29 December 2023: Original Paper
Increased Platelet Aggregation in Adults After Orthotopic Liver Transplantation Indicates Higher Probability of Early Postoperative Survival
Run Yang1ACEF, Chen Shang1ACEF, Zhifeng Xi2BD, Ya Yang3C, Yuxiao DengDOI: 10.12659/AOT.941583
Ann Transplant 2023; 28:e941583
Abstract
BACKGROUND: Studies have shown that increased platelet aggregation in patients with decompensated cirrhosis indicates higher risk of further decompensation and death, but studies on the association between platelet aggregation function and early postoperative survival in orthotopic liver transplantation (OLT) patients are rare. We conducted a retrospective study to investigate whole-blood platelet aggregation during the perioperative period of OLT patients and its association with clinical outcomes.
MATERIAL AND METHODS: Adult patients who underwent OLT between January 1 and April 30, 2021 were retrospectively reviewed. Laboratory test results indicating primary hemostasis were analyzed. The generalized linear model was used to investigate the association between primary hemostasis parameters and survival.
RESULTS: A total of 256 patients were enrolled. The median platelet count (PLT) was 61.5 (39.5-106.3)×109/L before transplantation. The median MA value was 43.1 (34.5-56.2) mm. From the 1st to the 3rd day after transplantation, PLT and MA both indicated a significant decrease. Two weeks after transplantation, PLT rose to 143.0 (85.0-209.0)×10⁹/L, and the MA value rose to 56.7 (52.2-62.7) mm. On multivariate analysis, PLT at 1 week after transplantation (OR: 1.07; P=0.006) and MA value (OR: 1.12; P=0.003) were independently associated with outcome. The AUROC of the model combined with MA value, MELD score, and age was 0.945 (95% CI: 0.911-0.978).
CONCLUSIONS: The change in primary hemostasis during the early postoperative period of adult OLT is mainly characterized by the increase of platelet count and function 14 days after transplantation. Higher PLT was associated with higher survival at 14 days after transplantation, while a higher PLT ratio was associated with survival at 3 months after transplantation. Based on comprehensive consideration, the model combined with MA value, MELD score, and age more reliably indicated the associated with early survival after transplantation.
Keywords: Hemostasis, Platelet Aggregation, Liver Transplantation, Thrombelastography
Background
Adult orthotopic liver transplantation (OLT) is an important method for treating various severe acute or advanced chronic liver diseases [1]. Following the development of surgical techniques, anaesthesiological approaches and surgical technique, along with improvements in immunosuppressive regimens, the mortality after liver transplantation (LT) associated with surgical factors has decreased and one-year survival rates were nearly 80–90% for transplant recipients [2]. More attention has been paid to the perioperative management of LT [3].
Studies have shown that the perioperative period of LT is associated with substantial alterations to the patient’s coagulation status [4] and these patients are prone to abnormal blood coagulation during the postoperative period [5]. At present, the hemostasis process is divided into three parts: primary hemostasis, coagulation factors and fibrinolysis [6]. Among the above parts, primary hemostasis mainly depends on number of platelet and platelet aggregation function. Aggregometry might allow for a more comprehensive evaluation of primary hemostasis than platelet count alone by measuring platelet aggregation, the process by which platelets adhere to each other at the site of vessel injury [7–9].
Thromboelastography (TEG) has been used perioperatively during LT to provide a real-time global hemostasis assessment for targeted blood product replacement [10, 11]. Researchers found that maximum amplitude (MA) value, which represents clot strength that decreases with hypocoagulable states or consumption of platelets [12], from the first postoperative TEG was associated with early allograft dysfunction (EAD) [13]. Another study found that variceal bleeding within 6 weeks prior to liver transplantation was associated with longer R-times, longer K-times, smaller α-angle, and lower MA values [14].
Studies have shown that the increase of platelet aggregation function indicates higher risk of further decompensation and death in patients with decompensated cirrhosis [15]. However, the changes of platelet aggregation function and TEG during the perioperative period, especially after OLT, and its relationship with the early postoperative survival of patients, are still unclear. Understanding whether prognosis of OLT is associated with alterations of platelet aggregation would improve the hemostatic management in these patients.
Thus, we aimed to investigate whole-blood platelet aggregation during the perioperative period of OLT patients and its association with clinical outcomes.
Material and Methods
DATA COLLECTION:
In this single-center, retrospective study, data were collected from Ren Ji Hospital, Shanghai Jiao Tong University School of Medicine. The post-transplantation observational period ended on 30 July 2021. Laboratory tests data were collected on the day of admission, and on days 1, 3, 7, and 14 after transplantation. Follow-up was conducted three months after OLT via both electronic medical record system and phone call.
INCLUSION AND EXCLUSION CRITERIA:
All patients who underwent OLT at Ren Ji Hospital between 1 January 2020 and 30 April 2021 were selected for the analysis. All the recipients received livers from either brain-dead donors or cardiac-death donors. Patients <18 years old and those lost to follow-up were excluded.
DEMOGRAPHIC CHARACTERISTICS AND CLINICAL PARAMETERS:
Collected data included demographic data such as sex, age, height, weight, body mass index (BMI), a preoperative characteristic such as Model for End-Stage Liver Disease (MELD) score, diagnosis, and indication for operation. We also collected data on intraoperative blood loss, red blood cell transfusion, and plasma transfusion. Laboratory tests included platelet count (PLT), platelet aggregation rate (induced by arachidonic acid or adenosine diphosphate, represented by AA or ADP), and TEG values. Patients were followed up to assess survival at 14 days and 3 months after OLT, re-transplantation, postoperative complications including thrombotic events, infection, postoperative bleeding, and acute kidney injury (AKI). Thrombotic events were defined as hepatic artery thrombosis and portal vein thrombosis diagnosed by ultrasound or reoperation. AKI was defined by the Kidney Disease Improving Global Outcome (KDIGO) 2012 consensus criteria. To overcome the effect of platelet count on platelet aggregation, we normalized the level of ADP-induced platelet aggregation to each patient’s platelet count using a PLT ratio: (ADP-induced platelet aggregation/PLT)×1000.
STATISTICAL ANALYSIS:
Normally distributed continuous variables are reported as mean values ± standard deviation and non-normally distributed continuous variables as median (interquartile range, IQR). Nominal variables are reported as counts and percentages. We used the t test or Mann Whitney U test for group comparisons where appropriate. Pearson’s chi-square test or Fisher’s exact test was used to compare nominal percentages. The generalized linear model was used to investigate the association between the target risk factors and outcomes. The covariates considered were age, sex, baseline MELD score [16], indication of transplantation, red blood cell transfusion, and preoperative thrombotic events [17]. Odds ratio (OR) with 95% CI for association were calculated. In the regression model, only patients with complete data in all variables were considered. P<0.05 indicated statistical significance. Statistical analysis was conducted by using Stata SE version 15.0 and figures were created by utilizing GraphPad Prism version 8.0.
Results
GENERAL CHARACTERISTICS OF PATIENTS:
During the study period, 256 adult patients were finally identified. Based on clinical outcomes at three months after OLT, we divided patients into a survival group and a death group. The demographic and clinical features of the patients included in the study are shown in Table 1. The median age of patients was 51.5 years old (IQR: 43.0–58.5); median height was 1.70 meters (IQR: 1.63–1.73); median weight was 67 kilograms (IQR: 58–78); and median BMI was 23.44 (20.91–26.35). The median MELD score was 13.0 (IQR: 10.0–21.5). Viral hepatitis cirrhosis (177/256, 69.14%) and malignant tumor (117/256, 45.31%) were the most common indications of transplantation.
As shown in Table 2, the median blood loss during the operation was 600 (IQR: 400–1000) milliliters, the median red blood cell transfusion was 4.0 (IQR: 1.5–8.0) units, and the median plasma infusion was 600 (IQR: 0–1000) milliliters. Preoperative clinical parameters are shown in Table 3.
Within the 14 days after the OLT, 68 (26.56%) patients suffered from postoperative complication, such as thrombosis (5/256, 1.95%) or severe bleeding event (9/256, 3.52%) which resulted in re-transplantation, acute kidney injury (32/256, 32.50%), and infection (27/256, 10.55%). The median length of stay in the intensive care unit (ICU) was 3 days (IQR: 1–4), and the median length of hospital stay was 22 days (IQR: 17–31). After 3 months of follow-up, 233 (91.02%) out of 256 patients survived, while 54 (21.09%) patients experienced readmission due to hepatic insufficiency, biliary stricture, infection, etc. The causes of death included abdominal bleeding, septic shock, primary graft dysfunction, acute myocardial infarction, and cerebral hemorrhage.
PRIMARY HEMOSTASIS DURING THE EARLY POSTOPERATIVE PERIOD OF OLT: FIRST DECREASED, THEN RETURNED TO PRE-TRANSPLANTATION LEVEL, THEN INCREASED BACK TO NORMAL RANGE:
Perioperative primary hemostasis status analysis (Figure 1) showed a decline of PLT and platelet aggregation functions before OLT. The median PLT was 61.5×(39.5–106.3)×109/L; the initial PLT below 100×109/L was reported in 169 (66.02%) patients. None of the patients underwent splenectomy prior to the OLT in the present study. The median platelet aggregation function induced by ADP (35.0% (14.8–62.4)%) and AA (41.1% (13.3–66.5)%) was less than the lower limit of the normal range.
Within three days after transplantation, the median platelet count in the study group decreased significantly, while the platelet aggregation induced by ADP and AA changed little. One week after transplantation, the median of PLT returned to the preoperative level. Two weeks after transplantation, the median of both PLT (143.0 (85.0–209.0)×109/L), platelet aggregation function induced by ADP (68.7% (58.0–76.5)%), and AA (69.7% (54.2–79.1)%) were higher than preoperative level. In particular, ADP in 150 (58.59%) patients and AA in 136 (53.13%) patients were beyond the normal higher limit value.
Perioperative TEG parameter analysis showed that the median MA value, which represents the number and function of platelet, was 43.1 (34.5–56.2) mm. The initial MA value in 118 (46.09%) patients was lower than the normal lower limit range. Two weeks after transplantation, the median MA value rose to 56.7 (52.2–62.7) mm. MA values in 53 (20.70%) patients were beyond the upper normal value limit, which indicated that the number and function of platelets 2 weeks after transplantation led to a hypercoagulable state compared with perioperative status (Figure 2).
ASSOCIATION BETWEEN PLATELET AGGREGATION AND CLINICAL OUTCOMES OF ADULT PATIENTS UNDERWENT OLT: THE HIGHER THE RECOVERY OF FUNCTION, THE HIGHER THE SURVIVAL PROBABILITY:
Detailed results of univariate analysis are shown in Table 4A and 4B. Based on that, we selected parameters on day 7 after OLT for further multivariable analysis. Results of regression models are shown in Tables 5 and 6. Higher PLT was associated with higher survival at 14 days after transplantation (OR: 1.07, 95% CI: 1.02–1.13, P = 0.006), but it did not show significant correlation with survival at 3 months after transplantation. On the contrary, a higher PLT ratio was associated with survival at 3 months after transplantation (OR: 2.55, 95% CI: 1.01–6.42, P=0.047) but did not show significant correlation with survival at 14 days after transplantation. As for MA value, the correlation with survival at both 14 days (OR: 1.12, 95% CI: 1.04–1.21, P=0.003) and 3 months (OR: 1.14, 95% CI: 1.01–1.30, P=0.037) after transplantation was statistically significant.
Figure 3 and Table 7 show results from AUROC analysis. The AUROC value of MA value was 0.802 (95% CI: 0.661–0.983) while that of the PLT was 0.559 (95% CI: 0.337–0.823). The AUROC value of ADP-induced platelet aggregation was 0.729 (95% CI: 0.618–0.914), and AA-induced platelet aggregation was 0.663 (95% CI: 0.538–0.933). Predictive values of PLT, ADP-induced platelet aggregation, AA-induced platelet aggregation, and PLT ratio for the survival at 14 days after transplantation are shown in Figure 4 and Table 8. The cutoff for MA value predicting survival of 3 months after transplantation was 40.6 mm. We found that 27.6% (8/29) patients with MA value less than 40.6 mm at day 7 after transplantation died, while 6.8% (15/219) of the other patients died (P=0.004).
Notably, Table 9 shows that using MA value, MELD score, and age in combination to predict the survival at 3 months after transplantation could boost the AUROC score to 0.945, and Figure 5 shows the ROC curve of combining MA value, MELD score, and age for predicting survival at 3 months after transplantation.
Discussion
In this study, we retrospectively analyzed the information of adult patients who successfully underwent OLT in Ren Ji Hospital, Shanghai Jiao Tong University School of Medicine between 1 January 2020 and 30 April 2021. The purpose of this study was to evaluate whole-blood platelet aggregation function during the perioperative period of OLT patients and its association with outcomes.
These results revealed that the preoperative coagulation abnormalities of patients on the waiting list for LT were mainly characterized by decreased PLT and platelet aggregation. Because of the relative lack of coagulant substances and anticoagulant substances, the preoperative blood coagulation function of the patients conformed to the characteristics of “fragile balance” [18,19]. On the first 3 days after the operation, PLT was significantly lower than the preoperative baseline. MA value indicated that platelet function was similar to that before transplantation, which was similar to ADP-induced and AA-induced platelet aggregation.
One week after OLT, PLT rose to pre-transplantation level. These results were consistent with a literature review, which suggested that high levels of platelet adhesive activity, an increased potential to generate thrombin, and temporary hypofibrinolysis are all indicative of increased hemostatic potential after transplantation [20]. Two weeks after OLT, PLT rose to a normal level, and the platelet aggregation function was significantly higher than that before the operation. MA value increased to be significantly higher than that before transplantation, suggesting that patients are still in a state of hypercoagulability.
