01 December 2020: Original Paper
MELD Score Reflects the Mood, Sleep, and Daily Living Ability in Liver Transplantation Candidates: A Descriptive Study
Kaiji Ni1ABDE, Chenglin Li2BCDEF, Yongbing Qian3AB, Xia Sun1E, Yan Zhan4B, Ting Zeng5B, Siqi Zhu2B, Qiang Xia3A, Wei Feng1CDE*, Yanli Luo1AEGDOI: 10.12659/AOT.926857
Ann Transplant 2020; 25:e926857
Abstract
BACKGROUND: This study aimed to assess the psychosocial status (mood, sleep quality, and activities of daily living) of candidates on an orthotopic liver transplantation (OLT) waiting list and to identify the association between psychosocial factors and MELD score in end-stage liver disease (ESLD).
MATERIAL AND METHODS: Fifty-three OLT waiting list candidates completed 4 scales (Hamilton Rating Scale for Depression [HAMD-17], Hamilton Anxiety Rating Scale [HAM-A], Pittsburgh Sleep Quality Index [PSQI], Activities of Daily Living Scale [ADL]) to assess their affective status, sleep quality, and daily living ability. Candidates were divided into 2 groups, the high MELD score group (MELD score ≥15) and the low MELD score group (MELD score <15), and statistical analyses, including the Spearman test for correlation and the Mann-Whiney U-test, were conducted.
RESULTS: The high MELD group had significantly higher scores than the low MELD score group for HAM-A (P=0.024), PSQI (P=0.021), and ADL (P=0.000). In addition, the MELD score was positively correlated with HAMD-17 (r=0.362, P<0.01), HAM-A (r=0.430, P<0.01), PSQI (r=0.289, P<0.05), and ADL (r=0.585, P<0.01).
CONCLUSIONS: MELD score could be a comprehensive indicator in OLT for more promptly detecting biopsychosocial problems derived from ESLD. It also provides a reference for both medical and psychosocial intervention before and after OLT.
Keywords: Activities of Daily Living, Anxiety, Depression, Liver Transplantation, Sleep Disorders, Waiting Lists, Affect, End stage liver disease, Liver, Severity of Illness Index, Sleep
Background
End-stage liver disease (ESLD) not only causes severe physical deterioration, but it can also lead to psychological issues [1]. The development of orthotopic liver transplantation (OLT) has improved long-term survival and the quality of life of recipients [2], and the 1-, 10-, and 18-year survival rates associated with adult OLT have reached 83% to 88%, 68% to 72%, and 48% to 56%, respectively [3]. However, due to the gap between supply and demand, candidates are placed on waiting lists and may have to wait for a long time before receiving the transplant. During this time, patients face multiple stressors: declining physical health; constant worry about whether the procedure will take place on time and, more importantly, in time [4]; the financial cost; and so forth.
The combination of these stressors can contribute to psychological disorders such as anxiety and depression. The prevalence rates for anxiety and depression have been estimated to be 14% to 52% and 17% to 60%, respectively [4]. Pretransplant depression and anxiety affect posttransplant health-related quality of life (HRQOL) [5]. Furthermore, pretransplant depression also affects posttransplant psychiatric morbidity [6], while anxiety can negatively affect the course of the disease by impairing adherence to treatment [7].
Sleep disturbance, including compromised sleep quality, has been reported among liver transplantation candidates on a waiting list [8]. Furthermore, sleep disturbance has a prevalence of 48% to 81% in patients with liver cirrhosis, which is much higher than in the general population [9]. Therefore, sleep disturbance appears to be a particular problem in waiting list candidates.
Deficits in activities of daily living are common in patients with ESLD. Functional decline, polypharmacy, and cognitive impairment, which is often seen in elderly patients, may contribute to the high risk of physical disability. These deficits can be a predictor of mortality and, more importantly, they could determine posttransplant disability reversion for candidates on a waiting list [10].
These considerations indicate a need to improve the mental and sleep status of patients. Thus, it is important to identify the predictors of disability and the factors related to psychological disorders and sleep disturbance that could be recapitulated in the patients’ psychosocial factors. Such predictors and factors should be used as the basis for developing diagnostic and therapeutic interventions because they could help prevent the worsening of candidates’ symptoms and the negative consequences.
The model for end-stage liver disease (MELD) score was initially created to predict the survival of transjugular intrahepatic portosystemic shunts but then applied as a standard metric to reflect the severity of liver diseases [11]. The MELD score has been statistically proved to predict 3-month mortality and to indicate the severity of ESLD. Thus, it is used as a determining factor for the OLT waiting list in accord with the idea of “the sickest first” [12]. Patients with a MELD score ≥15 are considered eligible to be placed on the waiting list. However, an exception exists for several diseases, whereby severity is not indicated by a higher MELD score [13]. A national study of the US liver transplant database revealed that a higher survival benefit was found in patients with a higher MELD score. A pretransplant MELD score of 31 to 34 predicted a 43 times greater relative life expectancy, while a MELD score of 35 to 40 had a 128 times higher expectation [14]. In addition to its ability to predict physiological outcomes, the MELD score also exhibits the potential to simultaneously reveal psychological outcomes in terms of health-related quality of life (HRQOL). Higher posttransplant HRQOL was found in patients with a higher pretransplant MELD score [13,15,16]. However, more research should be done to verify the correlation between MELD scores and psychological issues. Furthermore, the association between MELD score and sleep disturbance and daily living abilities remains unclear.
Thus, this study aimed to assess the affective status, sleep quality, and daily living abilities of candidates on the OLT waiting list at a single center in China and to identify the association between these factors and disease severity as represented by the MELD score.
Material and Methods
STUDY DESIGN:
This cross-sectional, single-center study included 53 pretransplant patients for whom surgery was indicated were recruited from the ward of the liver transplantation center of Renji Hospital, Shanghai, China, from May to December 2019. This study was approved by the Ethics Committee of Renji Hospital (No. [2017] 164).
