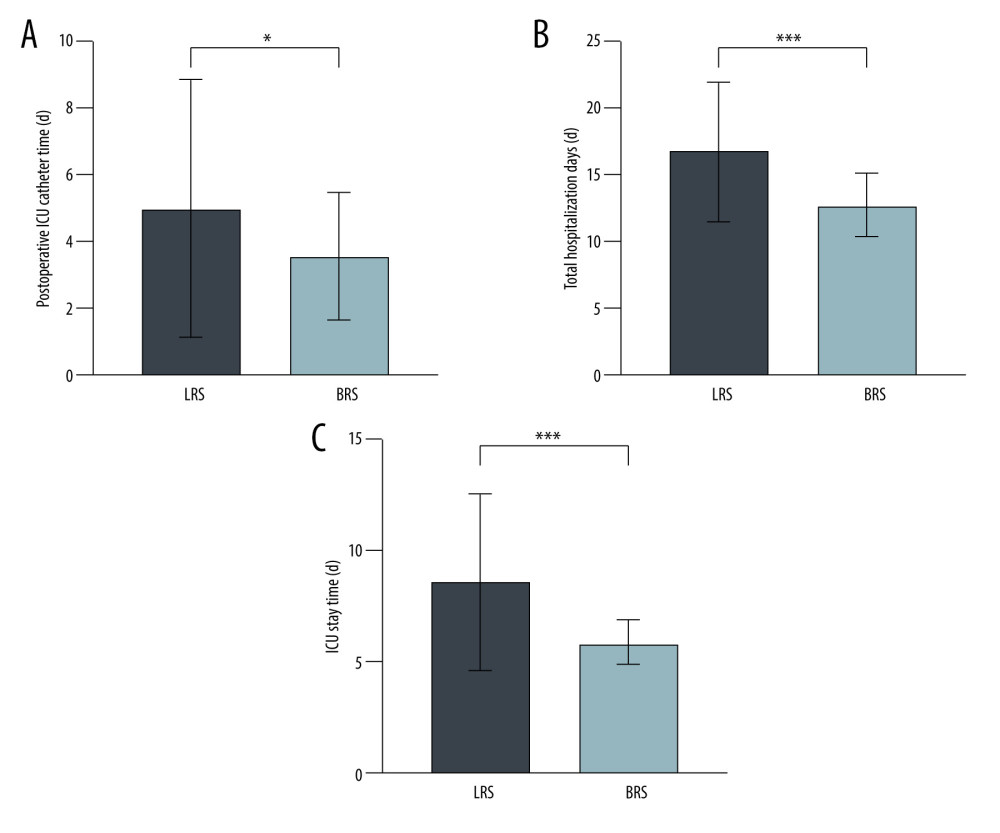 Figure 2. Postoperative recovery time in both groups. (A) Postoperative ICU catheter time; (B) total hospitalization days; (C) ICU stay time. T0: monitored after induction; T1: 30 min before opening; T2: 30 min after no liver period; T3: 30 min after opening; T4: the end of the operation. Data are the mean±SD. * P<0.05 between the 2 groups. LRS – sodium lactate Ringer’s solution; BRS – sodium bicarbonate Ringer’s solution; n – number of patients. Data analysis was performed using GraphPad prism8.0 software (GraphPad Software).