In the process of analyzing the association between platelet aggregation and clinical outcomes, we considered PLT, platelet aggregation induced by ADP and AA, MA value, and PLT ratio at day 7 after transplantation. Platelet aggregation induced by ADP and AA both showed significant relevance to survival at 14 days and 3 months after transplantation, but the principle of platelet aggregation measurement depends on platelet count [9], and perioperative thrombocytopenia would have an inevitable impact on the results. The correlation between ADP and AA and clinical outcomes should be interpreted cautiously. Meanwhile, PLT showed significant relevance to survival at 14 days after transplantation, but showed little association with survival at 3 months after transplantation. On the contrary, PLT ratio showed significant relevance to survival at 3 months after transplantation, but showed little association with survival at 14 days after transplantation. MA value showed significant relevance to survival both at 14 days after transplantation, with an OR of 1.12 (95% CI: 1.04–1.21) p=0.003, and at 3 months after transplantation, with an OR of 1.14 (95% CI: 1.01–1.30)
A previous study found that the increase of platelet aggregation function, especially PLT ratio, indicates higher risk of further decompensation and death in patients with decompensated cirrhosis [15]. However, they excluded patients who underwent liver transplantation and just focused on patients with decompensated cirrhosis, which we think could not reflect dynamic changes of whole hemostasis status during the perioperative period of liver transplantation. In our study, PLT ratio did not show a significant correlation with survival at 14 days after transplantation, which is inconsistent with the previous study. The reason for this difference might be that the recovery of platelet number and function after liver transplantation reflects the recovery of liver function and is related to better prognosis. MA value from TEG is an expression of clot strength, reflecting platelet count and function, fibrinogen levels, and the interaction between platelets and fibrinogen [21]. Specifically, in patients who underwent LT, preoperative MA value is an independent factor correlated with an increased incidence of early HAT [22]. Our study showed better correlation with the survival at 14 days and 3 months after transplantation, which indicated that MA value, which comprehensively reflects platelet count and function, might be better than single platelet count or platelet aggregation induced by ADP or AA. Increase of platelet count and platelet aggregation parameters might be a surrogate indicator for recovery of liver function, which could explain the correlation between MA value and survival outcome.
Our study has certain limitations. First, the clinical data used in the present study came entirely from the hospital’s electronic medical record system. Due to the patient’s medical condition, economic conditions, personal reasons, the integrity of doctors’ orders, and other factors, there could be some missing information, resulting in incomplete laboratory and ultrasound data, which may have biased our results. Second, this retrospective study spanned 16 months, which is relatively short; coupled with the influence of the COVID-19 virus epidemic characteristics, the number of adult orthotopic liver transplantations successfully performed during the observation period was smaller than it would be otherwise. Only 256 eligible patients were enrolled. In addition, in this retrospective study, we did not conduct a more detailed subgroup analysis of the patients. Also, limited by the technical conditions of clinical examination, we did not include platelet adhesion factors like von Willebrand factor (vwF) [23,24] and ADAMTS13, which have an important role in blood coagulation [25], so the results and conclusion might be relatively one-sided. High-quality, prospective studies with larger samples are needed to confirm the conclusions of this study.
Conclusions
We found that the change in primary hemostasis during the early postoperative period of adult orthotopic liver transplantation is mainly characterized by increased platelet count and function 14 days after transplantation. Higher PLT was associated with higher survival at 14 days after transplantation, while higher PLT ratio was associated with survival at 3 months after transplantation. Compared with single platelet count or platelet aggregation, MA value from TEG might have a better correlation with early postoperative survival. Our results indicate that a, our model using MA value, MELD score, and age reliably predicted early survival after transplantation. TEG value could be a potential indicator for predicting survival of adult transplantation patients.
Figures
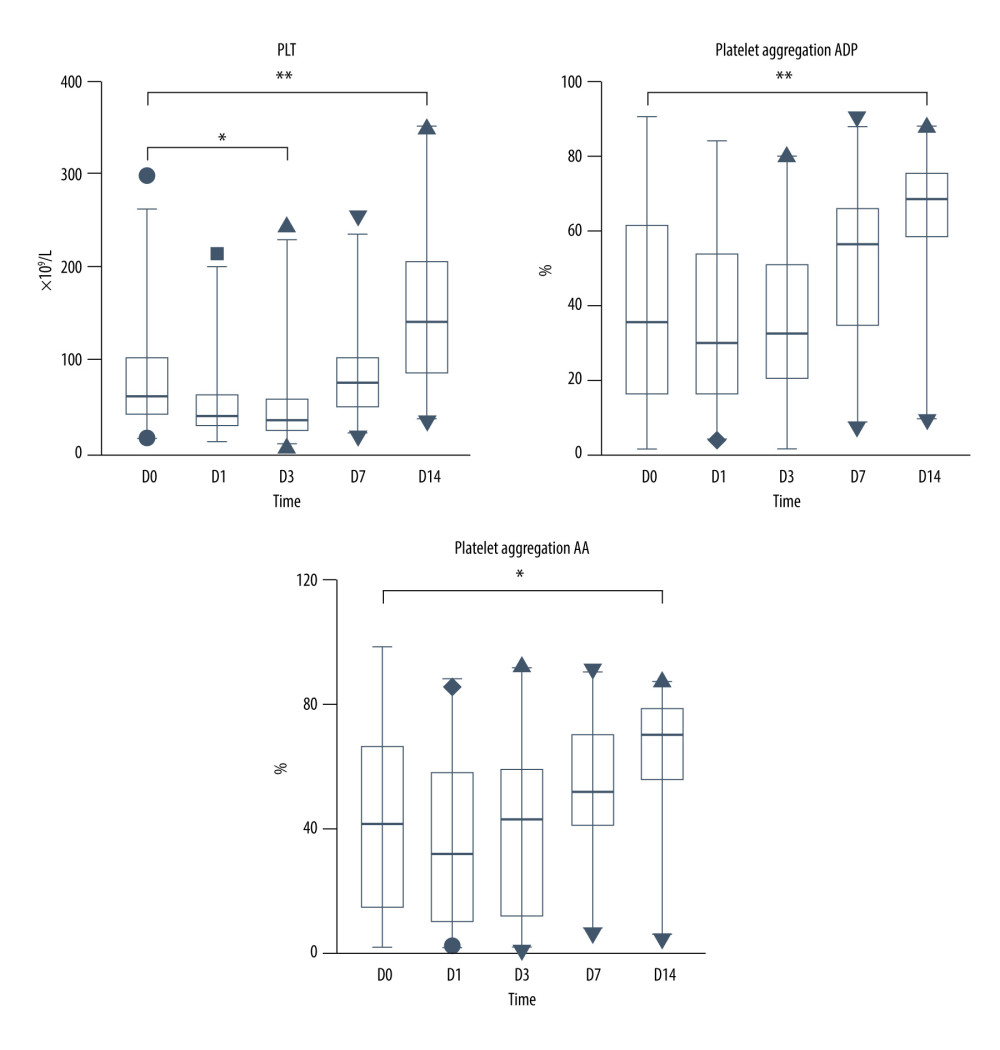 Figure 1. PLT and platelet aggregation function during the perioperative period. * p<0.05; ** p<0.0001.
Figure 1. PLT and platelet aggregation function during the perioperative period. * p<0.05; ** p<0.0001. 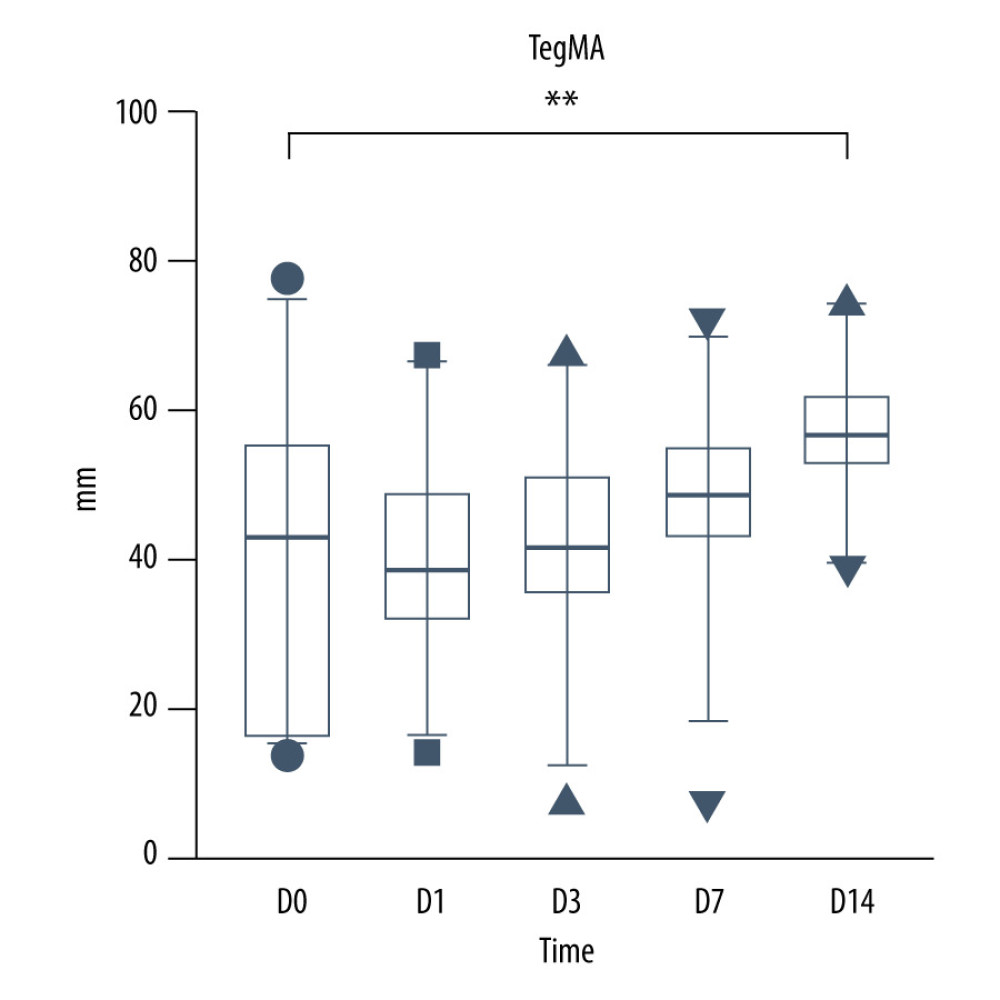 Figure 2. TEG MA value during the perioperarive period.
Figure 2. TEG MA value during the perioperarive period.  Figure 3. ROC curve of MA value, PLT, ADP-induced platelet aggregation, AA-induced platelet aggregation and PLTratio for predicting survival at 3 months after transplantation.
Figure 3. ROC curve of MA value, PLT, ADP-induced platelet aggregation, AA-induced platelet aggregation and PLTratio for predicting survival at 3 months after transplantation.  Figure 4. ROC curve of MA value, PLT, ADP-induced platelet aggregation, AA-induced platelet aggregation and PLTratio for predicting survival at 14 days after transplantation.
Figure 4. ROC curve of MA value, PLT, ADP-induced platelet aggregation, AA-induced platelet aggregation and PLTratio for predicting survival at 14 days after transplantation. 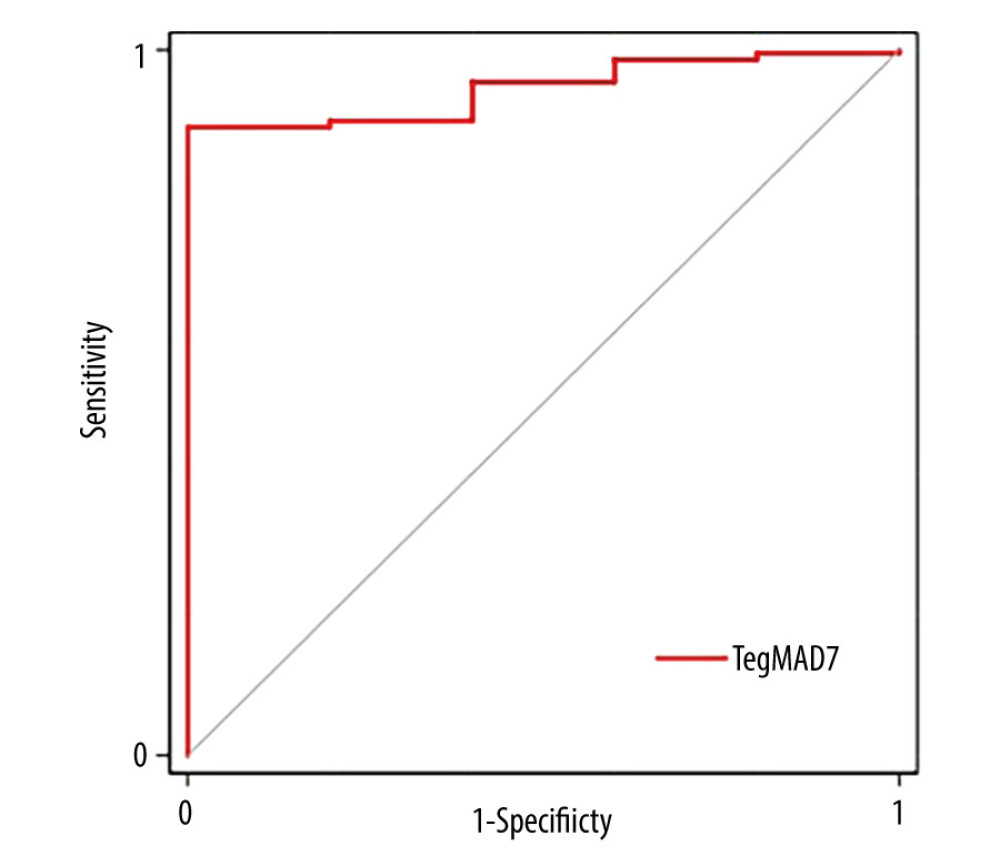 Figure 5. ROC curve of combining MA value, MELD score and age for predicting survival at 3 months after transplantation.