The inclusion criteria required study participants to (1) meet the indications for liver transplantation in Renji Hospital; (2) be age 18 or older; (3) agree to participate in the study in person; and (4) sign informed consent. The exclusion criteria were (1) having schizophrenia, bipolar disorder, or any other severe mental disorder; and (2) having significant diseases, other than hepatic diseases, such as cardiovascular, respiratory, renal, endocrine, and immune diseases.
Informed consent was obtained from all participants. Afterward, they provided their personal information, including sex, highest education, occupation, economic status, marital status, and alcohol and tobacco use. They then received the scales described below from a qualified medical worker, who completed 2 clinician-rated scales and helped collect the self-rated scales from participants after they finished these instruments on their own in their wards. Four medical workers participated in the data collection and the assessment of clinician-rated instruments. They were all well trained to use a standard procedure and to avoid bias. Participants’ MELD scores were calculated from the latest blood test results. Their medical records were reviewed to obtain liver disease type, duration of illness, time on the waiting list, mental disorder history, and corresponding medication.
RATING SCALES:
Scales were used to assess participants’ depression, anxiety, sleep quality, and activities of daily living.
To assess depression and anxiety, we used the Hamilton Rating Scale for Depression (HAMD-17) [17] and the Hamilton Anxiety Rating Scale (HAM-A) [18], 2 clinician-rated scales. For sleep quality, we used the Pittsburgh Sleep Quality Index (PSQI) [19]. For assessing daily living ability, we used the Activity of Daily Living Scale (ADL) [20]. These instruments have been widely used in China and all have been translated into Chinese, including adaptation to culture and idiom.
HAMD-17 AND HAM-A:
HAMD-17 is a clinician-rated scale designed to rate the severity of major depressive disorder (MDD) symptoms. It contains 17 items that relate to the symptoms observed in MDD, such as depressed mood; feelings of guilt; suicidal ideation insomnia; lack of interest in work and activities; thought retardation; agitation; psychic anxiety; somatic anxiety; somatic symptoms; loss of libido; hypochondria; weight loss; and lack of insight. HAMD-17 is evaluated by a qualified clinician interviewing patients while observing their symptoms; items are rated on scales of 0 to 4, 0 to 2, or 0 to 3 points (based on different item sets). The higher the points, the more severe the symptoms are, with a maximum score of 52. A normal total score is 0 to 7; a total score of 8 to 16 indicates probability of depression disorder; a total score between 17 and 24 is considered to indicate moderate MDD severity; and a total score of 25 or above signals severe depression [17,21,22].
Similar to HAMD-17, HAM-A is also clinician rated, but it is designed to rate anxiety symptoms based on 14 items, such as anxious mood; tension; fears; insomnia; intellectual ability; depressed mood; somatic, sensory, cardiovascular, respiratory, gastrointestinal, genitourinary, and autonomic symptoms; and observed behavior during the interview. Each item is scored from 0 (not present) to 4 (severe), and the maximum total score is 56. A total score of 0 to 7 is normal; 8 to 16 indicates probable anxiety; 17 to 24 indicates mild anxiety; 25 to 30 indicates moderate to severe anxiety; and 30 or above indicates severe [17,23].
HAMD-17 and HAM-A have been translated into Chinese, incorporating Chinese idioms and culture, and these scales have good reliability and validity [23]. Fourteen facilities in China cooperated in studying the reliability and validity of HAMD-17, which was found to have a reliability coefficient of 0.88 to 0.99 (P<0.01). For assessing depressive disorder, the authenticity coefficient was 0.92. In a study with 19 patients with anxiety disorder, the reliability coefficient was 0.93 (P<0.01) [24]. Another study, which included 36 patients with anxiety, showed that the validity coefficient was 0.36 (P<0.05) [25].
PITTSBURG SLEEP QUALITY INDEX:
PSQI is a scale that assesses sleep quality and disturbances within the past month. It contains 19 self-rated items and 5 items that are rated by partners. The 19th self-rated item and the 5 partner-rated items are not scored. The scored 18 items relate to 7 components: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. Each component contains items that match the category, and each component is scored from 0 to 3 based on the total score of the items it contains. Each item is rated from 0 to 3, with the higher score indicating greater frequency of the problem. The maximum score is 21, and a total score of 5 or more is considered as indicating a sleep disorder [19]. The scored part (18 self-rated items) of PSQI was translated into Chinese in 1996 by Xianchen et al. [26], who also studied the reliability and validity of the scale. Their findings indicated that the Chinese version of PSQI had good internal consistency, test-retest reliability, and high concept and criterion-related validity, with a sensitivity of 98.3% and a specificity of 90.2%.
ACTIVITY OF DAILY LIVING SCALE:
ADL was developed by Lawson and Brody in 1969 [20], and it comprises the Physical Self-Maintenance Scale (PSMS) and Instrumental Activities of Daily Living Scale (IADL). The PSMS and IADL scales were developed to assess ADL and IADL, and they include 6 ADL items (eating, dressing, grooming, walking, bathing, and toileting) and 8 IADL items (telephone use, shopping, food preparation, housekeeping, laundry, public transportation use, handle finances, and taking medicines). Each of the items is rated from 1 to 4 (1, can do; 2, can do with some difficulty; 3, need some help to do; and 4, cannot do independently), and the maximum score is 56. A total score of 22 or higher indicates significantly disability in ADL [20,27].
GROUPING STANDARD:
The patients were divided into a high MELD score group (MELD score ≥15) and a low MELD score group (MELD score <15) to identify the influence of severity of disease on depression, anxiety, sleep disturbance, and ADL. We chose the cutoff point of 15 because patients with a score ≥15 are considered to be eligible to be on the waiting list and have significant survival benefit from OLT [13]. During our literature search, we found several studies using this standard [28,29].
STATISTICAL ANALYSIS:
First, the data were checked for normal distribution by the Kolmogorov-Smirnov test, and data were found to not be normally distributed. Therefore, the Spearman test for correlation was used to assay the correlation between variables. A nonparametric statistical test (the Mann-Whitney U-test) was used to verify the statistical differences between groups, with the significance being 5%. Microsoft Excel (Microsoft, Redmond, WA, USA) and SPSS 26.0 (IBM, Armonk, NY, USA) were used for data input and statistical analysis.