Figure 2. Postoperative recovery time in both groups. (A) Postoperative ICU catheter time; (B) total hospitalization days; (C) ICU stay time. T0: monitored after induction; T1: 30 min before opening; T2: 30 min after no liver period; T3: 30 min after opening; T4: the end of the operation. Data are the mean±SD. * P<0.05 between the 2 groups. LRS – sodium lactate Ringer’s solution; BRS – sodium bicarbonate Ringer’s solution; n – number of patients. Data analysis was performed using GraphPad prism8.0 software (GraphPad Software). References
1. Olivo R, Guarrera JV, Pyrsopoulos NT, Liver transplantation for acute liver failure: Clin Liver Dis, 2018; 22; 409-17
2. Samuel D, Coilly A, Management of patients with liver diseases on the waiting list for transplantation: A major impact to the success of liver transplantation: BMC Med, 2018; 16; 113
3. Grace E, Keir AK, Fluid therapy: Friend or foe?: Clin Perinatol, 2020; 47; 515-28
4. Harris T, Coats TJ, Elwan MH, Fluid therapy in the Emergency Department: An expert practice review: Emerg Med J, 2018; 35; 511-15
5. Marques HP, Barros I, Li J, Current update in domino liver transplantation: Int J Surg, 2020; 82s; 163-68
6. Gitto S, Falcini M, Marra F, Metabolic disorders after liver transplantation: Metab Syndr Relat Disord, 2021; 19; 65-69
7. Xue M, Zhang X, Liu F, Effects of chloride content of intravenous crystalloid solutions in critically ill adult patients: A meta-analysis with trial sequential analysis of randomized trials: Ann Intensive Care, 2019; 9; 30
8. Wu H, Meng G, Zuo C, The Effects of sodium bicarbonate Ringer’s solution on acute kidney injury and the clinical outcomes after liver transplantation: A randomized controlled trial: Front Pharmacol, 2022; 13; 982472
9. Andersen LW, Mackenhauer J, Roberts JC, Etiology and therapeutic approach to elevated lactate levels: Mayo Clin Proc, 2013; 88; 1127-40
10. Kraut JA, Madias NE, Lactic acidosis: N Engl J Med, 2014; 371; 2309-19
11. Dai WB, Chen LK, Qi SY, Lactated Ringer’s solution versus normal saline in pediatric living-donor liver transplantation: A matched retrospective cohort study: Paediatr Anaesth, 2021; 31; 702-12
12. Jipa LN, Tomescu D, Droc G, The interrelation between arterial lactate levels and postoperative outcome following liver transplantation: Rom J Anaesth Intensive Care, 2014; 21; 106-12
13. Wang L, Lou J, Cao J, Bicarbonate Ringer’s solution for early resuscitation in hemorrhagic shock rabbits: Ann Transl Med, 2021; 9; 462
14. Ma J, Han S, Liu X, Zhou Z, Sodium bicarbonated Ringer’s solution effectively improves coagulation function and lactic acid metabolism in patients with severe multiple injuries and traumatic shock: Am J Transl Res, 2021; 13; 5043-50
15. Davies PG, Venkatesh B, Morgan TJ, Plasma acetate, gluconate and interleukin-6 profiles during and after cardiopulmonary bypass: A comparison of Plasma-Lyte 148 with a bicarbonate-balanced solution: Crit Care, 2011; 15; R21