Figure 5. ROC curve of combining MA value, MELD score and age for predicting survival at 3 months after transplantation. Tables
Table 1. Demographic and baseline features of the study population.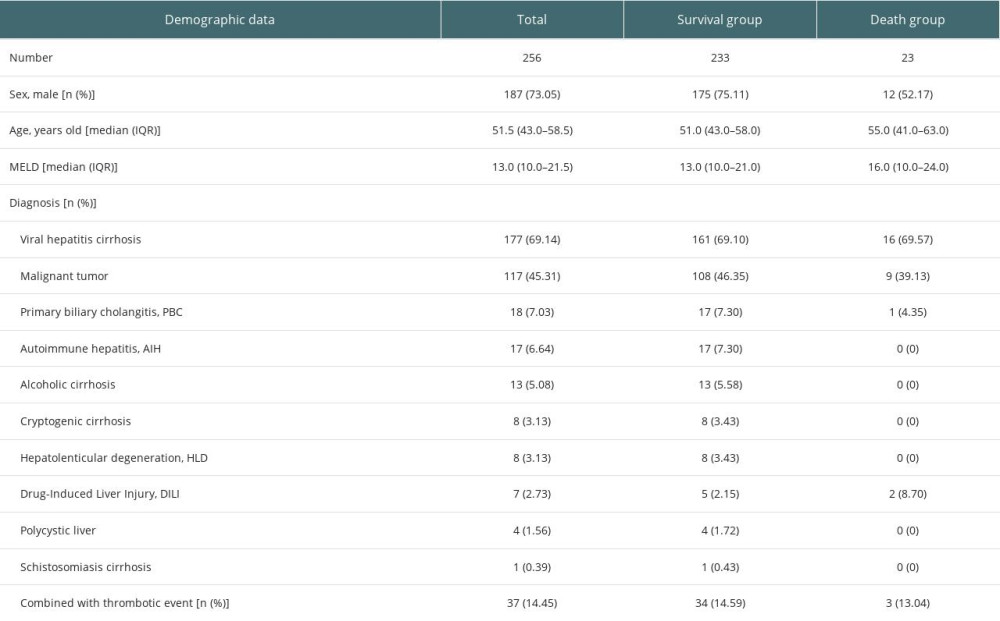 Table 2. Intraoperative and postoperative characteristics of the study population.
Table 2. Intraoperative and postoperative characteristics of the study population.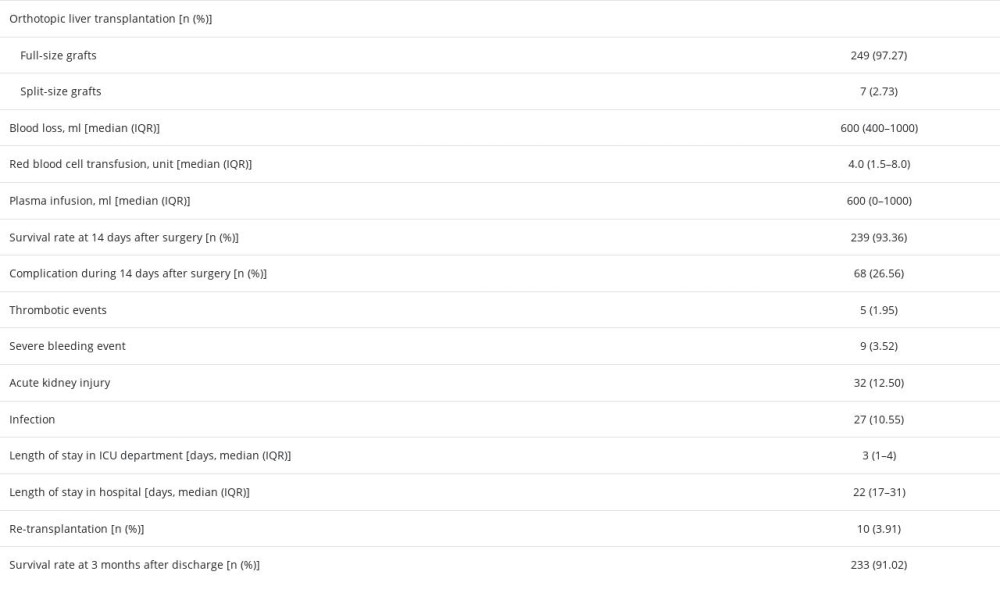 Table 3. Perioperative clinical parameters of the study population.
Table 3. Perioperative clinical parameters of the study population.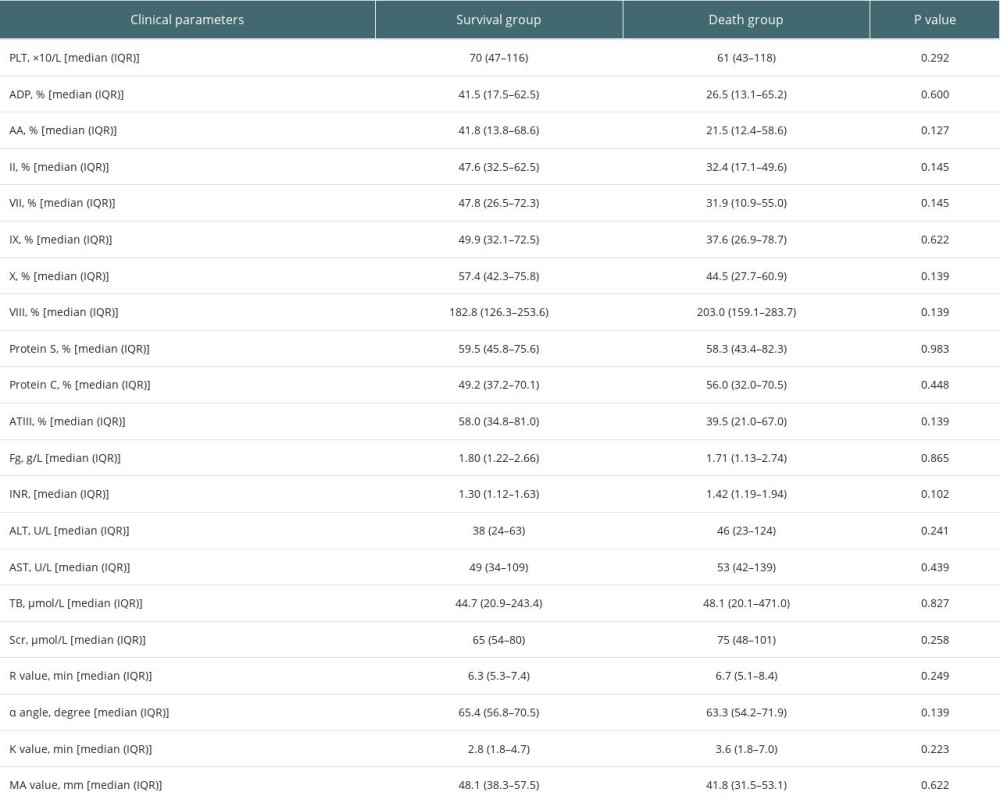 Table 4A. Univariate analysis of association between platelet aggregation and survival of adult patients underwent OLT.
Table 4A. Univariate analysis of association between platelet aggregation and survival of adult patients underwent OLT.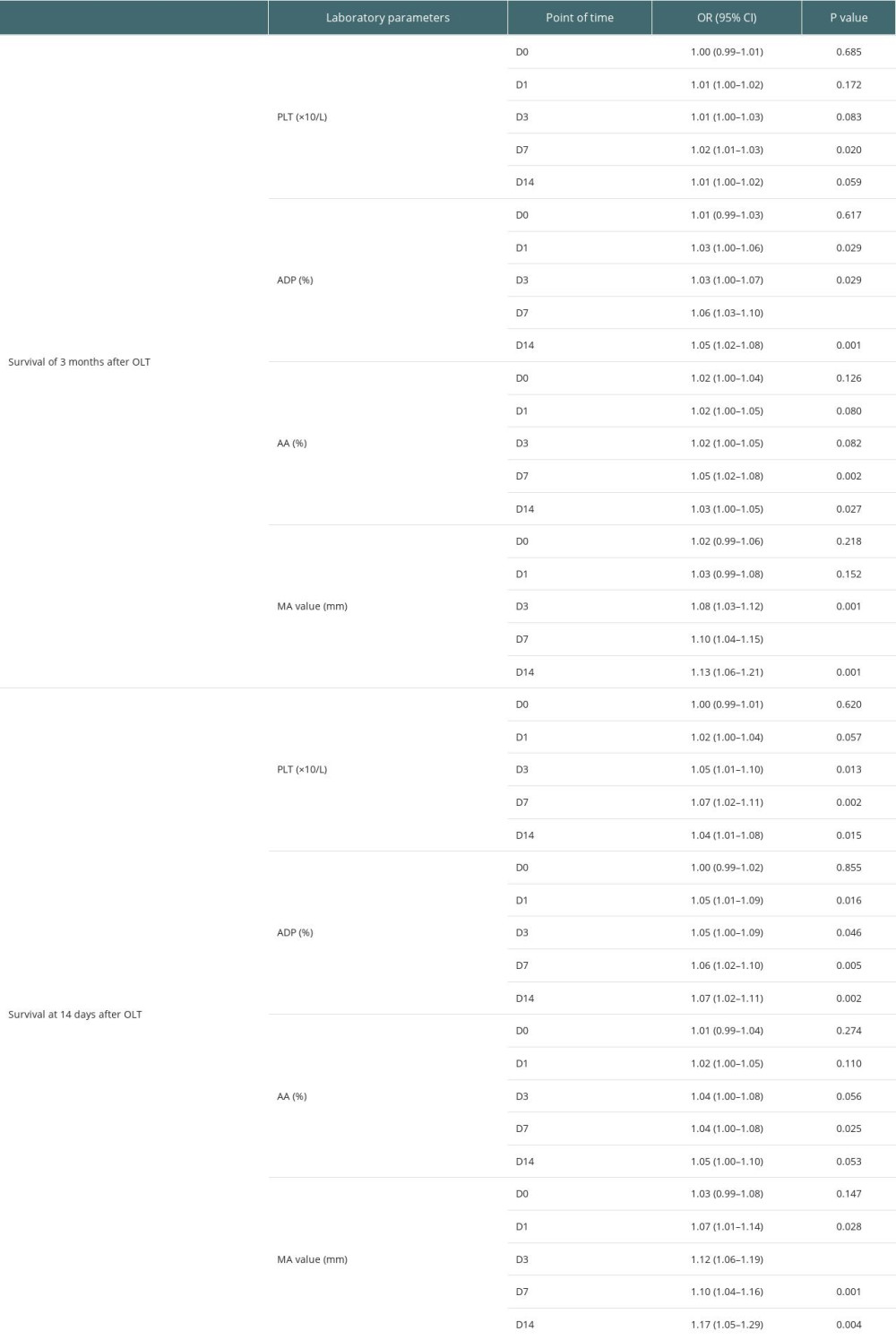 Table 4B. Univariate analysis of association between demographic and clinical parameters and survival of adult patients underwent OLT.
Table 4B. Univariate analysis of association between demographic and clinical parameters and survival of adult patients underwent OLT.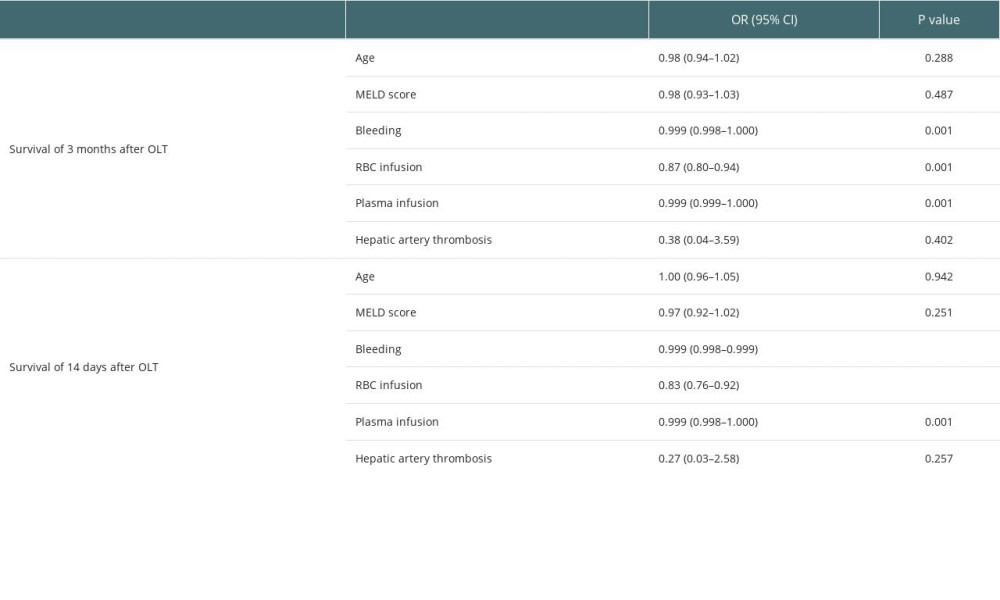 Table 5. Multivariate logistic regression analysis of the survival 14 days after transplantation.