Results
DEMOGRAPHIC INFORMATION:
Fifty-three candidates were included as participants in this study; 41 (77.4%) were men and 12 (22.6%) were women. The average age was 52.2±12.67 years (range, 21 to 84). For educational status, we considered the highest education received by each participant. Two (3.8%) had primary education; 22 (41.5%), lower secondary education; 12 (22.6%), upper secondary education; 9 (17%), short-cycle tertiary education; 6 (11.3%), bachelor’s degree or equivalent; and 2 (3.8%), master’s degree or equivalent. For monthly income, 19 (35.8%) had a monthly income below 430 USD; 10 (18.9%) had 430 to 717 USD; 7 (13.2%) had 717 to 1147 USD; 7 (13.2%) had 1147 to 1434 USD; 2 (3.8%) had 1434 to 2151 USD; 4 (7.5%) had 2151 to 2868 USD; and 4 (7.5%) had above 2868 USD. To provide context for the income status, we note that the minimum wage in China is around 140 to 360 USD, differing by province. The marriage status was as follows: 2 (3.8%) participants were not married, 48 (90.6%) were married, and 3 (5.7%) were divorced. The average duration of illness was 47.1±66.7 months, ranging from 0.25 to 240 months. The average time on the waiting list was 1.9±2.47 months, ranging from 0 to 12 months. The most common underlying disease was hepatitis B cirrhosis (30/53; Table 1).
The average MELD score was 14.2±9.3, ranging from 3.0 to 46.0. The low MELD score group (MELD <15) included 34 (64.2%) participants, the high MELD score group (MELD ≥15) contained 18 (34.0%), and 1 participant’s MELD score was not specified (Table 1). No statistical difference was found for highest education (P=0.507), marital status (P=0.749), monthly income (P=0.721), duration of illness (P=0.779), or time on the waiting list (P=0.555) between 2 groups.
HAMD-17 RESULTS:
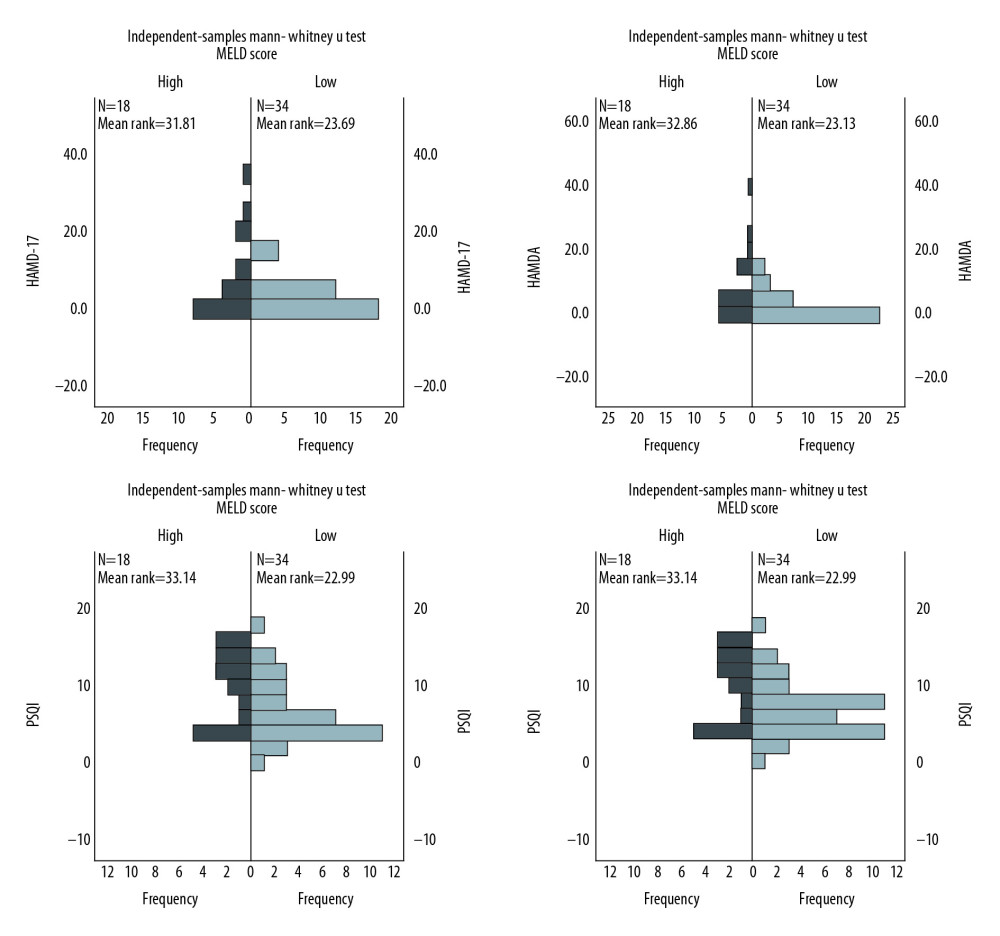
Among all participants, HAMD-17 scores ranged from 0 to 37, and 13 (24.5%) had scores ≥7, indicating they had depression. In the high MELD score group, the average HAMD-17 score was 8.4±10.3, with 7 of 18 (38.9%) having a score ≥7. The average score was 3.6±4.8, and 5 of 34 (14.7%) had a score ≥7 in the low MELD score group (Table 2). No statistical difference was found in HAMD-17 scores between the 2 groups (P=0.063), but there was a tendency toward a higher score in the high MELD score group (Figure 1).
HAM-A RESULTS:
HAM-A scores ranged from 0 to 38, and 13 (24.5%) participants had a score ≥7 and were considered to have an anxiety disorder. The average score was 9.0±10.4 in the high MELD score group and 3.1±4.5 in the low MELD score group. In the high MELD score group, 7 of 18 (38.9%) had a score ≥7, and 5 of 34 (14.7%) in the low MELD score group had a score ≥7 (Table 2). The score was significantly higher in the high MELD score group than in the low MELD score group (P=0.024; Figure 1).
