10 October 2023: Original Paper
Prolonged Tracheal Intubation in the ICU as a Possible Risk Factor for Arytenoid Dislocation After Liver Transplant Surgery: A Retrospective Case-Control Study
Wenqing Yan12BDEF, Weihua DongDOI: 10.12659/AOT.940727
Ann Transplant 2023; 28:e940727
Abstract
BACKGROUND: Arytenoid dislocation (AD) is a rare complication of general anesthesia with tracheal intubation, with a published incidence of 0.009-0.097%. This retrospective case-control study aimed to identify risk factors associated with AD in patients who underwent liver transplantation.
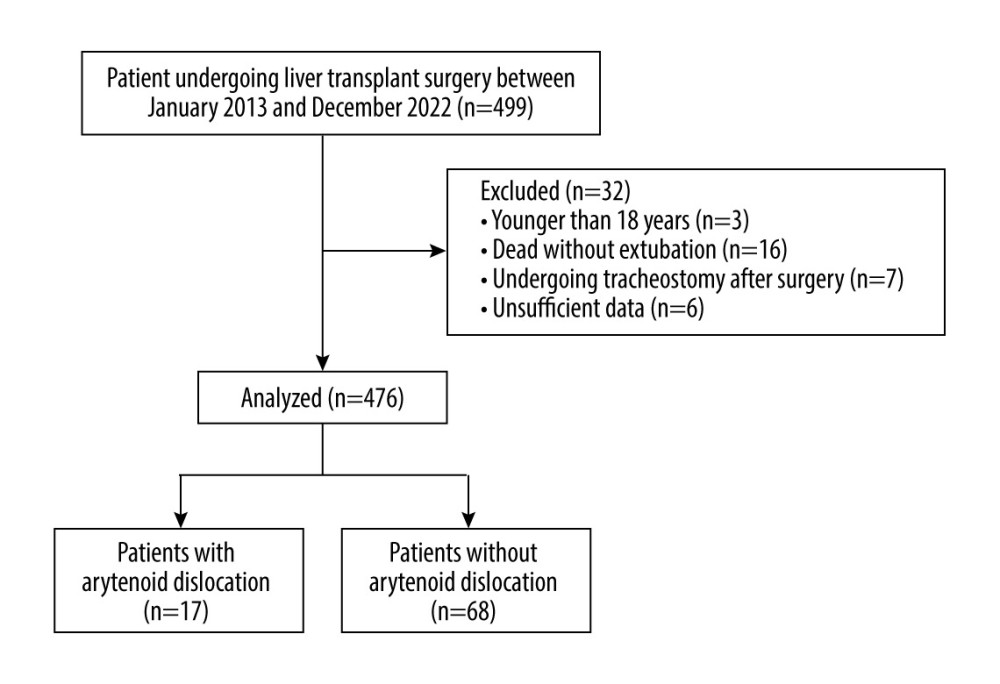
MATERIAL AND METHODS: This study included 476 patients who underwent liver transplantation between January 2013 and December 2022. Patients with AD who underwent surgery were included in the AD group. For each case of AD, 4 patients matched by anesthesia type and anesthetist were randomly selected as the non-AD group. Data on patient characteristics, anesthetic factors, and surgical factors were collected and compared between patients with and without AD. Logistic regression analysis was performed to determine the risk factors for AD after liver transplantation.
RESULTS: Of the 476 patients who underwent liver transplantation, 17 (3.57%) had AD. AD occurred on the left side in 13 patients and on the right side in 4 patients. The 17 patients who experienced AD and 68 matched non-AD patients were enrolled. Patients in the AD group had a greater intubation depth (24 [23-24] vs 24 [24-24], P=0.043), a higher level of hemoglobin (134.5 [118-147.5] vs 112 [96.25-125], P=0.014), and prolonged tracheal intubation in the ICU (19.75 [15.87-31.87] vs 13 [10.62-15], P<0.001) compared to those in the non-dislocation group. Multivariate logistic regression analysis showed that prolonged tracheal intubation in the ICU was independently associated with the occurrence of AD in patients who underwent liver transplantation (P=0.013).
CONCLUSIONS: This study showed that the incidence of AD was 3.57% in patients undergoing liver transplant surgery and that prolonged tracheal intubation in the ICU was a possible risk factor for AD.