Table 5. Multivariate logistic regression analysis of the survival 14 days after transplantation.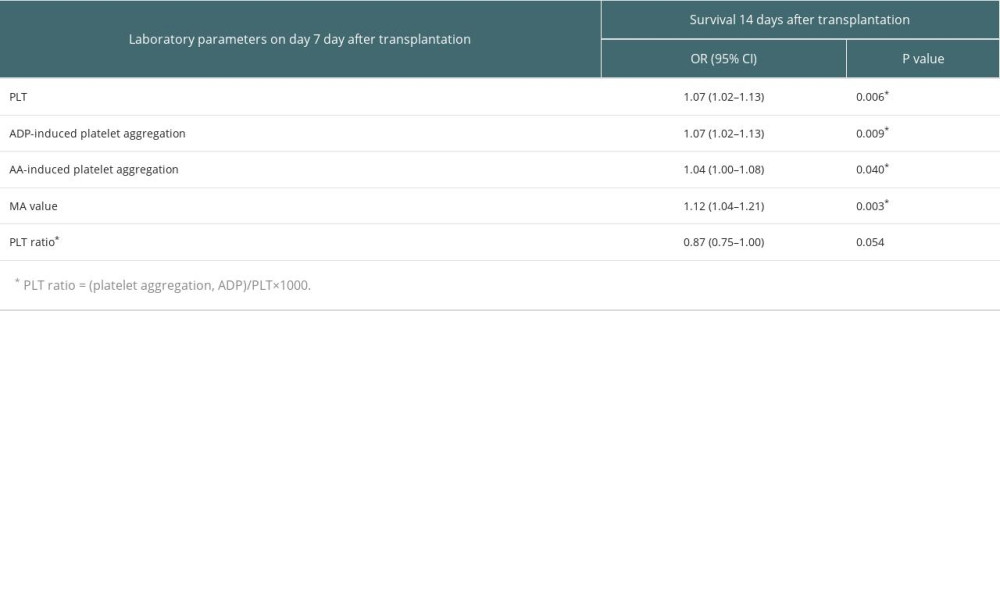 Table 6. Multivariate logistic regression analysis of the survival 3 months after transplantation.
Table 6. Multivariate logistic regression analysis of the survival 3 months after transplantation.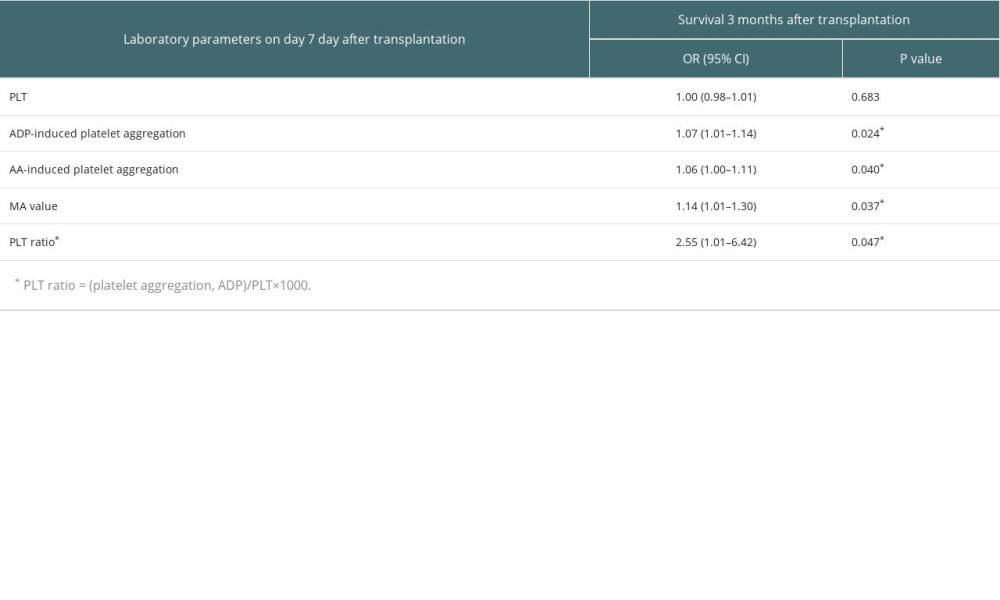 Table 7. Predictive values of PLT, ADP-induced platelet aggregation, AA-induced platelet aggregation and PLT ratio for the survival at 3 months after transplantation.
Table 7. Predictive values of PLT, ADP-induced platelet aggregation, AA-induced platelet aggregation and PLT ratio for the survival at 3 months after transplantation.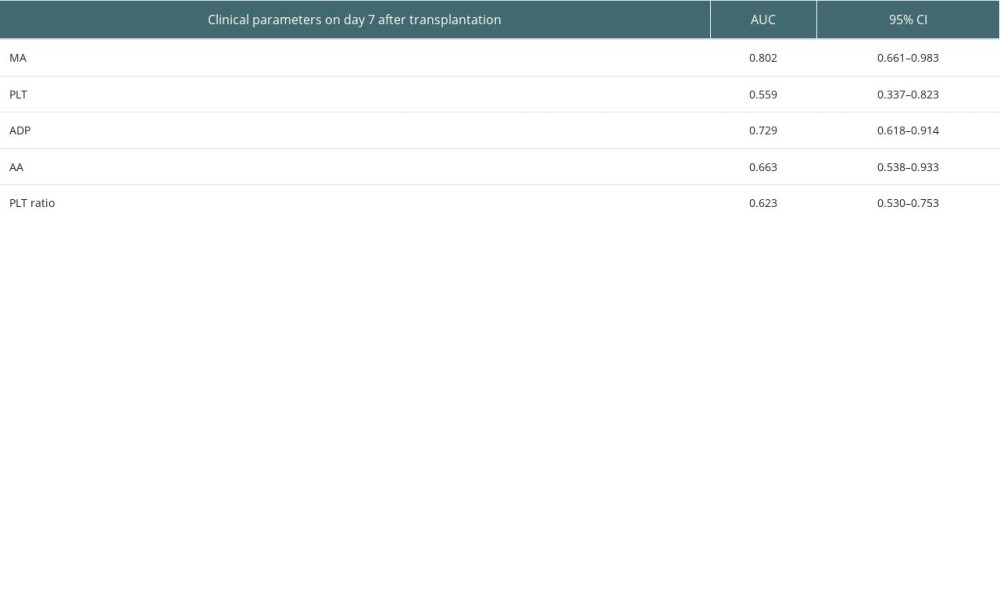 Table 8. Predictive values of MA value, PLT, ADP-induced platelet aggregation, AA-induced platelet aggregation and PLT ratio for the survival at 14 days after transplantation.
Table 8. Predictive values of MA value, PLT, ADP-induced platelet aggregation, AA-induced platelet aggregation and PLT ratio for the survival at 14 days after transplantation.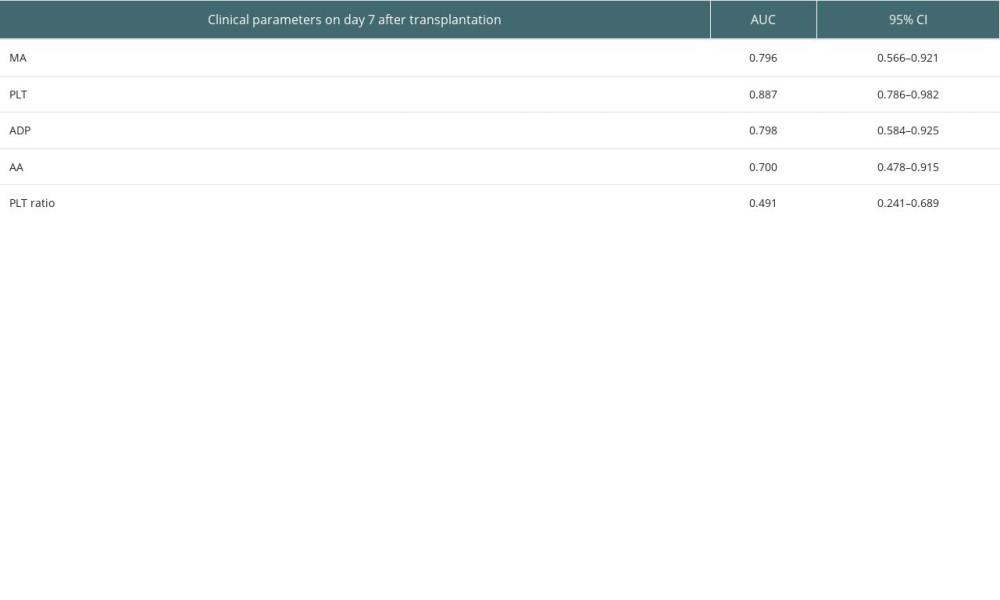 Table 9. Predictive values of MA value, MELD, and age for the survival at 3 months after transplantation.
Table 9. Predictive values of MA value, MELD, and age for the survival at 3 months after transplantation.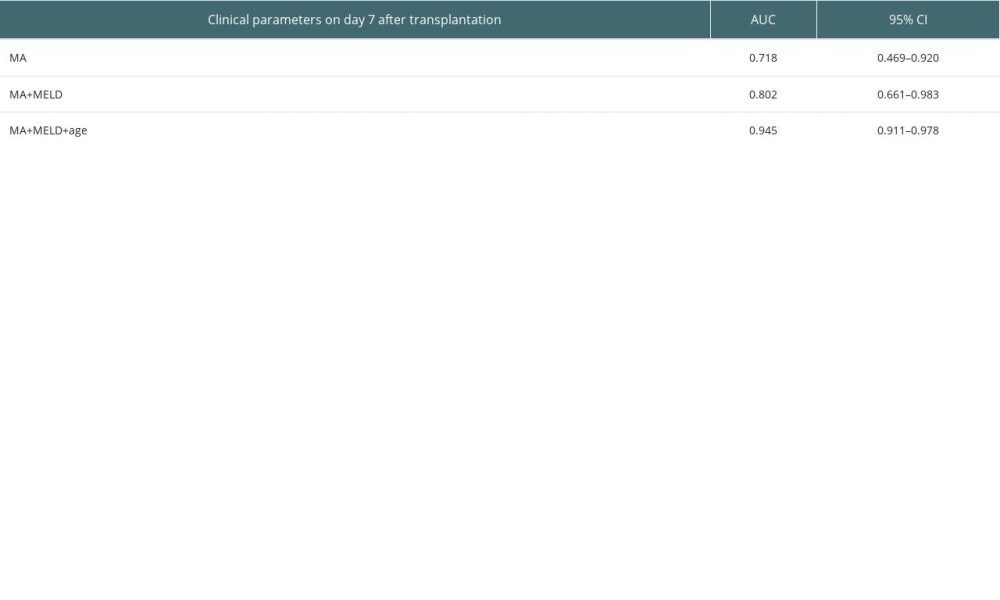
References
1. Wilke TJ, Fremming BA, Brown BA, 2020 clinical update in liver transplantation: J Cardiothorac Vasc Anesth, 2022; 36(5); 1449-57
2. Feltracco P, Barbieri S, Cillo U, Perioperative thrombotic complications in liver transplantation: World J Gastroenterol, 2015; 21(26); 8004-13
3. De Pietri L, Montalti R, Nicolini D, Perioperative thromboprophylaxis in liver transplant patients: World J Gastroenterol, 2018; 24(27); 2931-48
4. Malleeswaran S, Sivajothi S, Reddy MS, Viscoelastic monitoring in liver transplantation: Liver Transpl, 2022; 28(6); 1090-102
5. Kujovich JL, Coagulopathy in liver disease: A balancing act: Hematology Am Soc Hematol Educ Program, 2015; 2015; 243-49
6. Zanetto A, Campello E, Bulato C, Global hemostatic profiling in patients with decompensated cirrhosis and bacterial infections: JHEP Rep, 2022; 4(7); 100493
7. Northup PG, Garcia-Pagan JC, Garcia-Tsao G, Vascular liver disorders, portal vein thrombosis, and procedural bleeding in patients with liver disease: 2020 practice guidance by the American Association for the Study of Liver Diseases: Hepatology, 2021; 73(1); 366-413
8. Basili S, Raparelli V, Pignatelli P, Violi F, Pitfalls in assessing platelet activation status in patients with liver disease: Authors’ reply: Liver Int, 2012 Online ahead of print
9. Zanetto A, Senzolo M, Blasi A, Perioperative management of antithrombotic treatment: Best Pract Res Clin Anaesthesiol, 2020; 34(1); 35-50
10. Stravitz RT, Potential applications of thromboelastography in patients with acute and chronic liver disease: Gastroenterol Hepatol (NY), 2012; 8(8); 513-20
11. Kozek-Langenecker SA, Ahmed AB, Afshari A, Management of severe perioperative bleeding: Guidelines from the European Society of Anaesthesiology: First update 2016: Eur J Anaesthesiol, 2017; 34(6); 332-95
12. Salooja N, Perry DJ, Thrombelastography: Blood Coagul Fibrinolysis, 2001; 12(5); 327-37
13. Trautman CL, Palmer WC, Taner CB, Thromboelastography as a predictor of outcomes following liver transplantation: Transplant Proc, 2017; 49(9); 2110-16
14. Kohli R, Shingina A, New S, Thromboelastography parameters are associated with cirrhosis severity: Dig Dis Sci, 2019; 64(9); 2661-70