PSQI RESULTS:
The minimum PSQI score was 0, while the maximum was 18. Thirty-two (59.5%) participants were considered to have a sleep disorder (total score >5): 13 of 18 (72.2%) in the high MELD score group, and 19 of 34 (55.9%) in low MELD score group. The average score was 9.5±4.8 in the high MELD score group and 6.2±4.2 in the low MELD score group (Table 2). The PSQI score was significantly higher in the high MELD score group (P=0.021; Figure 1).
ADL RESULTS:
ADL scores ranged from 14 to 41, and 14 (26.4%) participants were considered significantly disabled (score ≥22): 3 of 34 (8.8%) in the low MELD score group and 11 of 18 (61.1%) in the high MELD score group. The average score was 22.8±5.9 in the high MELD score group and 16.4±5.8 in the low MELD score group (Table 2). The ADL score was significantly higher in the high MELD score group (P=0.000; Figure 1).
RELATIONSHIP BETWEEN MELD SCORE AND THE SCALES:
The results of the Spearman correlation test showed that the MELD score is positively correlated with HAMD-17 (r =0.362, P<0.01), HAM-A (r=0.430, P<0.01), PSQI (r=0.289, P<0.05), and ADL (r=0.585, P<0.01), which suggests that the higher the MELD score is, the more likely a transplant candidate on the waiting list had depression, anxiety, sleep disturbance, and daily living disability. No other variable included in the analyses (highest education, marriage status, economic status, age, duration of illness, and time on the waiting list) was correlated with the scores on these scales (Table 3).
Discussion
The present study found that the MELD score was positively correlated with levels of anxiety, depression, sleep disturbance, and ADL disability. OLT candidates on the waiting list with high MELD scores had more severe anxiety, sleep disturbance, and ADL disability than those with low MELD scores.
Pre-OLT depression and anxiety have been shown in several studies [7,30]. Only a few studies have examined the correlation between MELD score and depression and anxiety. Although a few of these studies recorded pre-OLT MELD scores, they did not assess whether a correlation existed and simply reported the mean scores [7,30]. However, a higher MELD score (≥13) after OLT has been shown to be associated with more severe depression; furthermore, depression was correlated with liver function [31]. These results generally coincide with our findings. They differed in that our assessments were conducted before OLT, and we found only a tendency toward higher HAMD-17 score in the high MELD score group rather than a statistical difference (
It is reasonable to believe that disease severity would affect the mood of patients, thus causing depression and anxiety to a corresponding degree with symptoms such as ascites, jaundice, and gastrointestinal hemorrhage. Annema et al. [4] found that the LDSI score, a subjective measurement of disease severity, is related to the trajectories of anxiety and depression. They emphasized the need to adequately manage the symptoms of ESLD, but they noted that further research was required on an objective measurement such as the MELD score. The results of this present study may imply that managing the physiological symptoms in ESLD could also help reduce psychological problems. But the relationship between cognitive appraisal of disease symptoms and the actual severity of the disease should be examined in future research. The core conflict between these 2 theories is the uncertainty of the biological basis of mood disorders. Since the MELD score is calculated by a formula incorporating 3 laboratory variables (international normalized ratio, serum creatinine, and serum bilirubin), our findings might be the starting point for future studies to focus on the relationship between biochemical markers and the severity of mood disorders as a comorbidity in chronic diseases.
Sleep disturbance is closely related to hepatic encephalopathy (HE), one of the clinical manifestations seen in ESLD and reported to affect 32% of patients with liver cirrhosis [9]. Several studies have focused on factors affecting sleep quality in ESLD, but only a few have examined the correlation between MELD score and sleep disturbance. Bruyneel et al. [33] found that sleep quality improved along with a significant decrease in HE severity after medical treatment. In an animal study, Felipo et al. [34] found that HE-model rats awoke more during sleep and took more naps during inactive phases than controls. In contrast, Gencdal et al. [35] found no correlation between MELD score and sleep quality. MELD score has not been found to depict the severity of HE in ESLD, and we were not able to obtain the HE status of all participants in this study. Thus, further research could focus on this particular problem to elucidate the relationship more precisely.
Few studies have examined the association between MELD score and ADL disability. Samoylova et al. [10] found that a higher MELD score was a predictor of new or increasing IADL disability, and they speculated that patients whose MELD scores are <12 have a much lower ADLs/IADLs disability rate since they only recruited patients with a MELD score ≥12. In our study, we proved their hypothesis by finding that a high MELD score group was significantly more disabled than a low MELD score group based on
To our knowledge, the present study was the first to discover the correlation of MELD score with depression, anxiety, sleep disturbance, and ADL disability simultaneously. It also suggested the possibility that the MELD score reflects the severity of candidates’ psychosocial problems, which is a more comprehensive role than the current one of only measuring the physiological severity of disease. The MELD score could accord with the biopsychosocial model of diseases, which would help clinicians consider not only the physiological and medical aspects of ESLD, but also the psychological and social factors.
The results shed light on the expanded clinical usage of MELD score in OLT. Most liver surgeons lack psychiatric expertise, but the MELD score is a value they commonly use in everyday practice. Given their familiarity with MELD scoring, they would be able to identify patients with potential psychological problems and could refer them to psychiatrists for evaluation of the affective status, sleep status, and ADL disability. Moreover, the MELD score could provide a reference for pretransplant and posttransplant intervention because it can also predict post-OLT HRQOL [13,15,16]. However, due to the limited amount of studies and contradictory findings, further research should be done to verify the validity of our findings.
Our study has its limitations. It is a single-center, cross-sectional study with a relatively small sample size. A future study should have a longitudinal design, focus on changes in MELD score over time, and include a larger sample size to test our findings. Future studies could also focus on the association between depression, anxiety, sleep disturbance, and disability to discover whether and how these problems affect each other.
Conclusions
In summary, MELD scores are correlated with anxiety, depression, sleep disturbance, and ADL disability, and a higher MELD score indicates more severe problems. The MELD score could be a more comprehensive indicator in OLT to quickly detect biopsychosocial problems associated with ESLD. Also, it could provide a reference for both medical and psychosocial intervention before and after OLT. Future longitudinal studies could determine the decline of MELD score caused by interventions to treat the psychological problems mentioned in our study.