Keywords: Liver Transplantation, Risk Factors, Intubation, Intratracheal, Arytenoid Cartilage, Humans, Retrospective Studies, Case-Control Studies, Joint Dislocations, Intensive Care Units
Background
Arytenoid dislocation (AD) is a rare complication of general anesthesia with tracheal intubation, with a published incidence of 0.009–0.097% [1–3]. However, its pathogenesis remains unclear. Gallet et al recently suggested that the occurrence of AD might be due to cricoarytenoid joint (CAJ) instability rather than the forces exerted on the articulation [4]. Therefore, it is important to investigate the risk factors for CAJ instability. Although several prospective studies [1–3,5–9] of AD identified some risk factors, such as anemia, a low body mass index (BMI), intubation difficulty, and prolonged operation time, other potential factors are unclear. Notably, we have an impression that patients undergoing liver transplantation tend to be associated with this complication. Nonetheless, there have been no published case reports of AD complicating liver transplant surgery and no reports of risk factors in patients undergoing liver transplantation. Therefore, this retrospective case-control study aimed to identify risk factors associated with AD in patients who underwent liver transplantation.
Material and Methods
PATIENT SELECTION:
We retrospectively enrolled all patients who underwent liver transplantation under general anesthesia with tracheal intubation at Jiang Xi Provincial People’s Hospital in China between January 2014 and December 2022. Patients aged <18 years were excluded. Patients were also excluded if intubation was performed before surgery, if they died or underwent tracheostomy before extubation, or if their medical data needed for this study were missing. Patients with AD who underwent surgery were included in the AD group. For each case of AD, 4 patients matched by anesthesia type and anesthetist were randomly selected as the non-AD group.
DATA SELECTION:
For each incident, we extracted patient data including age, sex, body weight, height, BMI, American Society of Anesthesiologists physical status classification, limited mouth opening, smoking and alcohol history, Mallampati score, number of intubation attempts, endotracheal tube diameter, intubation depth, timing of surgery (day or night), duration of surgery, intraoperative blood loss, duration of mechanical ventilation in the ICU, and stomach tube indwelling time. Preoperative baseline laboratory data, including routine blood analysis and liver, kidney, and coagulation functions, were also recorded.
Limited mouth opening was defined as a restriction of less than 2 finger breadths. We divided the day into 2 epochs consistent with the time when the anaesthesiologist shifts started at 8: 00 (daytime) and 17: 30 (nighttime).
AD should be considered in patients with persistent hoarseness after general anesthesia. For all included patients with AD, its occurrence was confirmed by an experienced otolaryngologist using a combination of fiber-optic laryngoscopy and neck computed tomography.
For AD patients, we further analyzed the incidence of left and right AD and the outcomes of surgical repair versus conservative treatment.
STATISTICAL ANALYSIS:
This case-control study compared the parameters of the AD group and non-AD group. Descriptive data are expressed as mean±standard deviation or median (interquartile range) for normally and non-normally distributed data, and were compared using the unpaired
Results
Of the 499 patients initially enrolled during the study period, 32 were excluded because they were younger than 18 years (n=3), died without extubation (n=16), underwent tracheostomy after surgery (n=7), or had insufficient data (n=6) (Figure 1). Among the 476 patients who underwent general anesthesia between 2013 and 2022, 17 (3.57%) were diagnosed with AD. The 17 patients who experienced AD and 68 matched non-AD patients were enrolled. The demographic and surgery-related characteristics are compared between the AD and non-AD groups in Table 1. There were 13 men and 4 women with a mean age of 48±6.36 (range, 38–59) years. AD occurred on the left side in 13 patients and on the right side in 4 patients. All patients with AD recovered or improved after the reduction.
The baseline demographic and surgery-related characteristics were comparable between the AD and non-AD groups. Hemoglobin levels were significantly higher level in the AD than non-AD group (134.5 [118–147.5] vs 112 [96.25–125],
Table 2 shows the anesthesia- and ICU-related characteristics. Patients in the AD group had a greater intubation depth (24 [23–24] vs 24 [24–24],
These 3 factors were subjected to multivariate logistic regression analysis. Table 3 shows the results of multivariate logistic regression analysis to determine the potential risk factors for AD. The multivariate logistic regression analysis showed that prolonged tracheal intubation in the ICU was independently associated with the occurrence of AD in patients who underwent liver transplantation (
Discussion
In our study, the incidence of postoperative AD was 3.57% in patients undergoing liver transplant surgery. Liver transplant patients with prolonged tracheal intubation in the ICU were at increased risk of postoperative AD.