16. Lv C, Zhou B, Zhang D, The effects of bicarbonated versus acetated Ringer’s solutions on acid-base status and kidney injury following orthotopic liver transplantation: Protocol for a single-centre, randomised controlled trial (The BETTER trial): Front Surg, 2022; 9; 1019570
17. Takahashi K, Jafri SR, Safwan M, Peri-transplant lactate levels and delayed lactate clearance as predictive factors for poor outcomes after liver transplantation: A propensity score-matched study: Clin Transplant, 2019; 33; e13613
18. Golse N, Guglielmo N, El Metni A, Arterial lactate concentration at the end of liver transplantation is an early predictor of primary graft dysfunction: Ann Surg, 2019; 270; 131-38
19. Rohrig R, Wegewitz C, Lendemans S, Superiority of acetate compared with lactate in a rodent model of severe hemorrhagic shock: J Surg Res, 2014; 186; 338-45
20. Nadeem A, Salahuddin N, El Hazmi A, Chloride-liberal fluids are associated with acute kidney injury after liver transplantation: Crit Care, 2014; 18; 625
21. Yu LQ, Meng CC, Jin XS, Cai J, Clinical study of sodium bicarbonated Ringer’s solution on fluid resuscitation of patients with hemorrhagic shock: Eur Rev Med Pharmacol Sci, 2022; 26; 1535-42
22. Bian Y, Xu T, Le Y, Li S, The efficacy and safety of sodium bicarbonate Ringer’s solution in critically ill patients: A retrospective cohort study: Front Pharmacol, 2022; 13; 829394
23. Zhang J, Han D, Zhang K, Observation on the effectiveness and safety of sodium bicarbonate Ringer’s solution in the early resuscitation of traumatic hemorrhagic shock: A clinical single-center prospective randomized controlled trial: Trials, 2022; 23; 825
24. Carrier FM, Chassé M, Sylvestre MP, Effects of intraoperative fluid balance during liver transplantation on postoperative acute kidney injury: An observational cohort study: Transplantation, 2020; 104; 1419-28
25. Carrier FM, Chassé M, Wang HT, Restrictive fluid management strategies and outcomes in liver transplantation: A systematic review: Can J Anaesth, 2020; 67; 109-27
26. Carrier FM, Sylvestre MP, Massicotte L, Effects of intraoperative hemodynamic management on postoperative acute kidney injury in liver transplantation: An observational cohort study: PLoS One, 2020; 15; e0237503
Figures
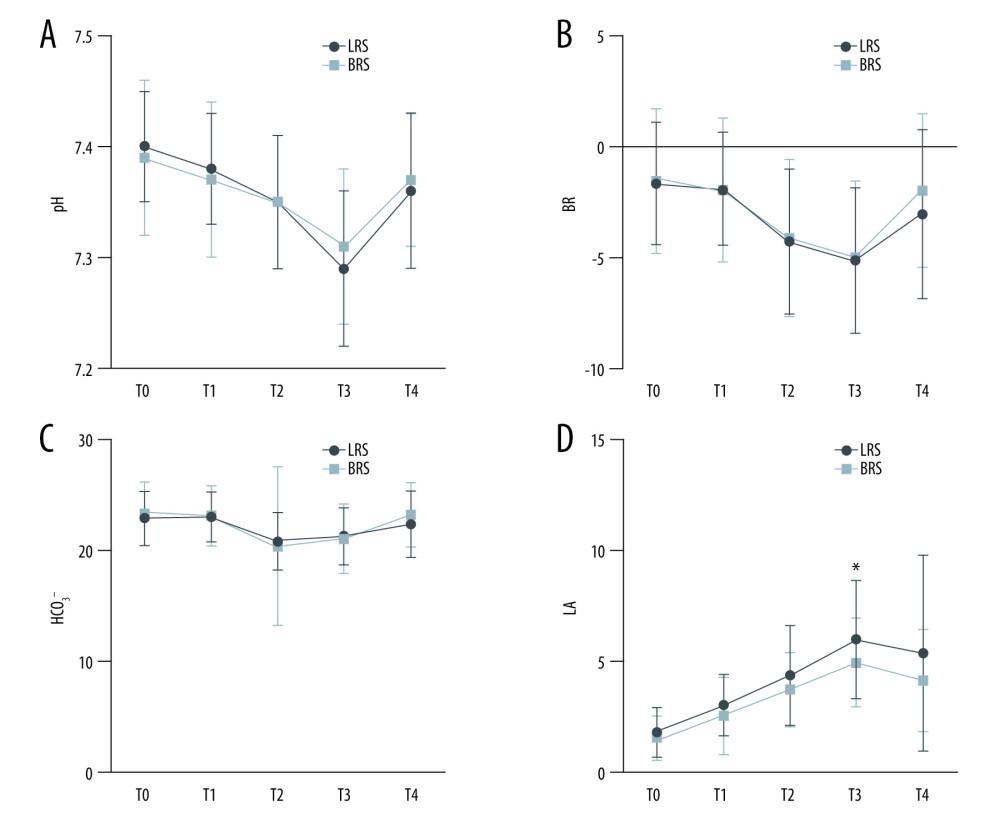 Figure 1. Changes of blood gas analysis at different time points during the operation. (A) pH value; (B) base excess (BE); (C) bicarbonate (HCO3−); (D) lactic acid (LA) levels. T0: post-induction monitoring; T1: 30 min before opening; T2: 30 min after anhepatic stage; T3: 30 min after opening; T4: No further action is required. T0: monitored after induction; T1: 30 min before opening; T2: 30 min after no liver period; T3: 30 min after opening; T4: the end of the operation. Data are the mean±SD. * P<0.05 between the 2 groups. LRS – sodium lactate Ringer’s solution; BRS – sodium bicarbonate Ringer’s solution; n – number of patients. Data analysis was performed using GraphPad prism8.0 software (GraphPad Software).