References
1. Pérez-San-Gregorio MÁ, Martín-Rodríguez A, Domínguez-Cabello E, Quality of life and mental health comparisons among liver transplant recipients and cirrhotic patients with different self-perceptions of health: J Clin Psychol Med Settings, 2013; 20(1); 97-106
2. Fox AN, Brown RS, Is the patient a candidate for liver transplantation?: Clin Liver Dis, 2012; 16; 435-48
3. Yang LS, Shan LL, Saxena A, Morris DL, Liver transplantation: A systematic review of long-term quality of life: Liver Int, 2014; 34; 1298-313
4. Annema C, Roodbol PF, Van den Heuvel ER, Trajectories of anxiety and depression in liver transplant candidates during the waiting-list period: Br J Health Psychol, 2017; 22; 481-501
5. Onghena L, Develtere W, Poppe C, Quality of life after liver transplantation: state of the art: World J Hepatol, 2016; 8; 749-56
6. Rogal SS, Landsittel D, Surman O, Pretransplant depression, antidepressant use, and outcomes of orthotopic liver transplantation: Liver Transpl, 2016; 17; 251-60
7. Teixeira HRS, Marques DM, Lopes ARF, Anxiety and stress levels on liver transplantation candidates: Transplant Proc, 2016; 48; 2333-37
8. Marques DM, Teixeira HR, Lopes AR, Sleep quality assessment and daytime sleepiness of liver transplantation candidates: Transplant Proc, 2016; 48(7); 2356-60
9. Bruyneel M, Sersté T, Sleep disturbances in patients with liver cirrhosis: Prevalence, impact, and management challenges: Nat Sci Sleep, 2018; 10; 369-75
10. Samoylova ML, Covinsky KE, Haftek M, Disability in patients with end-stage liver disease: Results from the functional assessment in liver transplantation study: Liver Transpl, 2017; 23; 292-98
11. Kamath PS, Kim WR, The model for end-stage liver disease (MELD): Hepatology, 2007; 45; 797-805
12. Sacleux S-C, Samuel D, A critical review of MELD as a reliable tool for transplant prioritization: Semin Liver Dis, 2019; 39; 403-13
13. Benzing C, Krezdorn N, Förster J, Health-related quality of life and affective status in liver transplant recipients and patients on the waiting list with low MELD scores: HPB (Oxford), 2016; 18; 449-55
14. Luo X, Leanza J, Massie AB, MELD as a metric for survival benefit of liver transplantation: Am J Transplant, 2018; 18; 1231-37
15. Togashi J, Sugawara Y, Akamatsu N, Quality of life after adult living donor liver transplantation: A longitudinal prospective follow-up study: Hepatol Res, 2013; 43; 1052-63
16. Rodrigue JR, Nelson DR, Reed AI, Is model for end-stage liver disease score associated with quality of life after liver transplantation?: Prog Transplant, 2011; 21; 207-14
17. Hamilton M, Development of a rating scale for primary depressive illness: Br J Soc Clin Psychol, 1967; 6; 278-96
18. Hamilton M, The assessment of anxiety states by rating: Br J Med Psychol, 1959; 32; 50-55