The incidence of AD in our cohort was higher than that reported in previous studies (0.01–0.1%) [1,5,10,11]. AD is classically defined as complete separation of the arytenoid cartilage from the CAJ [1]. However, the underlying pathogenesis mechanism of AD remains unclear. Previous reports suggested that the high forces acting on CAJ by laryngoscope or intubation tube are responsible for AD. However, a cadaveric study by Friedman et al [12] attempted to assess the likelihood of AD during intubation through the application of controlled force. AD did not occur, even when the testing approximated the maximum force achievable under extreme conditions. Endotracheal tube insertion thus seems unlikely to cause AD. Recently, Gallet et al [4] suggested that AD is linked to congenital or acquired CAJ instability, thus facilitating AD after even minor trauma. Therefore, it is necessary to assess the risk factors for CAJ instability. A retrospective study by Jang et al [4], including patients who underwent operation under general anesthesia with endotracheal intubation, aimed to identify the patient, anesthetic, and operative factors associated with AD. This study showed that head-neck positioning during surgery, less anesthetist experience, and female sex were significantly associated with AD. A study by Tsuru et al [7] demonstrated that major cardiovascular surgery was one of the significant risk factors for AD. Tan et al [13] reported that use of a large-bore orogastric tube can increase the potential for AD after prolonged tracheal intubation. Moreover, anemia, laryngomalacia, acromegaly, chronic steroid use, and low BMI were also considered to be important risk factors for AD. Previous studies excluded patients undergoing emergent surgery [2,5–7,13]. Patients admitted to the Intensive Care Unit (ICU) after surgery were also excluded [5,13]. However, patients undergoing urgent surgery and patients admitted to the ICU after surgery were included in our study. In our study, we found that liver transplant patients with prolonged tracheal intubation in the ICU were at increased risk of postoperative AD. A tracheal tube can exert pressure in the region of the arytenoid cartilage when the tracheal tube is left in situ [13,14]. Early extubation after liver transplantation is impossible, and patients remain endotracheally intubated and sedated for mechanical ventilation. Prolonged tracheal intubation implied that CAJ would receive prolonged pressure. CAJ instability may be caused by prolonged pressure by the tracheal tube. In addition, nasogastric tubes were used in intubated patients in the ICU, and CAJ injury may be possible when the CAJ becomes pinched between the tracheal tube and the nasogastric tubes [13].
The goal of sedation for mechanically ventilated patients in the ICU is to ensure patient comfort and safety while facilitating patient–ventilator interactions [15–18]. Inappropriate sedation can cause patients to experience unnecessarily prolonged tracheal intubation [16,19], and it may fail to ensure adequate pain control. If irritability and even delirium persists, the tracheal tube may exert larger pressure on the CAJ [16,17]. Therefore, many challenges remain in sedation management for most postoperative patients.
Patients admitted to the ICU after surgery were not the only liver transplantation patients. Why did patients undergoing liver transplantation tend to have AD in our hospital? The following points may be relevant. First, liver transplantation is a safe treatment for selected patients with end-stage liver disease, primary liver cancer, and fulminant hepatic failure [18]. Almost all patients presented with anemia, splenomegaly, and jaundice. Several previous studies indicated that anemia is a risk factor for AD [9]. Although our univariate analysis showed hemoglobin levels were significantly higher level in the AD patients, this could have been influenced by unmeasured confounders and the small sample size. Furthermore, we believe that AD was rarely missed among liver transplant patients as they are always under close surveillance in the ICU.
Our findings may be applicable to all patients transferred to the surgical ICU without extubation. For such patients, prolonged tracheal intubation in the ICU may increase the incidence of AD. Appropriate analgesia and sedation are critical aspects in the management of patients receiving mechanical ventilation in the ICU. Therefore, we must reasonably assess these patients and remove the tubes as soon as possible.