15. Zanetto A, Campello E, Bulato C, Increased platelet aggregation in patients with decompensated cirrhosis indicates higher risk of further decompensation and death: J Hepatol, 2022; 77(3); 660-69
16. Aragon Pinto C, Iyer VN, Albitar HAH, Outcomes of liver transplantation in patients with hepatopulmonary syndrome in the pre and post-MELD eras: A systematic review: Respir Med Res, 2021; 80; 100852
17. Zhong J, Smith C, Walker P, Imaging post liver transplantation part I: Vascular complications: Clin Radiol, 2020; 75(11); 845-53
18. La Mura V, Bitto N, Tripodi A, Rational hemostatic management in cirrhosis: From old paradigms to new clinical challenges: Expert Rev Hematol, 2022; 15(12); 1031-44
19. Tripodi A, Hemostasis abnormalities in cirrhosis: Curr Opin Hematol, 2015; 22(5); 406-12
20. Arshad F, Lisman T, Porte RJ, Hypercoagulability as a contributor to thrombotic complications in the liver transplant recipient: Liver Int, 2013; 33(6); 820-27
21. Pietri L, Montalti R, Bolondi G, Intraoperative thromboelastography as a tool to predict postoperative thrombosis during liver transplantation: World J Transplant, 2020; 10(11); 345-55
22. Zahr Eldeen F, Roll GR, Derosas C, Preoperative thromboelastography as a sensitive tool predicting those at risk of developing early hepatic artery thrombosis after adult liver transplantation: Transplantation, 2016; 100(11); 2382-90
23. Arshad F, Lisman T, Porte RJ, Blood markers of portal hypertension are associated with blood loss and transfusion requirements during orthotopic liver transplantation: Semin Thromb Hemost, 2020; 46(6); 751-56
24. Verhoeven CJ, Simon TC, de Jonge J, Liver grafts procured from donors after circulatory death have no increased risk of microthrombi formation: Liver Transpl, 2016; 22(12); 1676-87
25. Hartmann M, Szalai C, Saner FH, Hemostasis in liver transplantation: Pathophysiology, monitoring, and treatment: World J Gastroenterol, 2016; 22(4); 1541-50
Figures
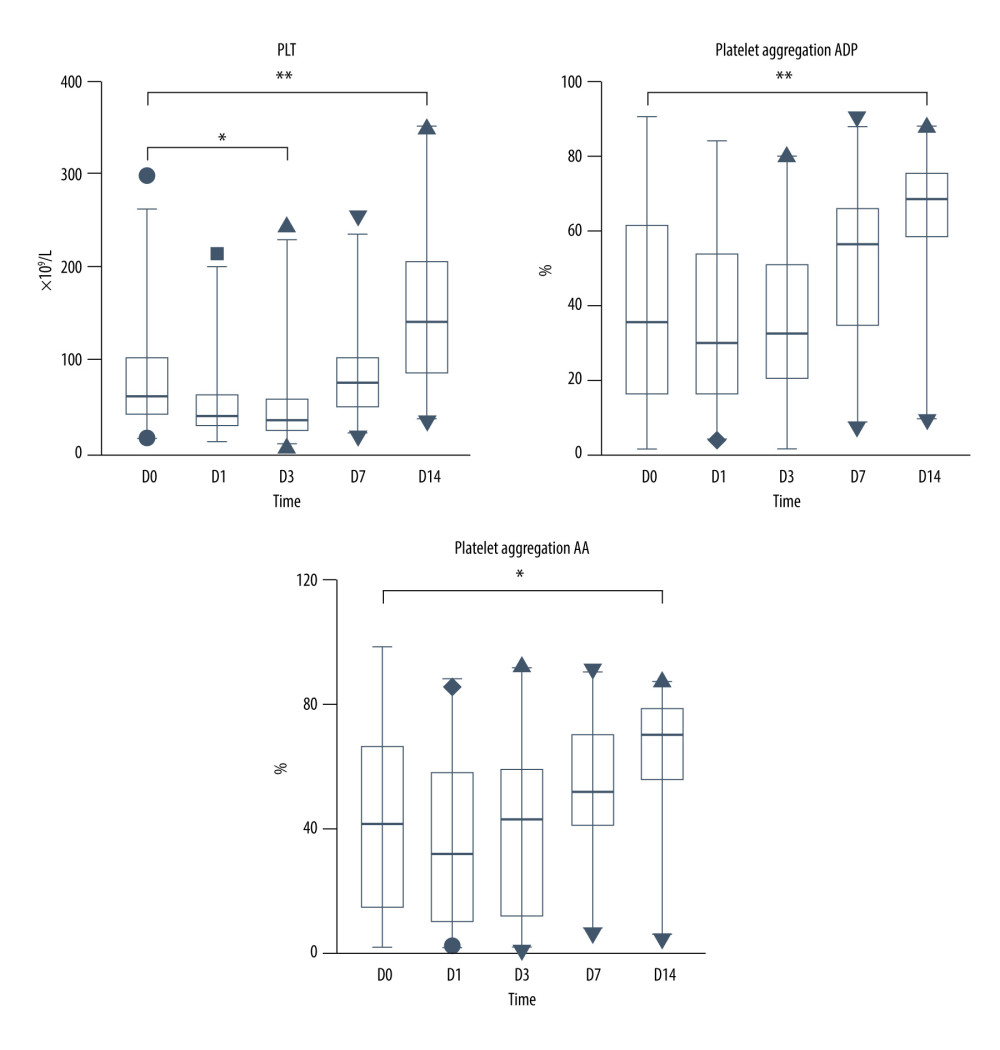 Figure 1. PLT and platelet aggregation function during the perioperative period. * p<0.05; ** p<0.0001.
Figure 1. PLT and platelet aggregation function during the perioperative period. * p<0.05; ** p<0.0001.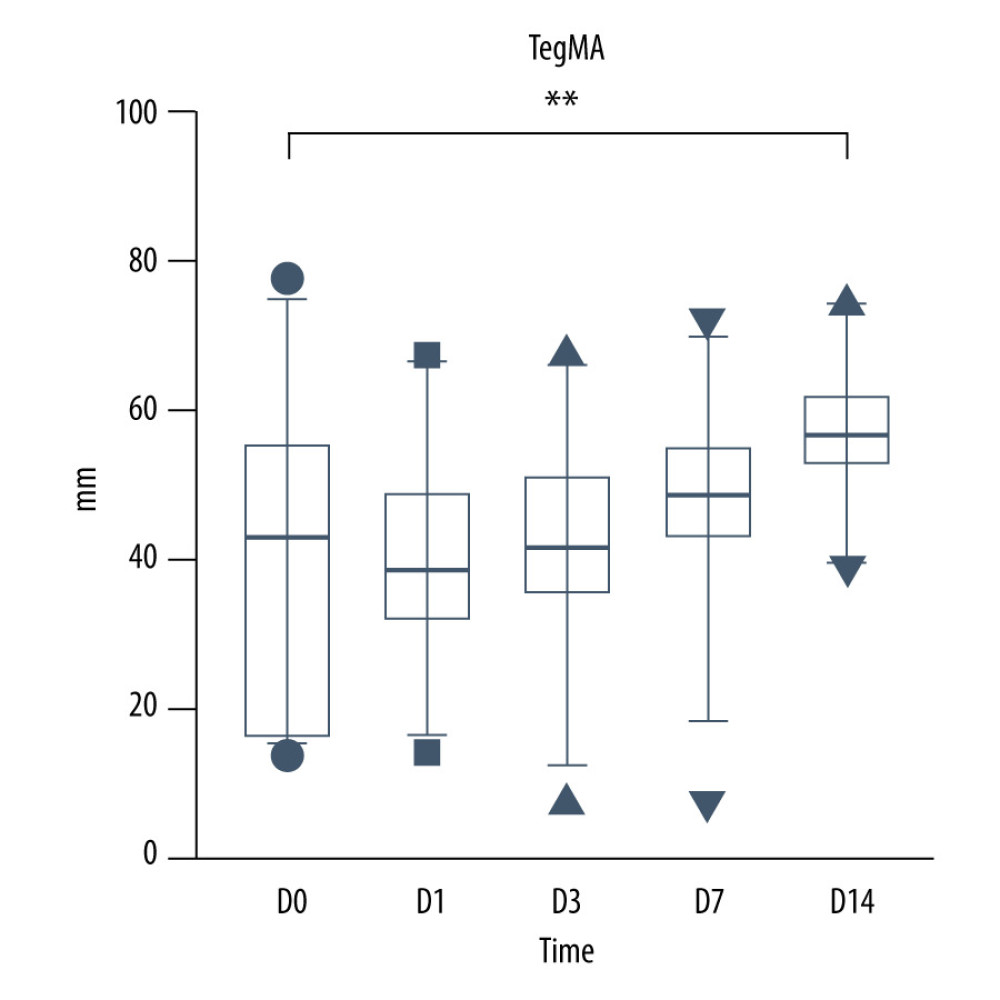 Figure 2. TEG MA value during the perioperarive period.
Figure 2. TEG MA value during the perioperarive period. Figure 3. ROC curve of MA value, PLT, ADP-induced platelet aggregation, AA-induced platelet aggregation and PLTratio for predicting survival at 3 months after transplantation.
Figure 3. ROC curve of MA value, PLT, ADP-induced platelet aggregation, AA-induced platelet aggregation and PLTratio for predicting survival at 3 months after transplantation. Figure 4. ROC curve of MA value, PLT, ADP-induced platelet aggregation, AA-induced platelet aggregation and PLTratio for predicting survival at 14 days after transplantation.
Figure 4. ROC curve of MA value, PLT, ADP-induced platelet aggregation, AA-induced platelet aggregation and PLTratio for predicting survival at 14 days after transplantation.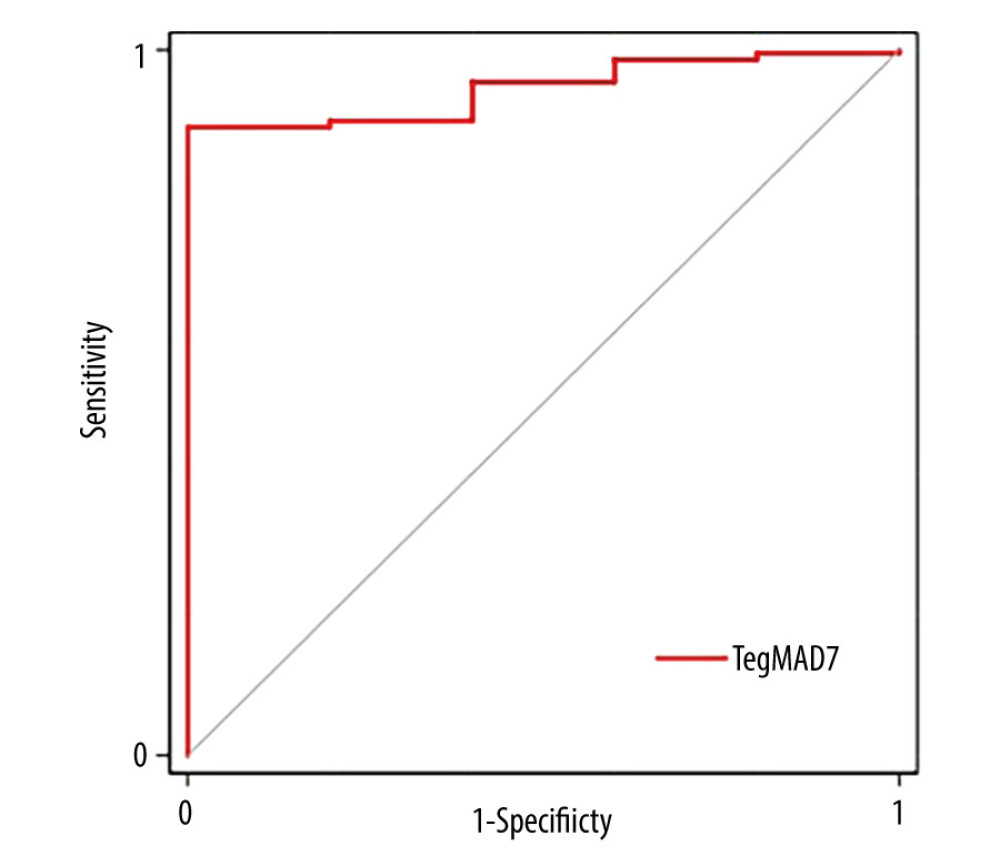 Figure 5. ROC curve of combining MA value, MELD score and age for predicting survival at 3 months after transplantation.
Figure 5. ROC curve of combining MA value, MELD score and age for predicting survival at 3 months after transplantation. Tables
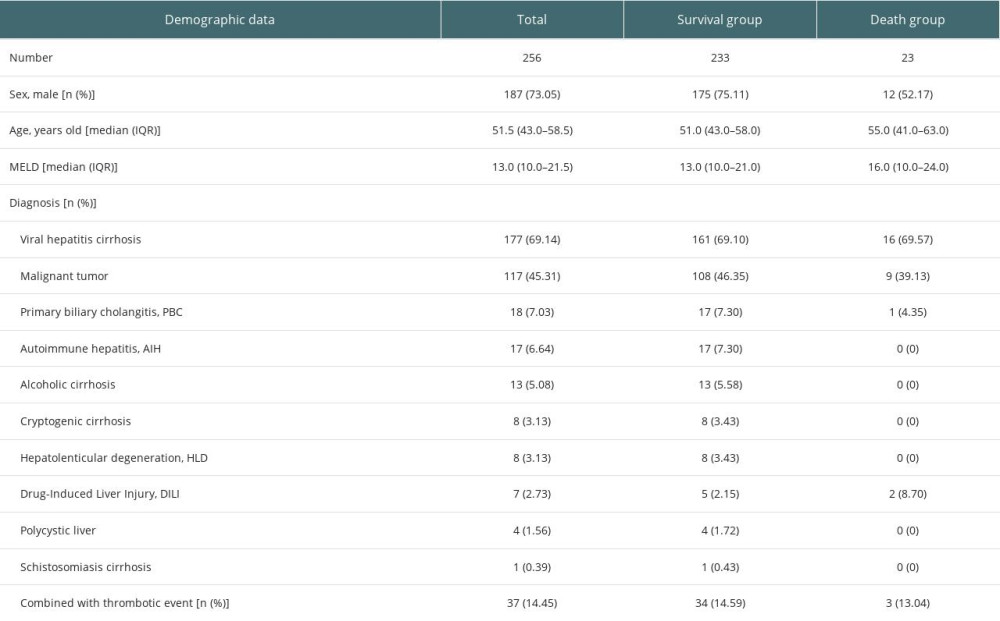 Table 1. Demographic and baseline features of the study population.