19. Buysse DJ, Reynolds CF, Monk TH, The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research: Psychiatry Res, 1989; 28; 193-213
20. Lawton MP, The functional assessment of elderly people: J Am Geriatr Soc, 1971; 19; 465-81
21. Boessen R, Groenwold RHH, Knol MJ, Comparing HAMD(17) and HAMD subscales on their ability to differentiate active treatment from placebo in randomized controlled trials: J Affect Disord, 2013; 145; 363-69
22. Zimmerman M, Martinez JH, Young D, Severity classification on the Hamilton Depression Rating Scale: J Affect Disord, 2013; 150; 384-88
23. Zhang M: Manual of psychiatric rating scale, 2015, Changsha, Hunan Science and Technology Press
24. Dai Z, Liang S, Yucun S, Application of Hamilton Rating Scale for Depression Scale in geriatric patients: Chinese J Clin Psychol, 1993(1); 22-24
25. Chun W, Yanmin C, Yalin Z, Study on the factorial structure of Hamilton Anxiety Scale: J Clin Psychiatry, 2011; 21(5); 299-301
26. Xianchen L, Maoqin T, Lei H, Reliability and validity of the Pittsburgh sleep quality index: Chinese J Psychiatry, 1996; 29; 103-7
27. Thompson E, Hamilton Rating Scale for Anxiety (HAM-A): Occup Med (Lond), 2015; 65(7); 601
28. Yang M, Hao Q, Luo L, Body mass index and disability in Chinese nonagenarians and centenarians: J Am Med Dir Assoc, 2014; 15; 303.e1-6
29. Kang SH, Jeong WK, Baik SK, Impact of sarcopenia on prognostic value of cirrhosis: Going beyond the hepatic venous pressure gradient and MELD score: J Cachexia Sarcopenia Muscle, 2018; 9(5); 860-70
30. Togashi J, Sugawara Y, Akamatsu N, Quality of life after adult living donor liver transplantation: A longitudinal prospective follow-up study: Hepatol Res, 2013; 43; 1052-63
31. Martins PD, Sankarankutty AK, de Silva OC, Gorayeb R, Psychological distress in patients listed for liver transplantation: Acta Cir Bras, 2006; 21(Suppl 1); 40-43
32. Cron DC, Friedman JF, Winder GS, Depression and frailty in patients with end-stage liver disease referred for transplant evaluation: Am J Transplant, 2016; 16; 1805-11
33. Bruyneel M, Sersté T, Libert W, Improvement of sleep architecture parameters in cirrhotic patients with recurrent hepatic encephalopathy with the use of rifaximin: Eur J Gastroenterol Hepatol, 2017; 29; 302-8
34. Felipo V, Piedrafita B, Barios JA, Rats with minimal hepatic encephalopathy show reduced cGMP-dependent protein kinase activity in hypothalamus correlating with circadian rhythms alterations: Chronobiol Int, 2015; 32; 966-79
35. Gencdal G, Gunsar F, Meral CE, Sleep disorders in cirrhotics: How can we detect?: Liver Int, 2014; 34; 1192-97
Tables
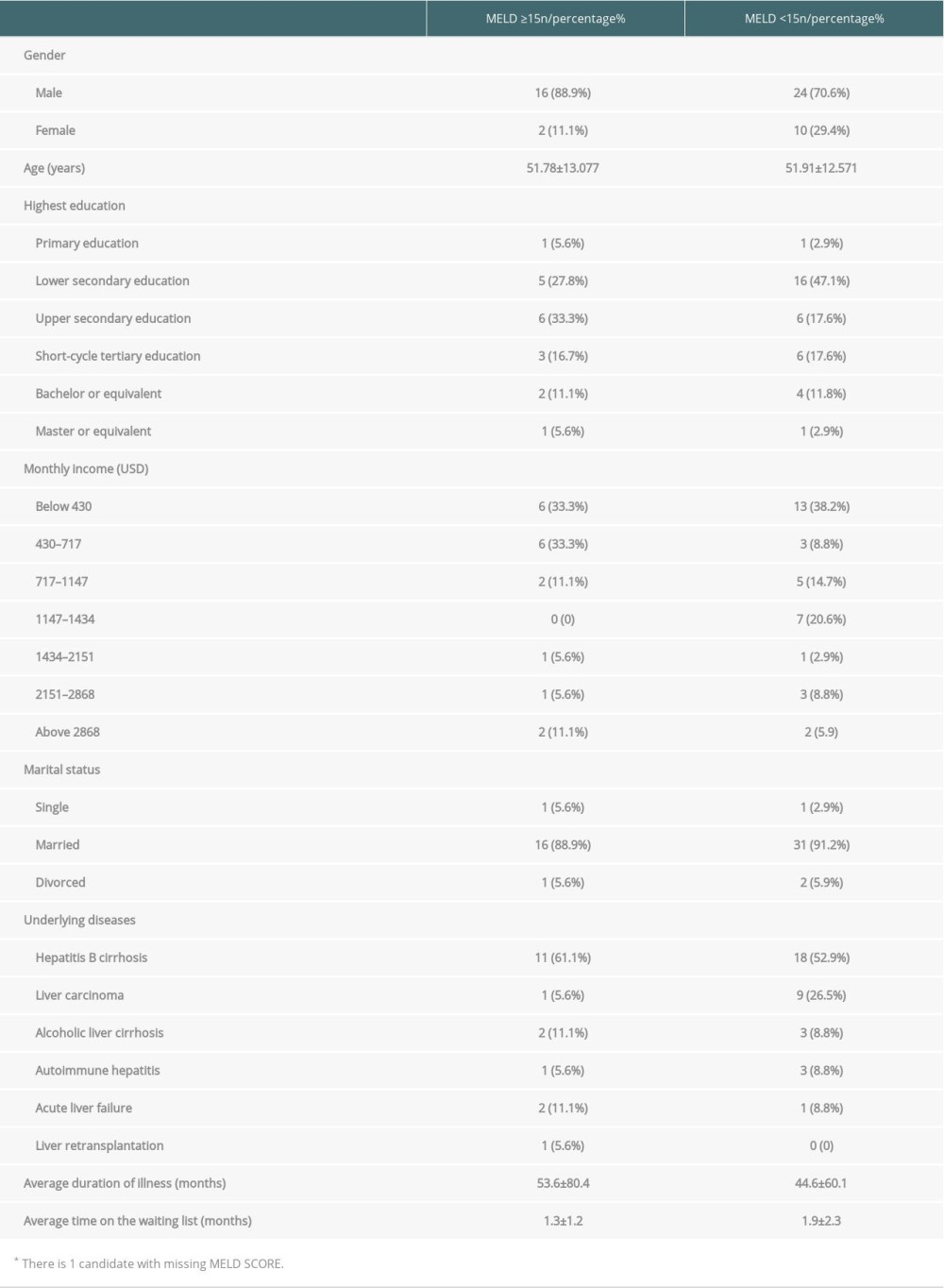 Table 1. Demographic information on liver candidates divided by MELD score.
Table 1. Demographic information on liver candidates divided by MELD score.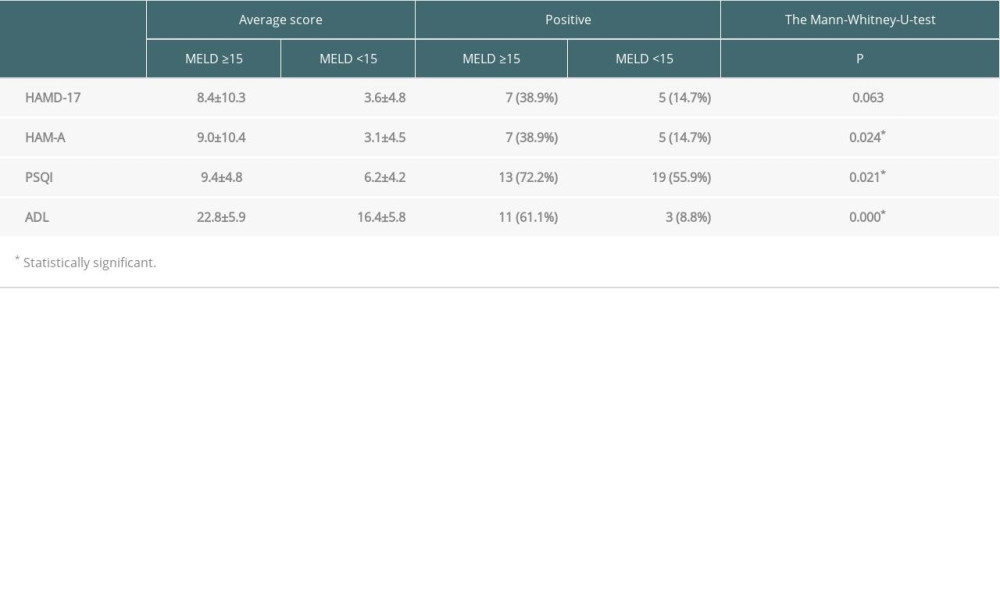 Table 2. Results of HAMD-17, HAM-A, PSQI and ADL based on different MELD score groups.