This study has some limitations. First, the retrospective nature of the study and the small sample size of the AD group may have led to bias and may have caused our results to be unstable. Second, in this retrospective study, we could only obtain limited information recorded in the medical charts. Third, we did not perform receiver operating characteristic (ROC) curve analysis to identify the cut-off value of tracheal intubation time for predicting the occurrence of AD. The sample size was small, which may have affected the accuracy of the results of ROC curve analysis. Fourth, we did not compare patients after liver transplantation with other surgical patients to explore the risk factors for AD. The incidence of AD is low, and it is difficult to obtain a sufficient sample size of patients undergoing liver transplantation or other surgery. Fifth, the occurrence of AD may be mistaken for postoperative hoarseness or laryngeal nerve paralysis owing to atypical clinical presentations. The symptoms of some patients with AD improve without treatment and the condition may remain undetected by clinicians. Therefore, the incidence may have been underestimated. Finally, this was a single-center study; thus, the generalisability of its findings may be limited.
Conclusions
This study showed that the incidence of AD was 3.57% in patients undergoing liver transplant surgery and that prolonged tracheal intubation in the ICU was a possible risk factor for AD.
References
1. Frosolini A, Marioni G, Maiolino L, Current management of arytenoid sub-luxation and dislocation: Eur Arch Otorhinolaryngol, 2020; 277(11); 2977-86
2. Wu L, Shen L, Zhang Y, Association between the use of a stylet in endotracheal intubation and postoperative arytenoid dislocation: A case-control study: BMC Anesthesiol, 2018; 18(1); 59
3. Szigeti CL, Baeuerle JJ, Mongan PD, Arytenoid dislocation with lighted stylet intubation: Case report and retrospective review: Anesth Analg, 1994; 78(1); 185-86
4. Gallet P, Nguyen DT, Toussaint B, Spontaneous arytenoid dislocation and crico-arytenoid instability: Eur Ann Otorhinolaryngol Head Neck Dis, 2019; 136(4); 307-8
5. Jang EA, Yoo KY, Lee S, Head-neck movement may predispose to the development of arytenoid dislocation in the intubated patient: A 5-year retrospective single-center study: BMC Anesthesiol, 2021; 21(1); 198