Figure 1. Changes of blood gas analysis at different time points during the operation. (A) pH value; (B) base excess (BE); (C) bicarbonate (HCO3−); (D) lactic acid (LA) levels. T0: post-induction monitoring; T1: 30 min before opening; T2: 30 min after anhepatic stage; T3: 30 min after opening; T4: No further action is required. T0: monitored after induction; T1: 30 min before opening; T2: 30 min after no liver period; T3: 30 min after opening; T4: the end of the operation. Data are the mean±SD. * P<0.05 between the 2 groups. LRS – sodium lactate Ringer’s solution; BRS – sodium bicarbonate Ringer’s solution; n – number of patients. Data analysis was performed using GraphPad prism8.0 software (GraphPad Software).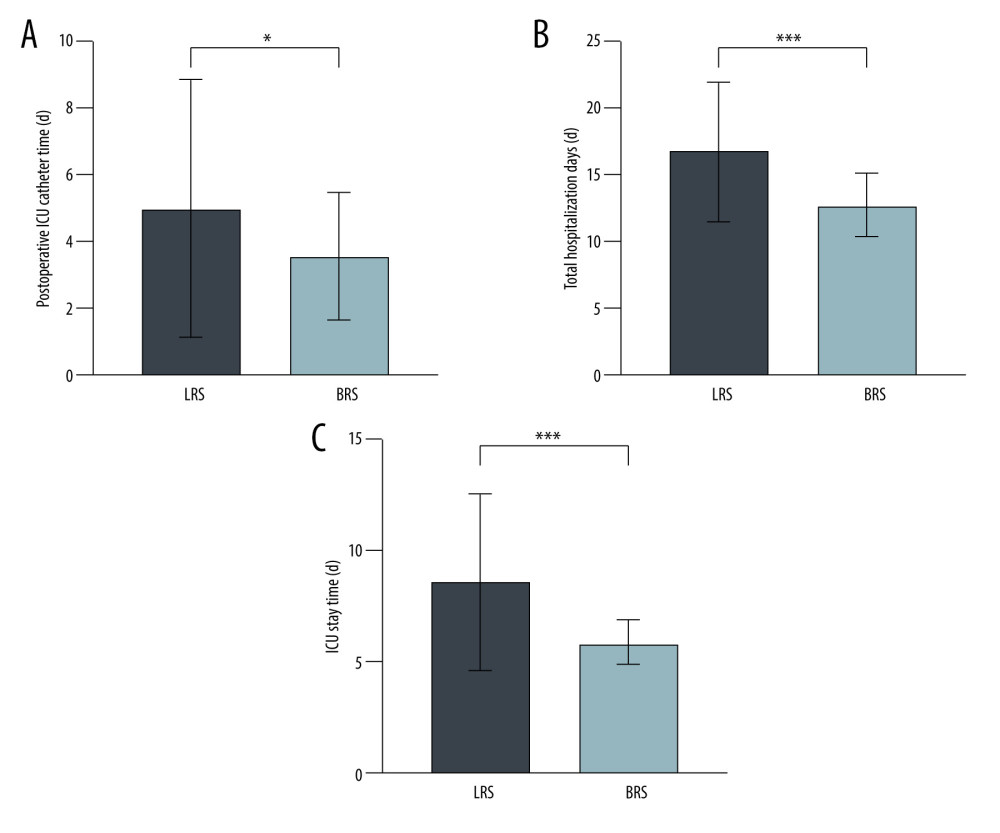 Figure 2. Postoperative recovery time in both groups. (A) Postoperative ICU catheter time; (B) total hospitalization days; (C) ICU stay time. T0: monitored after induction; T1: 30 min before opening; T2: 30 min after no liver period; T3: 30 min after opening; T4: the end of the operation. Data are the mean±SD. * P<0.05 between the 2 groups. LRS – sodium lactate Ringer’s solution; BRS – sodium bicarbonate Ringer’s solution; n – number of patients. Data analysis was performed using GraphPad prism8.0 software (GraphPad Software).