Table 2. Results of HAMD-17, HAM-A, PSQI and ADL based on different MELD score groups.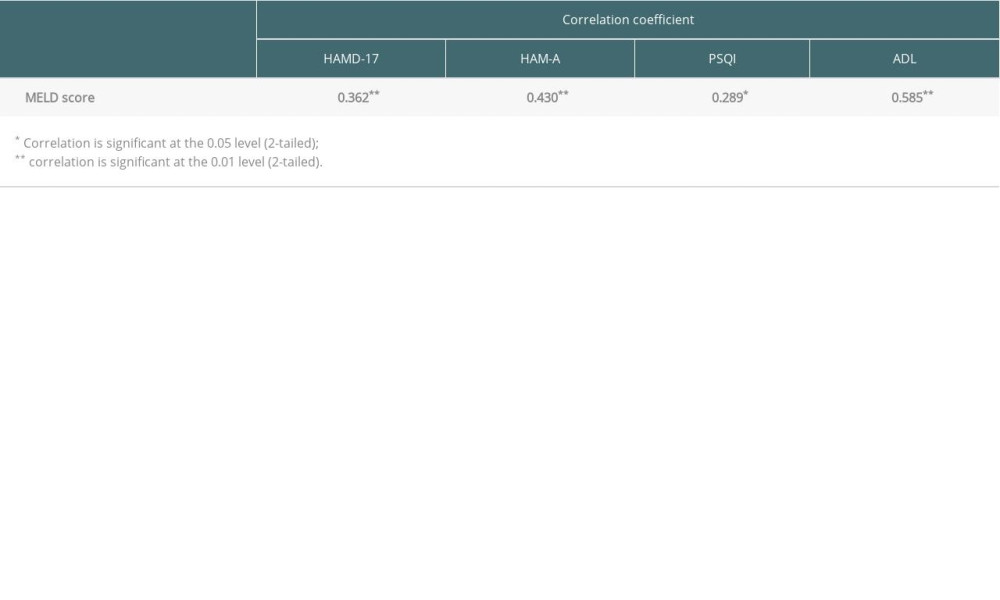 Table 3. Result of the Spearman test for correlation.
Table 3. Result of the Spearman test for correlation.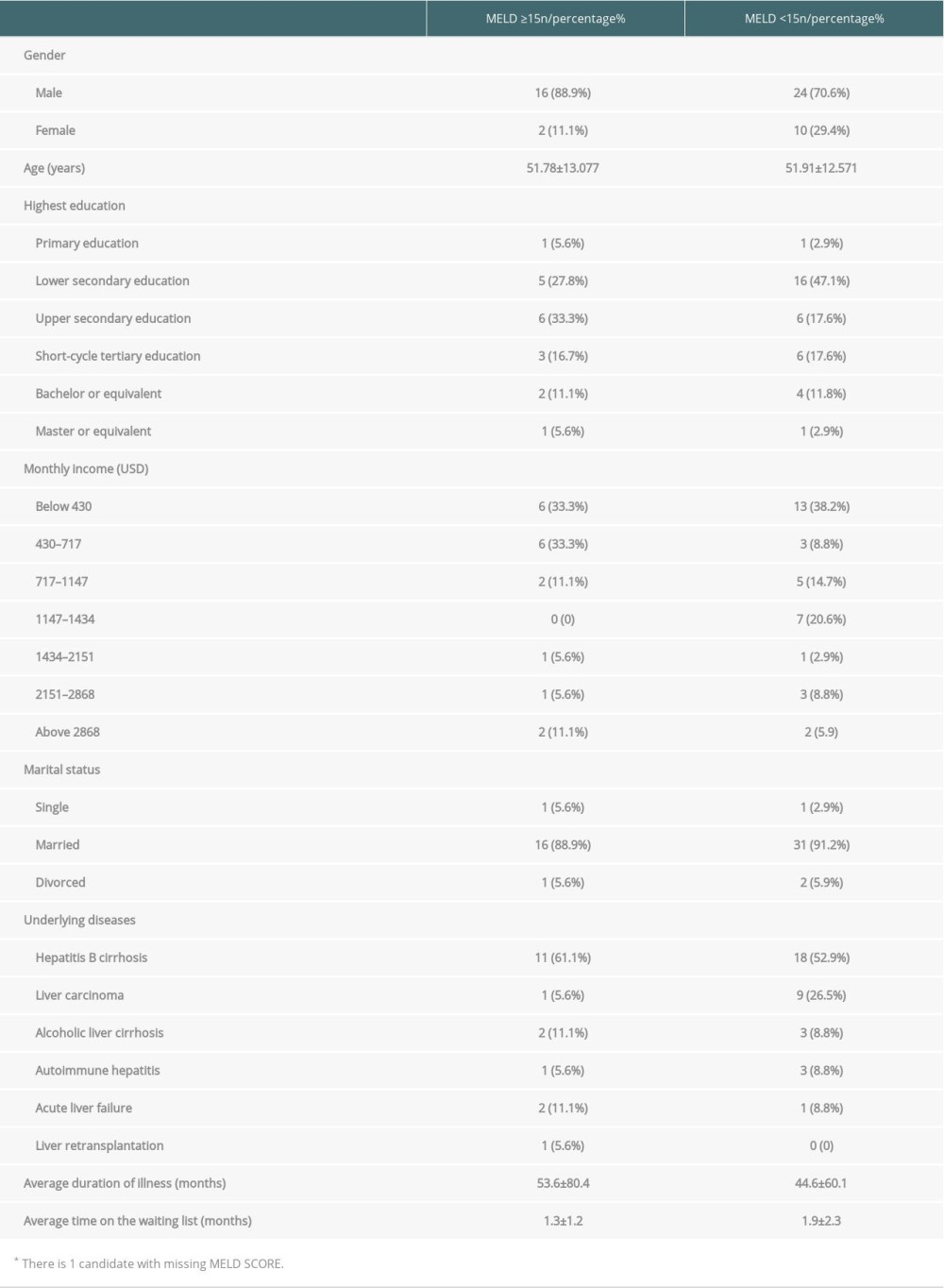 Table 1. Demographic information on liver candidates divided by MELD score.