6. Lou Z, Yu X, Li Y, BMI may be the risk factor for arytenoid dislocation caused by endotracheal intubation: A retrospective case-control Study: J Voice, 2018; 32(2); 221-25
7. Tsuru S, Wakimoto M, Iritakenishi T, Cardiovascular operation: A significant risk factor of arytenoid cartilage dislocation/subluxation after anesthesia: Ann Card Anaesth, 2017; 20(3); 309-12
8. Lee DH, Yoon TM, Lee JK, Clinical characteristics of arytenoid dislocation after endotracheal intubation: J Craniofac Surg, 2015; 26(4); 1358-60
9. Shen L, Wang WT, Yu XR, Evaluation of risk factors for arytenoid dislocation after endotracheal intubation: A retrospective case-control study: Chin Med Sci J, 2014; 29(4); 221-24
10. Yamanaka H, Hayashi Y, Watanabe Y, Prolonged hoarseness and arytenoid cartilage dislocation after tracheal intubation: Br J Anaesth, 2009; 103(3); 452-55
11. Rubin AD, Hawkshaw MJ, Moyer CA, Arytenoid cartilage dislocation: A 20-year experience: J Voice, 2005; 19(4); 687-701
12. Friedman AD, Kobler JB, Landau-Zemer T, High-force simulated intubation fails to dislocate cricoarytenoid joint in ex vivo human larynges: Ann Otol Rhinol Laryngol, 2012; 121(11); 746-53
13. Tan PH, Hung KC, Hsieh SW, Large-bore calibrating orogastric tube and arytenoid dislocation: A retrospective study: Br J Anaesth, 2016; 116(2); 296-98
14. Weymuller EA, Bishop MJ, Fink BR, Quantification of intralaryngeal pressure exerted by endotracheal tubes: Ann Otol Rhinol Laryngol, 1983; 92(5 Pt 1); 444-47
15. Devlin JW, Skrobik Y, Gelinas C, Executive summary: Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU: Crit Care Med, 2018; 46(9); 1532-48
16. Devlin JW, Skrobik Y, Gelinas C, Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU: Crit Care Med, 2018; 46(9); e825-e73
17. Vincent JL, Shehabi Y, Walsh TS, Comfort and patient-centred care without excessive sedation: the eCASH concept: Intensive Care Med, 2016; 42(6); 962-71
18. European Association for the Study of the Liver, EASL clinical practice guidelines: Liver transplantation: J Hepatol, 2016; 64(2); 433-85
19. Lang J, Appraisal of clinical practice guideline: Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU: J Physiother, 2022; 68(4); 282
Tables
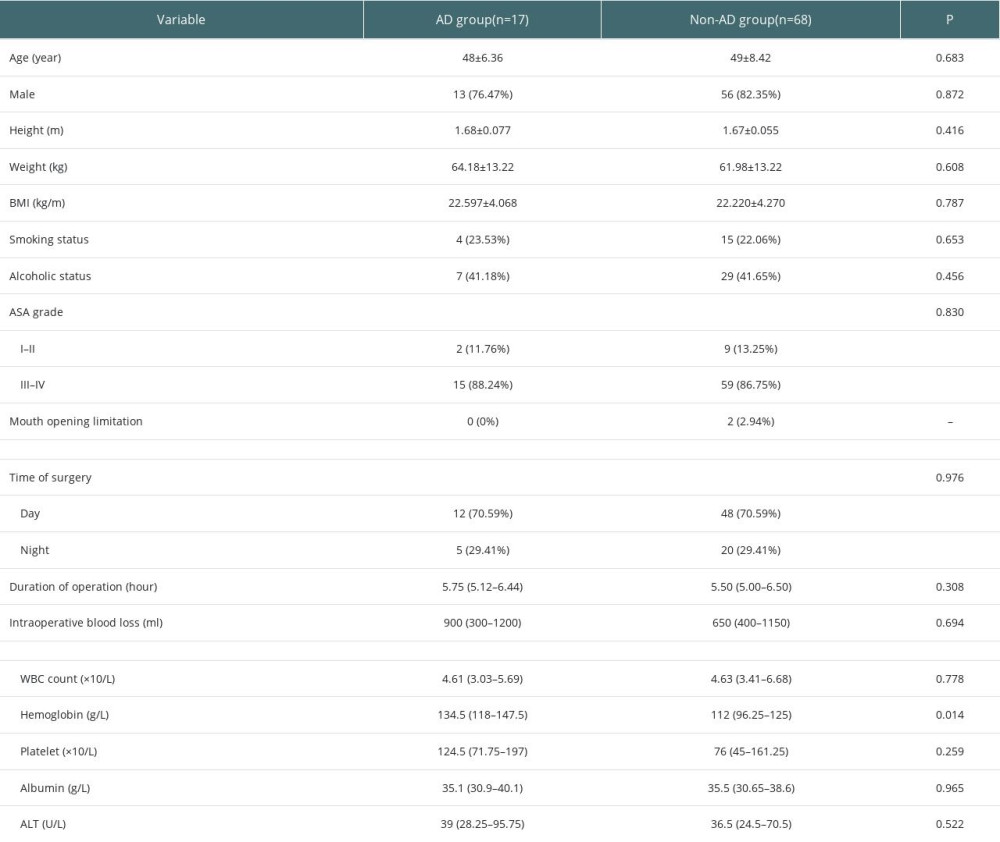 Table 1. Demographic characteristics and surgery-related characteristics.