Figure 2. Postoperative recovery time in both groups. (A) Postoperative ICU catheter time; (B) total hospitalization days; (C) ICU stay time. T0: monitored after induction; T1: 30 min before opening; T2: 30 min after no liver period; T3: 30 min after opening; T4: the end of the operation. Data are the mean±SD. * P<0.05 between the 2 groups. LRS – sodium lactate Ringer’s solution; BRS – sodium bicarbonate Ringer’s solution; n – number of patients. Data analysis was performed using GraphPad prism8.0 software (GraphPad Software). Tables
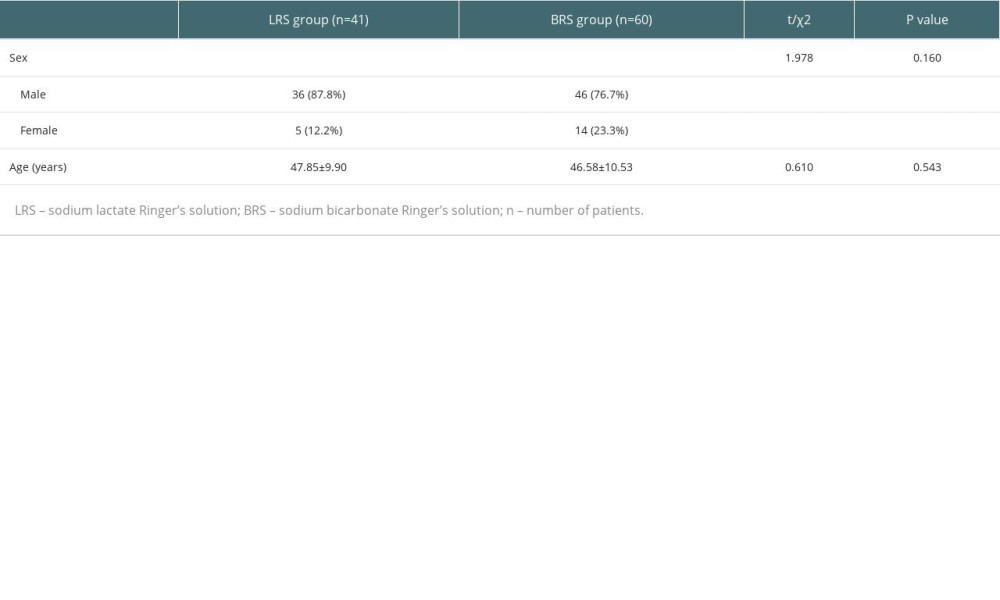 Table 1. Baseline characteristics of the patients. Data are the mean±SD, or median (interquartile range: 25–75%).