Table 1. Demographic and baseline features of the study population.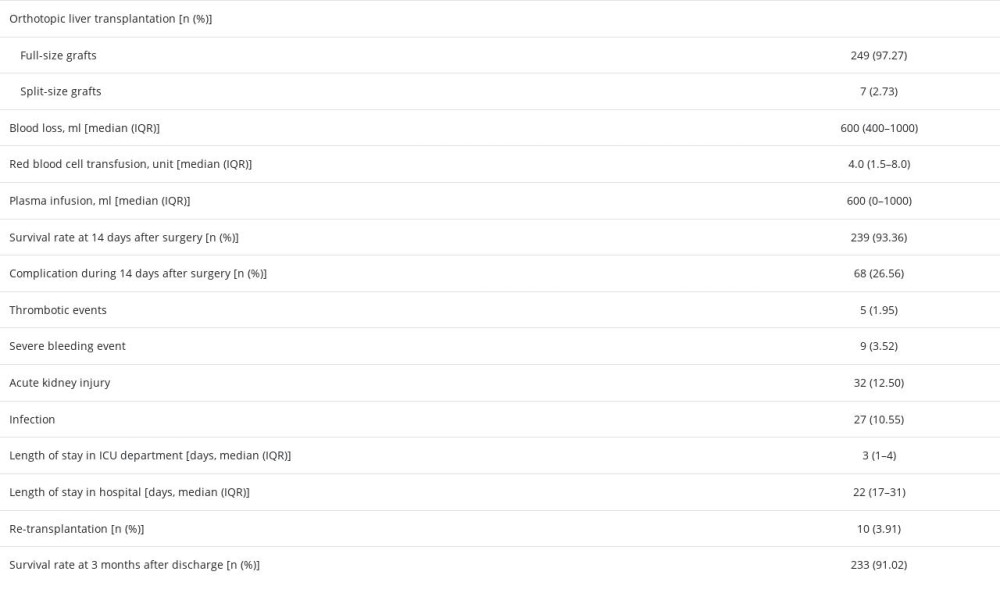 Table 2. Intraoperative and postoperative characteristics of the study population.
Table 2. Intraoperative and postoperative characteristics of the study population.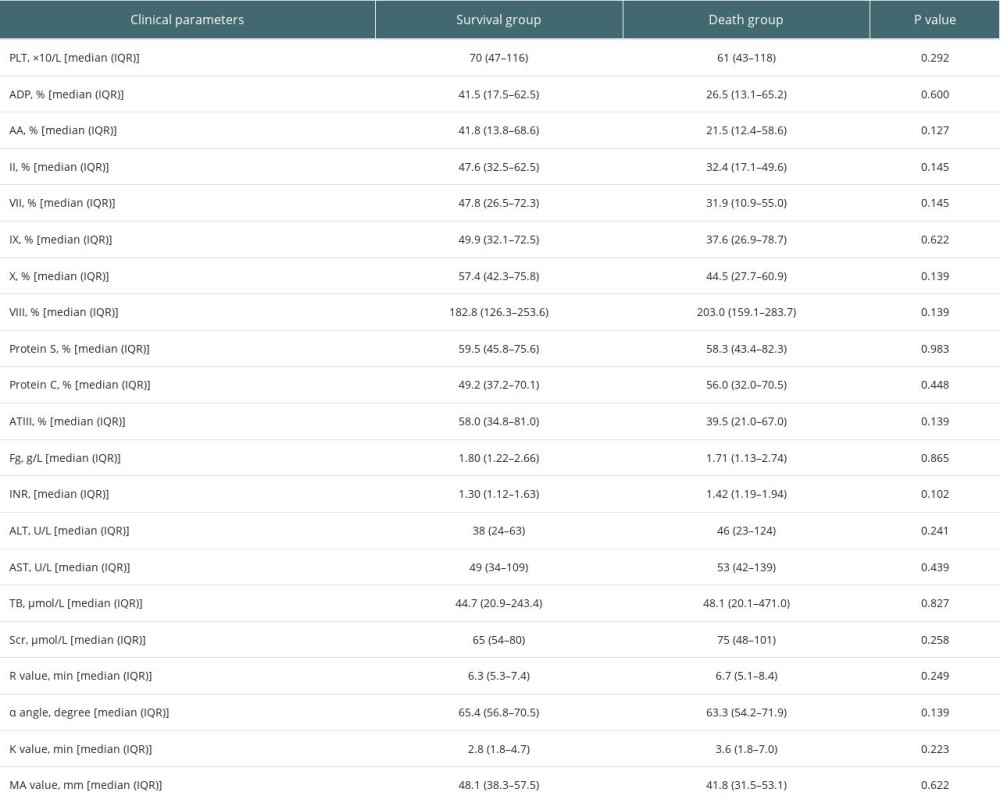 Table 3. Perioperative clinical parameters of the study population.
Table 3. Perioperative clinical parameters of the study population.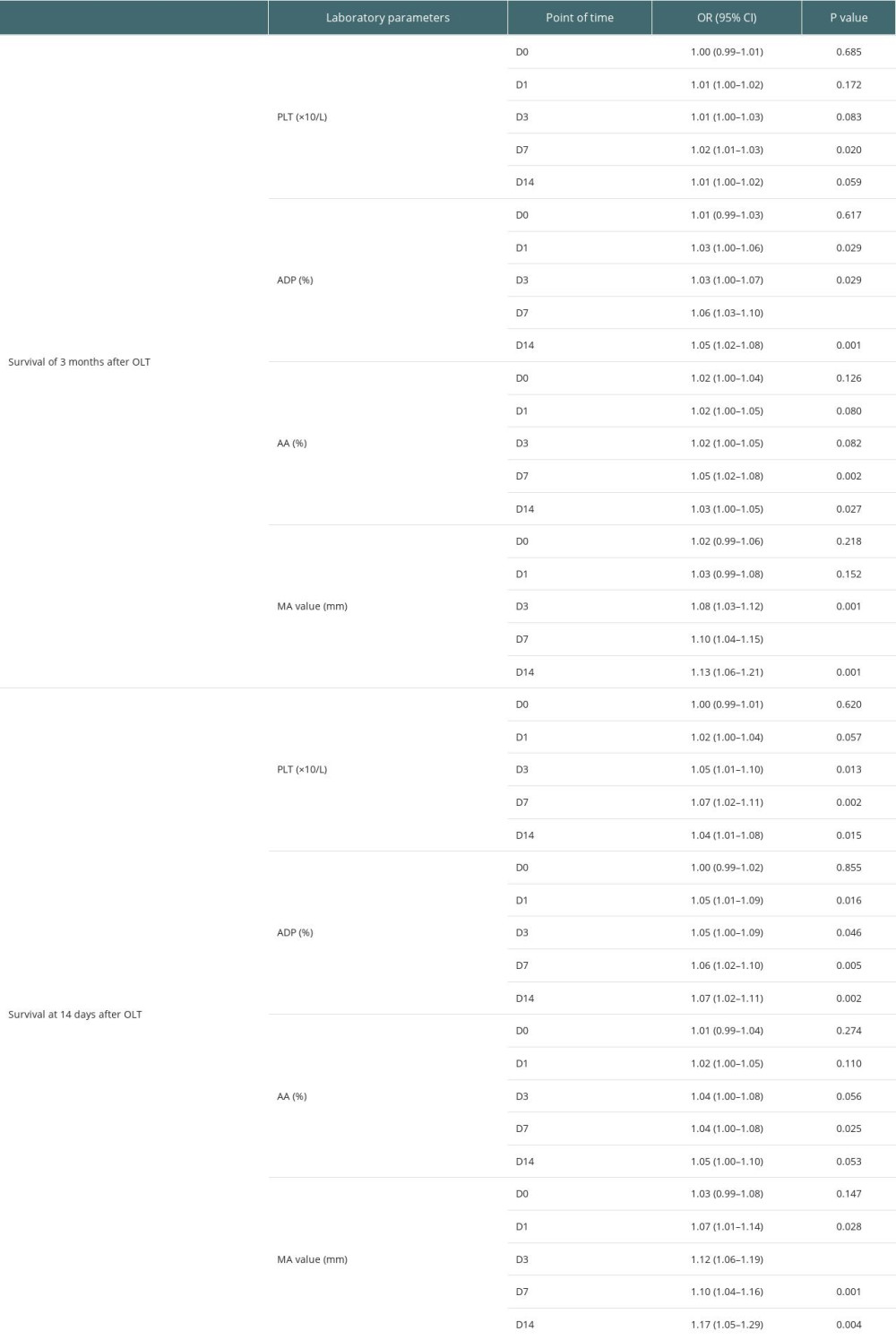 Table 4A. Univariate analysis of association between platelet aggregation and survival of adult patients underwent OLT.
Table 4A. Univariate analysis of association between platelet aggregation and survival of adult patients underwent OLT.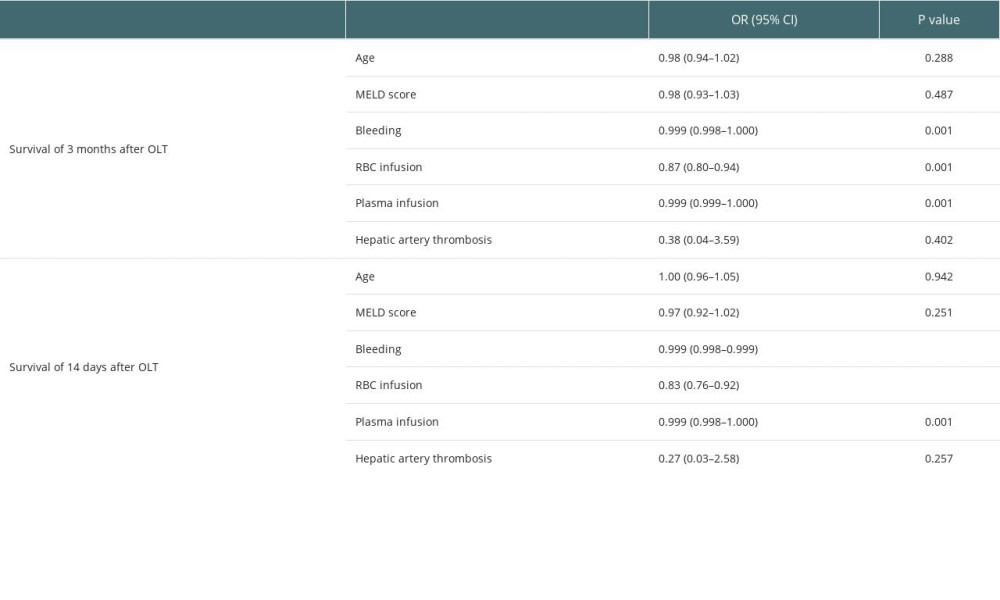 Table 4B. Univariate analysis of association between demographic and clinical parameters and survival of adult patients underwent OLT.
Table 4B. Univariate analysis of association between demographic and clinical parameters and survival of adult patients underwent OLT.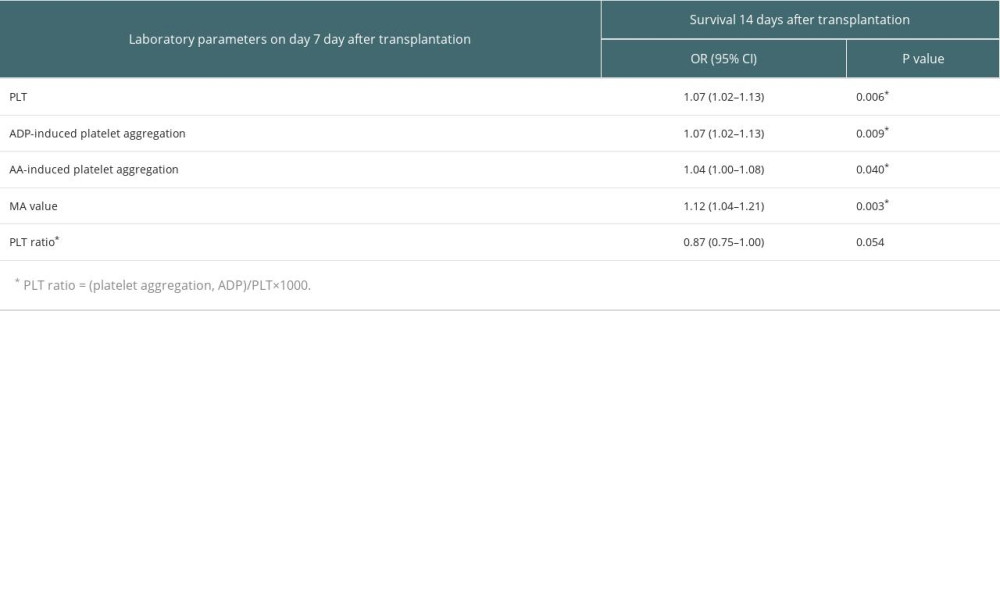 Table 5. Multivariate logistic regression analysis of the survival 14 days after transplantation.