Table 1. Demographic characteristics and surgery-related characteristics.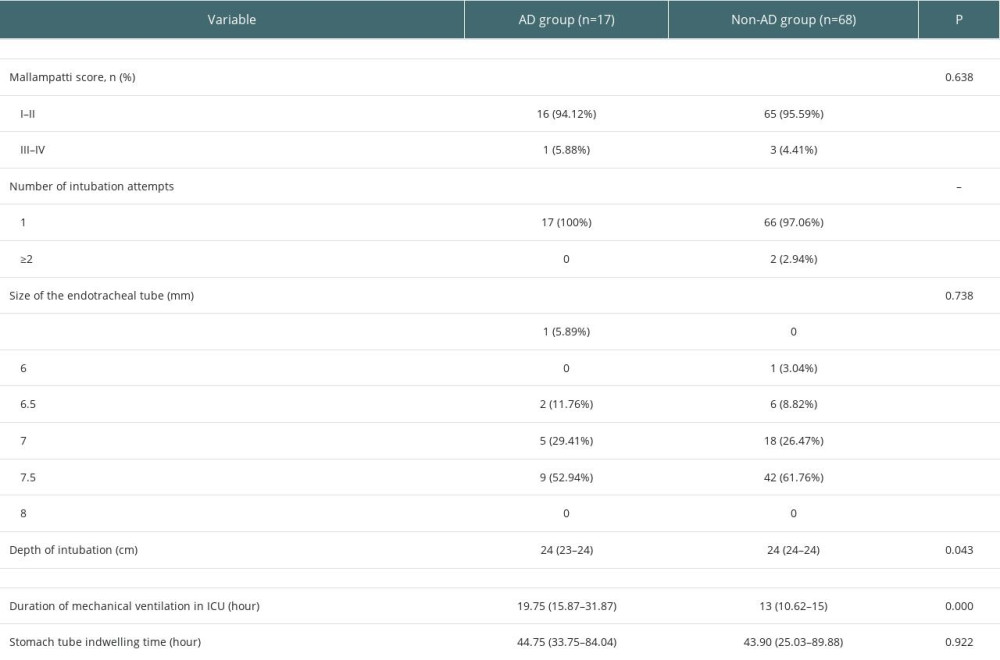 Table 2. Anesthesia-related and ICU-related characteristics.
Table 2. Anesthesia-related and ICU-related characteristics.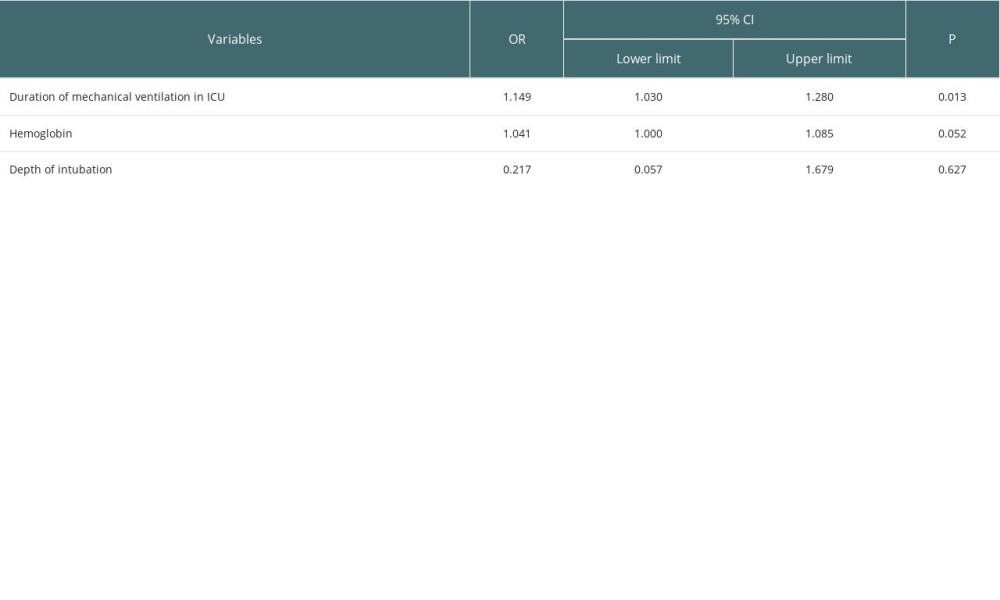 Table 3. Multivariate analysis of risk factors associated with AD.