Table 1. Baseline characteristics of the patients. Data are the mean±SD, or median (interquartile range: 25–75%).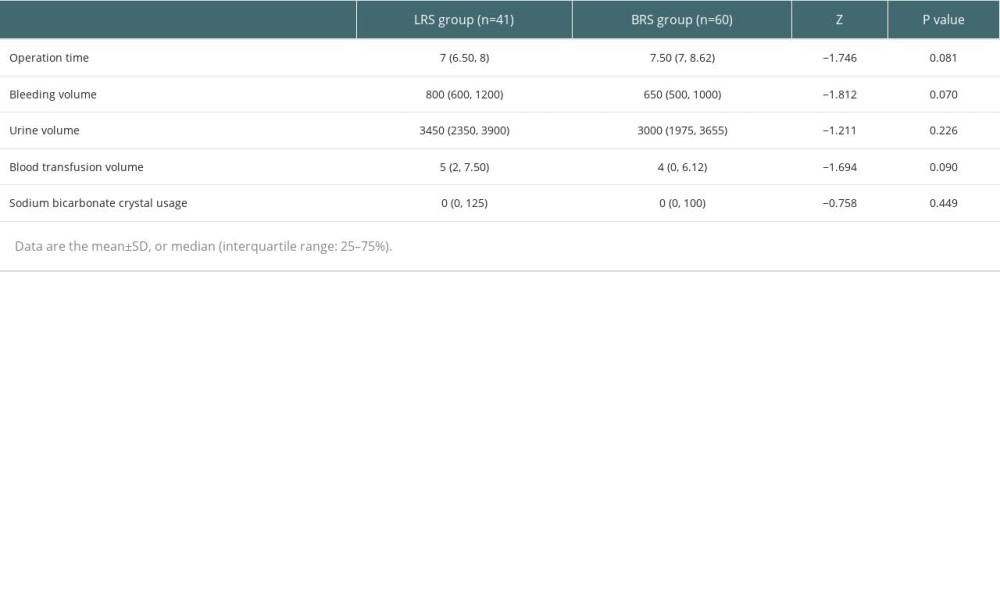 Table 2. Intraoperative factors in the 2 groups.
Table 2. Intraoperative factors in the 2 groups.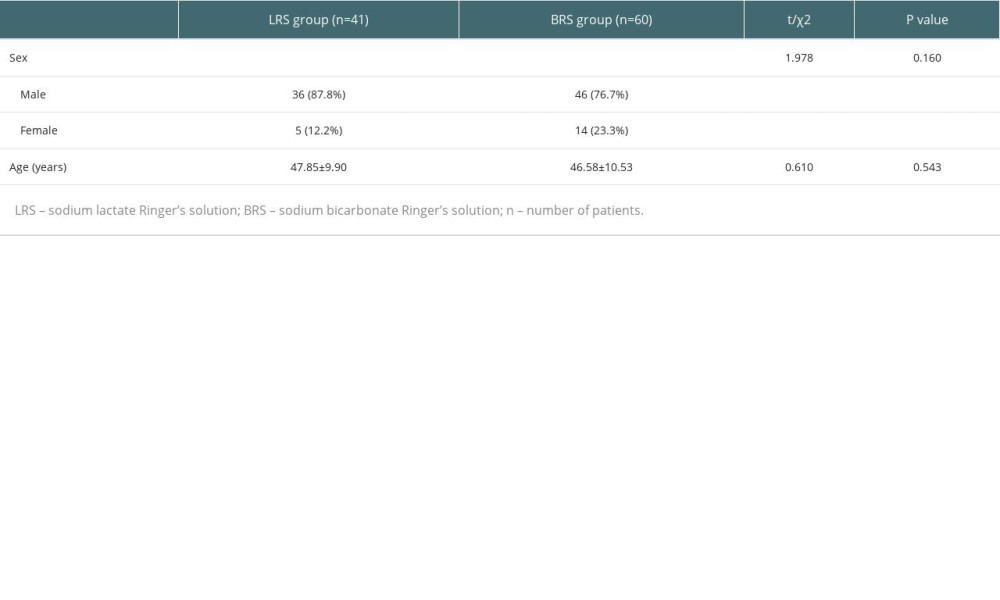 Table 1. Baseline characteristics of the patients. Data are the mean±SD, or median (interquartile range: 25–75%).