Table 5. Multivariate logistic regression analysis of the survival 14 days after transplantation.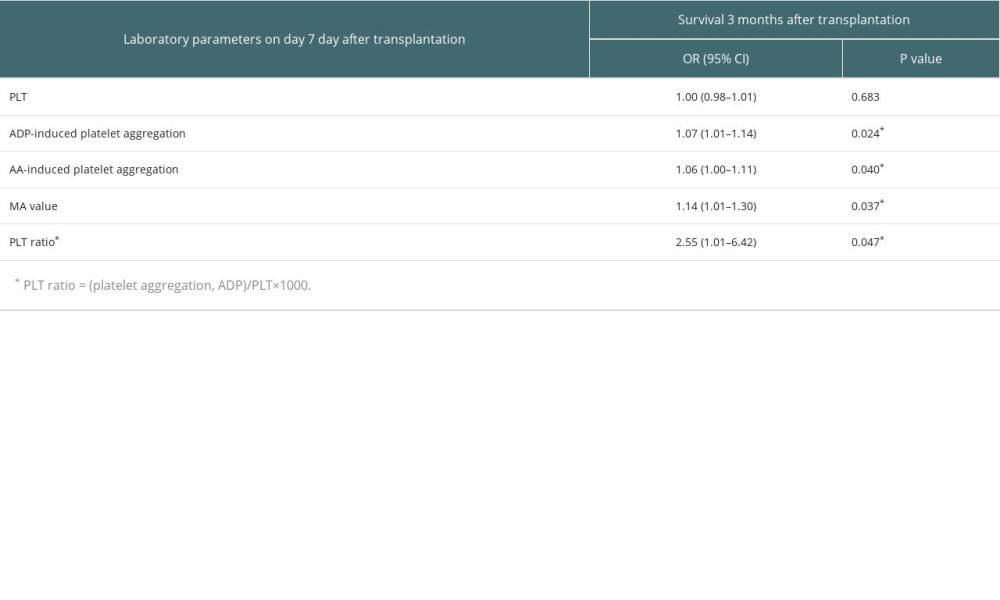 Table 6. Multivariate logistic regression analysis of the survival 3 months after transplantation.
Table 6. Multivariate logistic regression analysis of the survival 3 months after transplantation.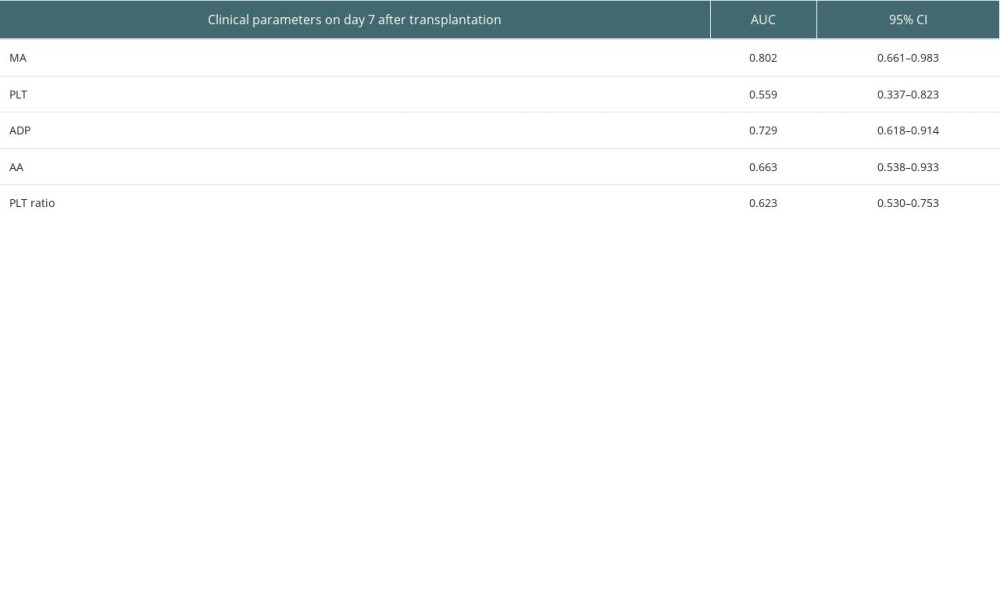 Table 7. Predictive values of PLT, ADP-induced platelet aggregation, AA-induced platelet aggregation and PLT ratio for the survival at 3 months after transplantation.
Table 7. Predictive values of PLT, ADP-induced platelet aggregation, AA-induced platelet aggregation and PLT ratio for the survival at 3 months after transplantation.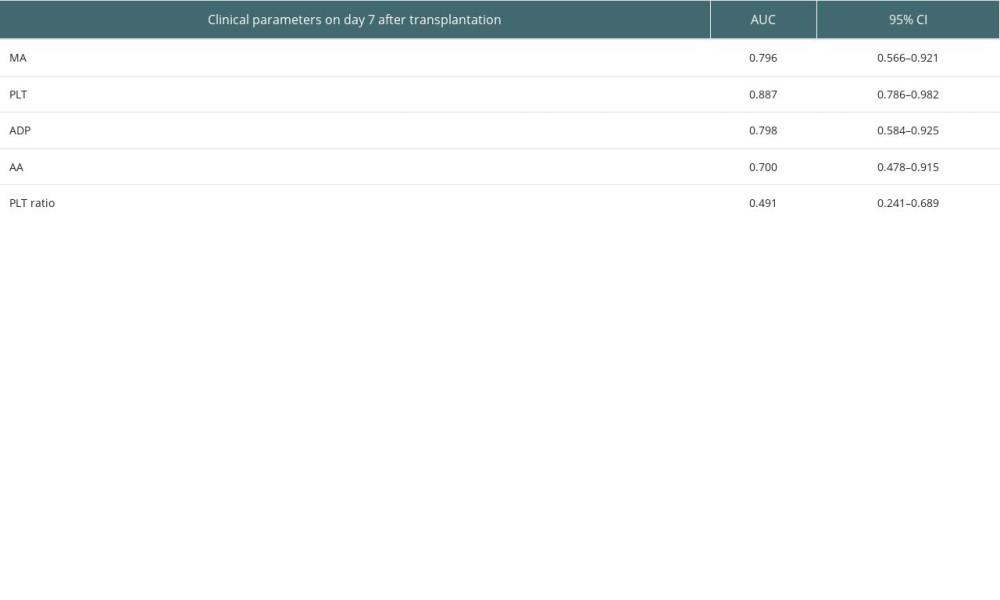 Table 8. Predictive values of MA value, PLT, ADP-induced platelet aggregation, AA-induced platelet aggregation and PLT ratio for the survival at 14 days after transplantation.
Table 8. Predictive values of MA value, PLT, ADP-induced platelet aggregation, AA-induced platelet aggregation and PLT ratio for the survival at 14 days after transplantation.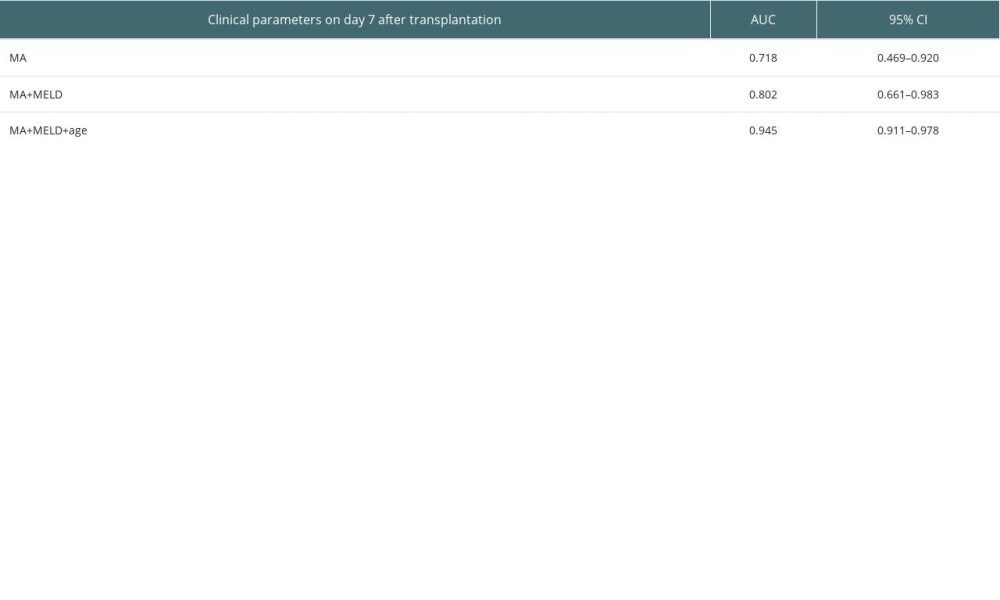 Table 9. Predictive values of MA value, MELD, and age for the survival at 3 months after transplantation.
Table 9. Predictive values of MA value, MELD, and age for the survival at 3 months after transplantation.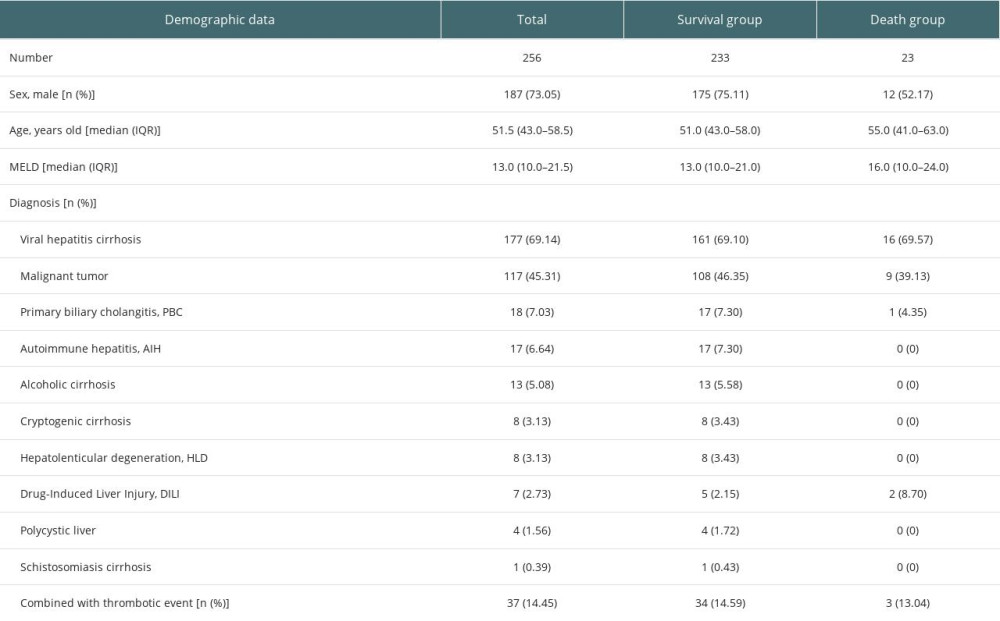 Table 1. Demographic and baseline features of the study population.
Table 1. Demographic and baseline features of the study population.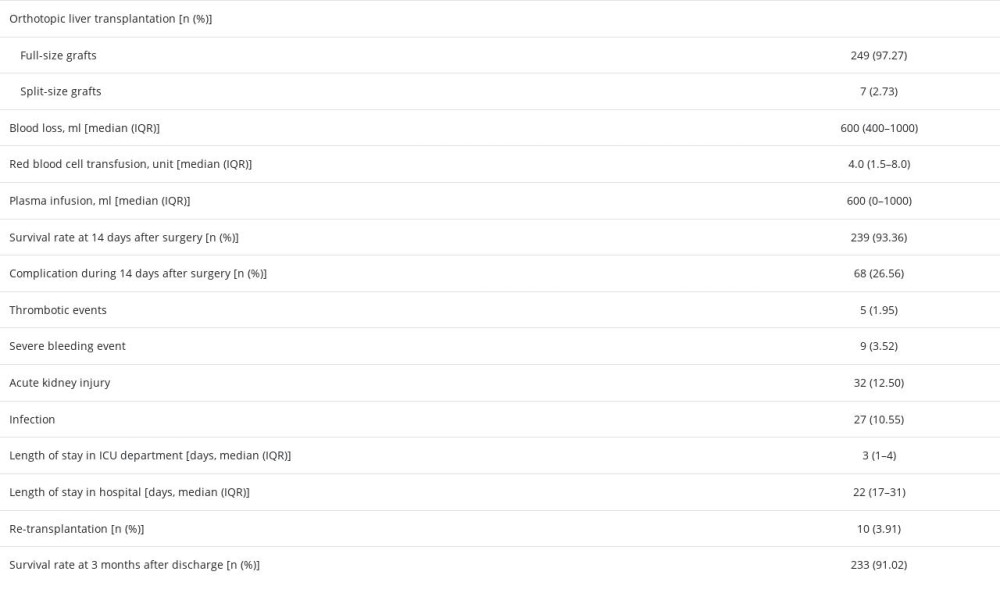 Table 2. Intraoperative and postoperative characteristics of the study population.
Table 2. Intraoperative and postoperative characteristics of the study population.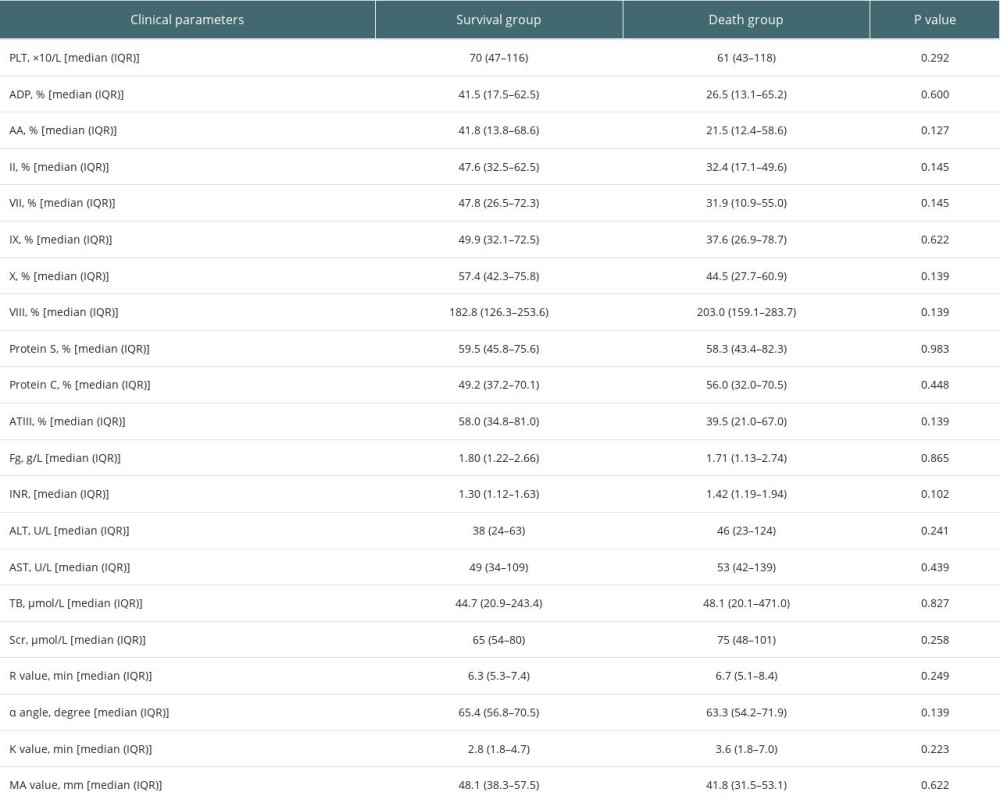 Table 3. Perioperative clinical parameters of the study population.