Table 3. Multivariate analysis of risk factors associated with AD.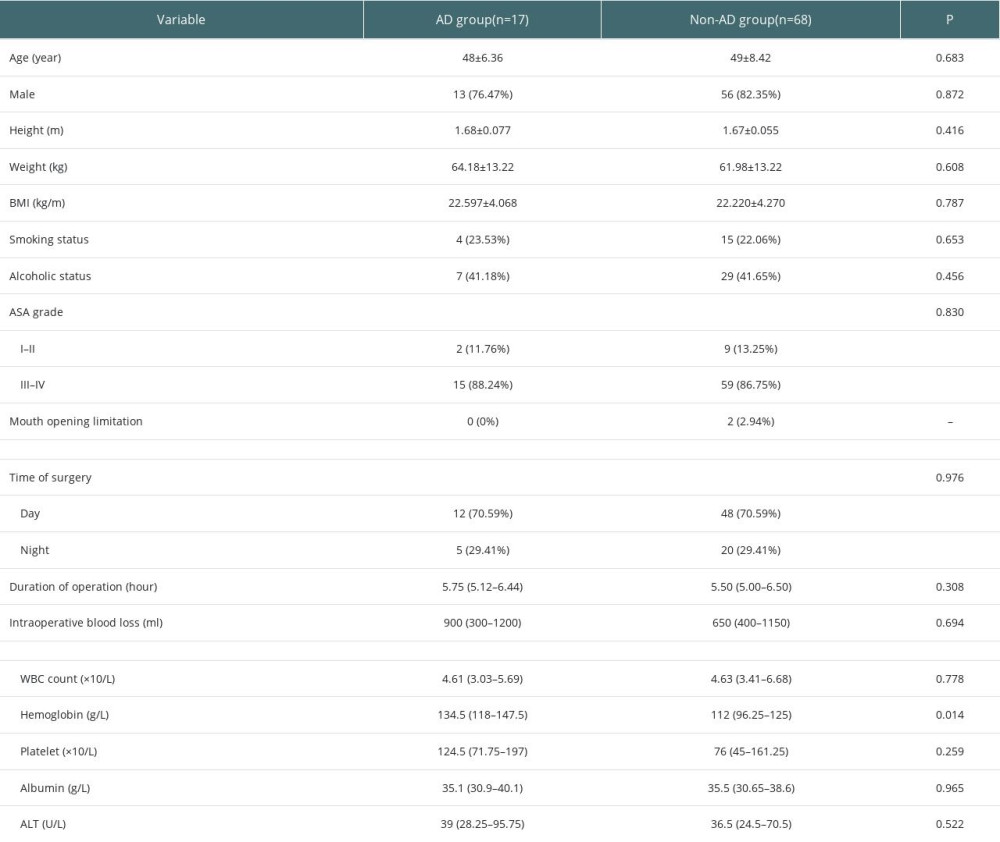 Table 1. Demographic characteristics and surgery-related characteristics.
Table 1. Demographic characteristics and surgery-related characteristics.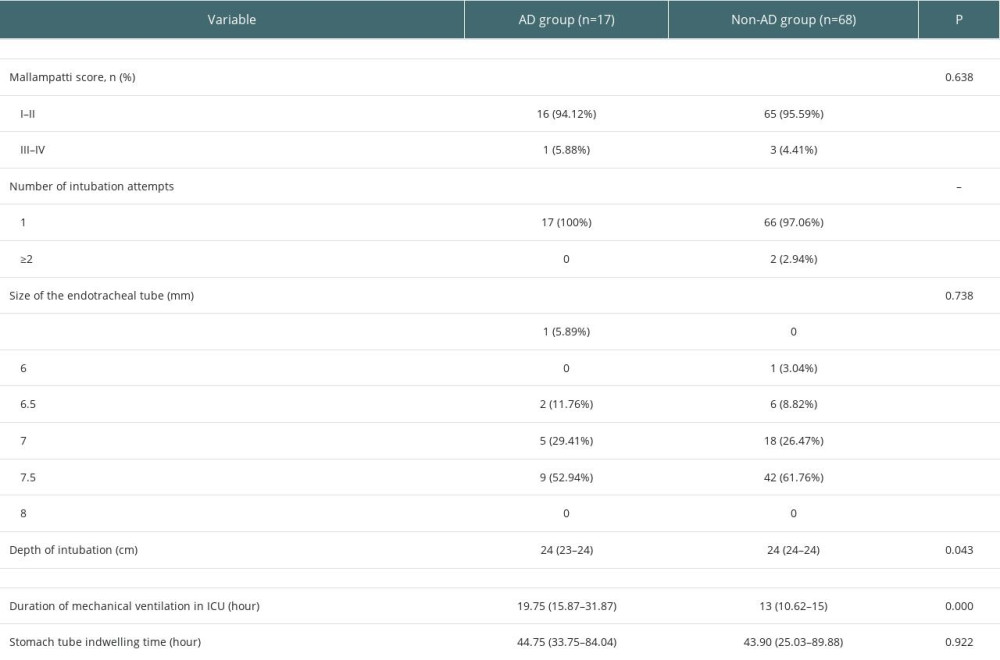 Table 2. Anesthesia-related and ICU-related characteristics.