Table 1. Demographic information on liver candidates divided by MELD score.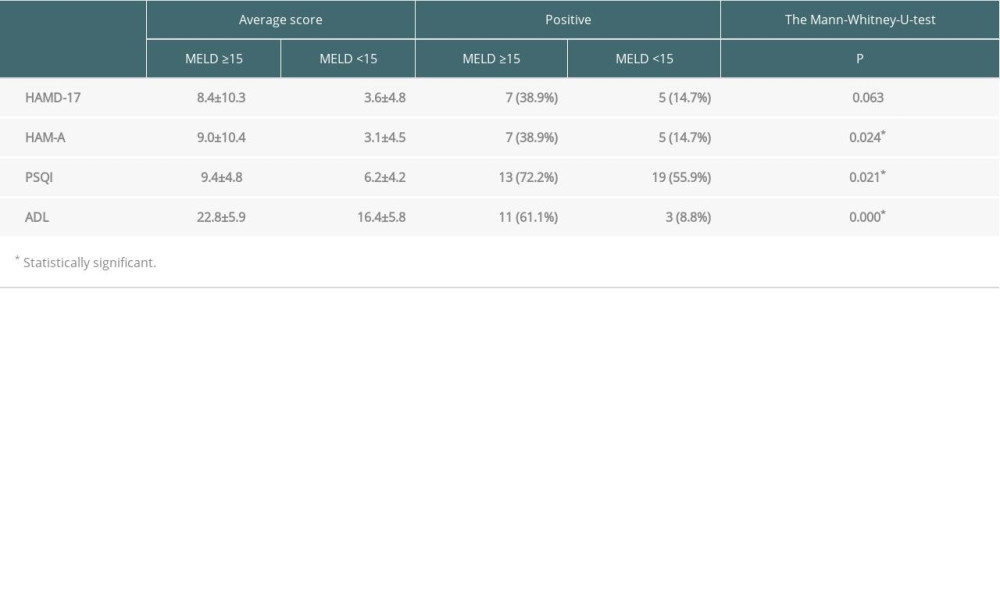 Table 2. Results of HAMD-17, HAM-A, PSQI and ADL based on different MELD score groups.
Table 2. Results of HAMD-17, HAM-A, PSQI and ADL based on different MELD score groups.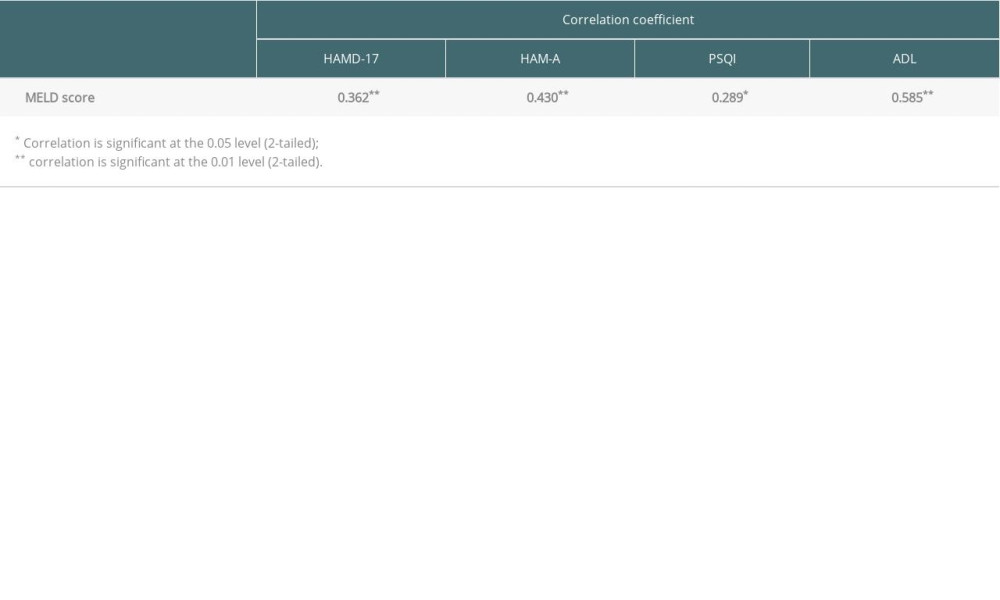 Table 3. Result of the Spearman test for correlation.
Table 3. Result of the Spearman test for correlation. In Press
18 Mar 2024 : Original article
Does Antibiotic Use Increase the Risk of Post-Transplantation Diabetes Mellitus? A Retrospective Study of R...Ann Transplant In Press; DOI: 10.12659/AOT.943282
20 Mar 2024 : Original article
Transplant Nephrectomy: A Comparative Study of Timing and Techniques in a Single InstitutionAnn Transplant In Press; DOI: 10.12659/AOT.942252
28 Mar 2024 : Original article
Association Between FEV₁ Decline Rate and Mortality in Long-Term Follow-Up of a 21-Patient Pilot Clinical T...Ann Transplant In Press; DOI: 10.12659/AOT.942823
02 Apr 2024 : Original article
Liver Transplantation from Brain-Dead Donors with Hepatitis B or C in South Korea: A 2014-2020 Korean Organ...Ann Transplant In Press; DOI: 10.12659/AOT.943588
Most Viewed Current Articles
05 Apr 2022 : Original article
Impact of Statins on Hepatocellular Carcinoma Recurrence After Living-Donor Liver TransplantationDOI :10.12659/AOT.935604
Ann Transplant 2022; 27:e935604
12 Jan 2022 : Original article
Risk Factors for Developing BK Virus-Associated Nephropathy: A Single-Center Retrospective Cohort Study of ...DOI :10.12659/AOT.934738
Ann Transplant 2022; 27:e934738
22 Nov 2022 : Original article
Long-Term Effects of Everolimus-Facilitated Tacrolimus Reduction in Living-Donor Liver Transplant Recipient...DOI :10.12659/AOT.937988
Ann Transplant 2022; 27:e937988
15 Mar 2022 : Case report
Combined Liver, Pancreas-Duodenum, and Kidney Transplantation for Patients with Hepatitis B Cirrhosis, Urem...DOI :10.12659/AOT.935860
Ann Transplant 2022; 27:e935860