Table 1. Baseline characteristics of the patients. Data are the mean±SD, or median (interquartile range: 25–75%).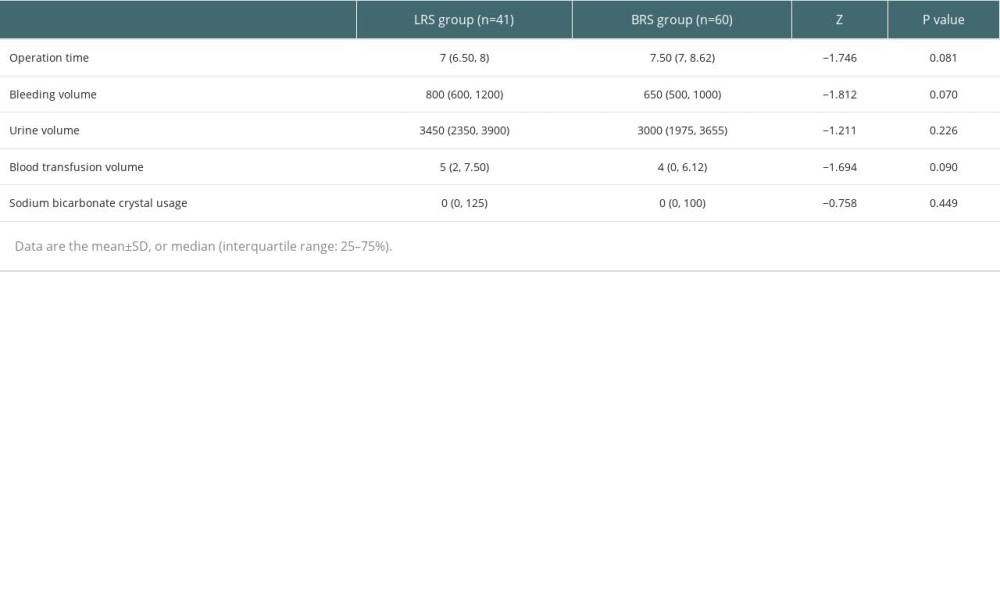 Table 2. Intraoperative factors in the 2 groups.
Table 2. Intraoperative factors in the 2 groups. In Press
18 Mar 2024 : Original article
Does Antibiotic Use Increase the Risk of Post-Transplantation Diabetes Mellitus? A Retrospective Study of R...Ann Transplant In Press; DOI: 10.12659/AOT.943282
20 Mar 2024 : Original article
Transplant Nephrectomy: A Comparative Study of Timing and Techniques in a Single InstitutionAnn Transplant In Press; DOI: 10.12659/AOT.942252
28 Mar 2024 : Original article
Association Between FEV₁ Decline Rate and Mortality in Long-Term Follow-Up of a 21-Patient Pilot Clinical T...Ann Transplant In Press; DOI: 10.12659/AOT.942823
02 Apr 2024 : Original article
Liver Transplantation from Brain-Dead Donors with Hepatitis B or C in South Korea: A 2014-2020 Korean Organ...Ann Transplant In Press; DOI: 10.12659/AOT.943588
Most Viewed Current Articles
05 Apr 2022 : Original article
Impact of Statins on Hepatocellular Carcinoma Recurrence After Living-Donor Liver TransplantationDOI :10.12659/AOT.935604
Ann Transplant 2022; 27:e935604
12 Jan 2022 : Original article
Risk Factors for Developing BK Virus-Associated Nephropathy: A Single-Center Retrospective Cohort Study of ...DOI :10.12659/AOT.934738
Ann Transplant 2022; 27:e934738
22 Nov 2022 : Original article
Long-Term Effects of Everolimus-Facilitated Tacrolimus Reduction in Living-Donor Liver Transplant Recipient...DOI :10.12659/AOT.937988
Ann Transplant 2022; 27:e937988
15 Mar 2022 : Case report
Combined Liver, Pancreas-Duodenum, and Kidney Transplantation for Patients with Hepatitis B Cirrhosis, Urem...DOI :10.12659/AOT.935860
Ann Transplant 2022; 27:e935860