Table 2. Anesthesia-related and ICU-related characteristics.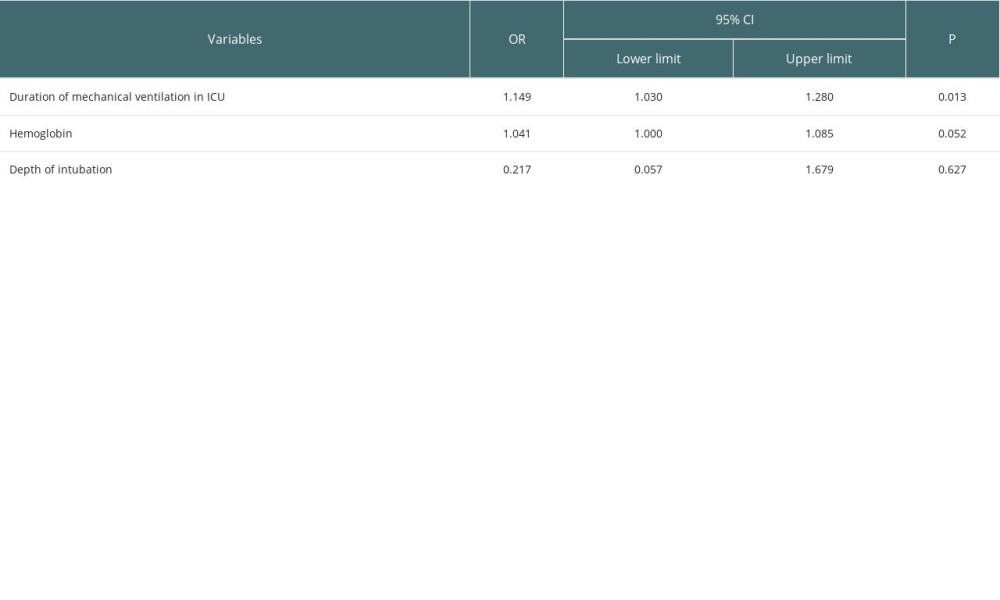 Table 3. Multivariate analysis of risk factors associated with AD.
Table 3. Multivariate analysis of risk factors associated with AD. In Press
20 Mar 2024 : Original article
Transplant Nephrectomy: A Comparative Study of Timing and Techniques in a Single InstitutionAnn Transplant In Press; DOI: 10.12659/AOT.942252
28 Mar 2024 : Original article
Association Between FEV₁ Decline Rate and Mortality in Long-Term Follow-Up of a 21-Patient Pilot Clinical T...Ann Transplant In Press; DOI: 10.12659/AOT.942823
02 Apr 2024 : Original article
Liver Transplantation from Brain-Dead Donors with Hepatitis B or C in South Korea: A 2014-2020 Korean Organ...Ann Transplant In Press; DOI: 10.12659/AOT.943588
02 Apr 2024 : Original article
Effect of Dexmedetomidine Combined with Remifentanil on Emergence Agitation During Awakening from Sevoflura...Ann Transplant In Press; DOI: 10.12659/AOT.943281
Most Viewed Current Articles
05 Apr 2022 : Original article
Impact of Statins on Hepatocellular Carcinoma Recurrence After Living-Donor Liver TransplantationDOI :10.12659/AOT.935604
Ann Transplant 2022; 27:e935604
12 Jan 2022 : Original article
Risk Factors for Developing BK Virus-Associated Nephropathy: A Single-Center Retrospective Cohort Study of ...DOI :10.12659/AOT.934738
Ann Transplant 2022; 27:e934738
22 Nov 2022 : Original article
Long-Term Effects of Everolimus-Facilitated Tacrolimus Reduction in Living-Donor Liver Transplant Recipient...DOI :10.12659/AOT.937988
Ann Transplant 2022; 27:e937988
15 Mar 2022 : Case report
Combined Liver, Pancreas-Duodenum, and Kidney Transplantation for Patients with Hepatitis B Cirrhosis, Urem...DOI :10.12659/AOT.935860
Ann Transplant 2022; 27:e935860