Table 3. Perioperative clinical parameters of the study population.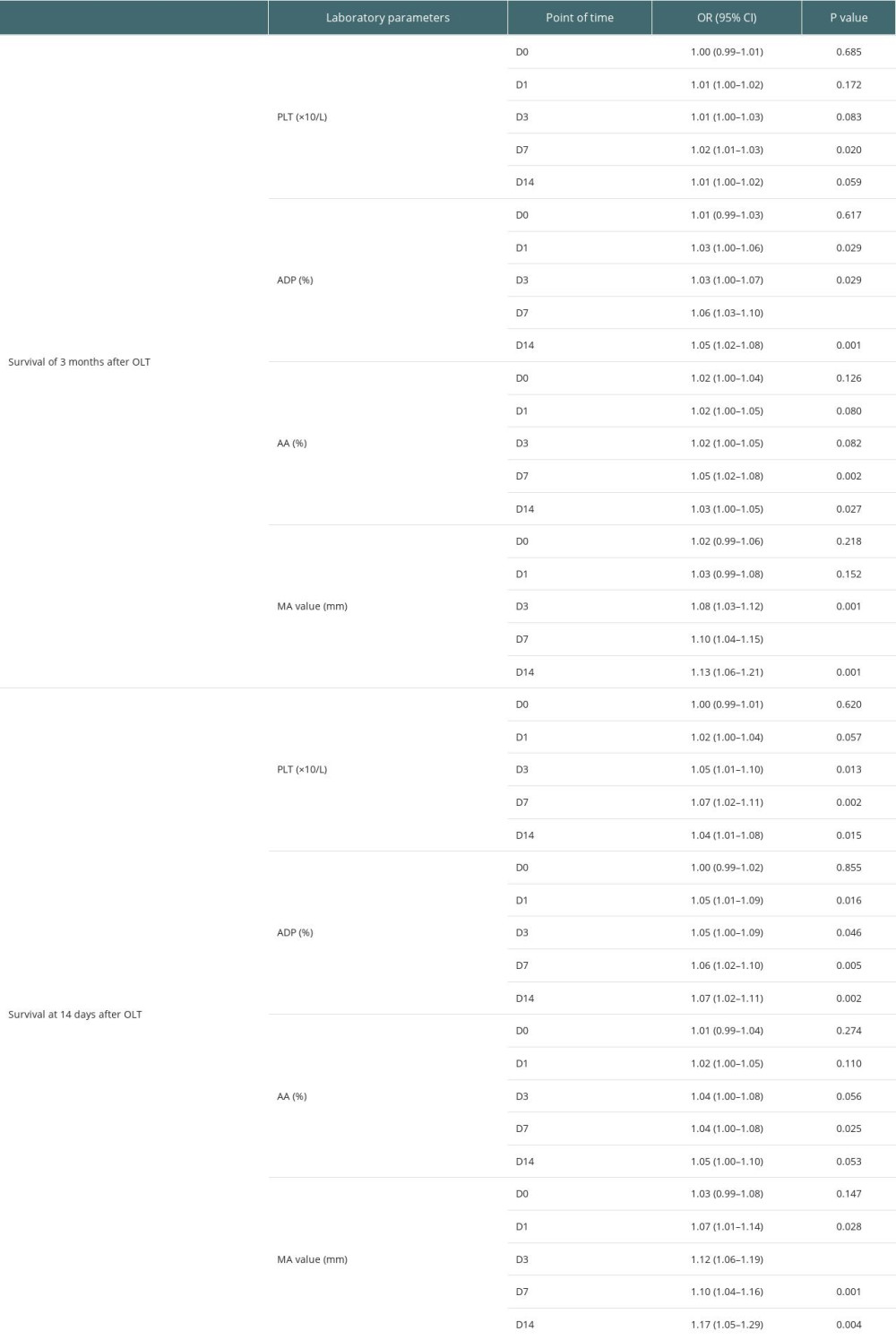 Table 4A. Univariate analysis of association between platelet aggregation and survival of adult patients underwent OLT.
Table 4A. Univariate analysis of association between platelet aggregation and survival of adult patients underwent OLT.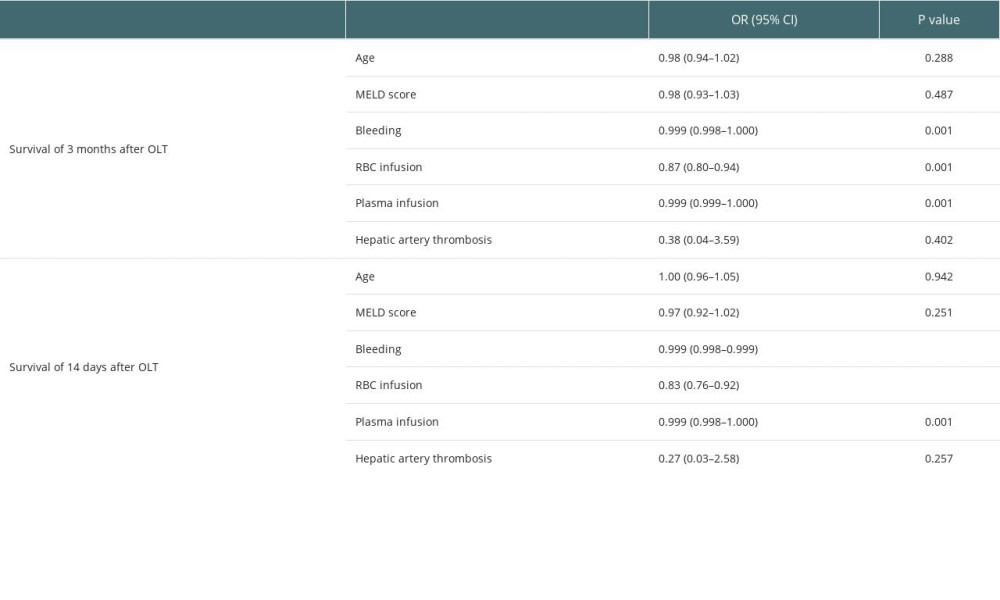 Table 4B. Univariate analysis of association between demographic and clinical parameters and survival of adult patients underwent OLT.
Table 4B. Univariate analysis of association between demographic and clinical parameters and survival of adult patients underwent OLT.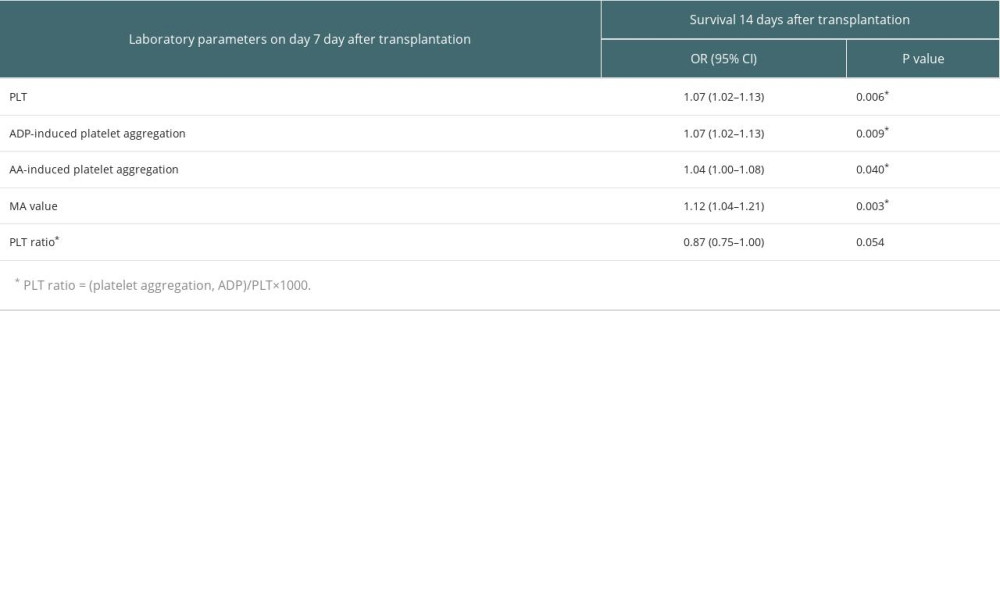 Table 5. Multivariate logistic regression analysis of the survival 14 days after transplantation.
Table 5. Multivariate logistic regression analysis of the survival 14 days after transplantation.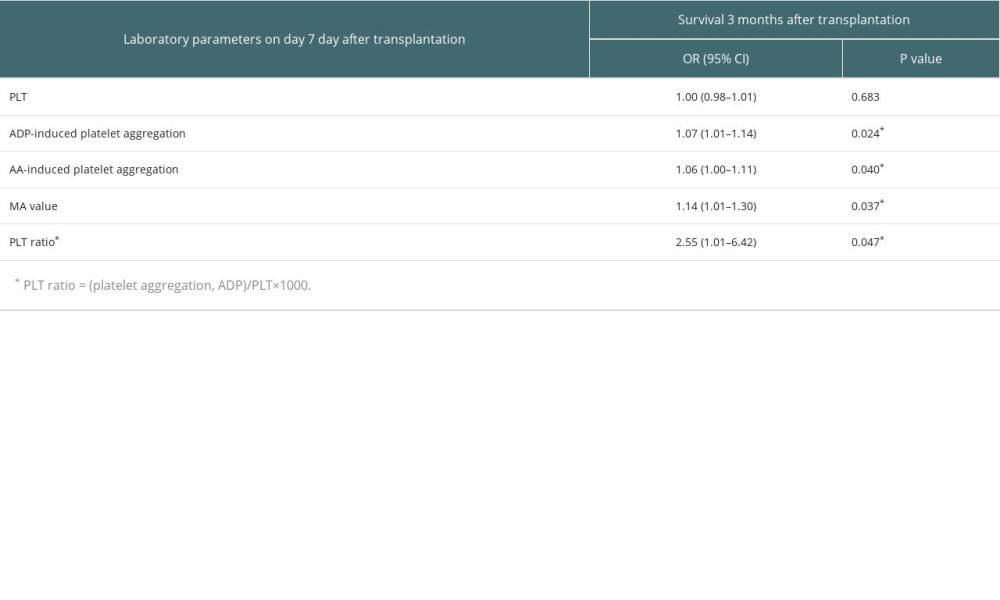 Table 6. Multivariate logistic regression analysis of the survival 3 months after transplantation.
Table 6. Multivariate logistic regression analysis of the survival 3 months after transplantation.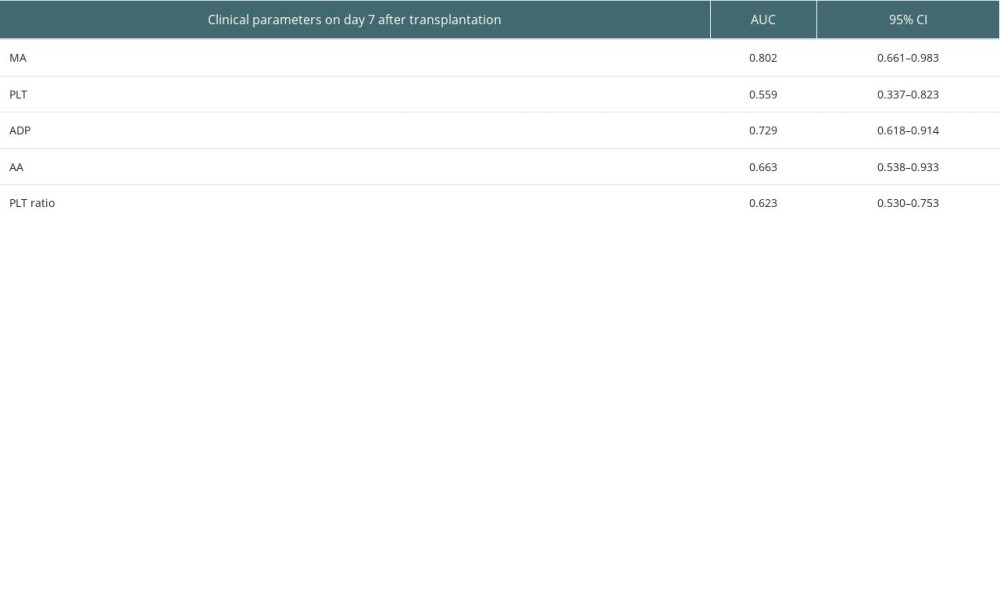 Table 7. Predictive values of PLT, ADP-induced platelet aggregation, AA-induced platelet aggregation and PLT ratio for the survival at 3 months after transplantation.
Table 7. Predictive values of PLT, ADP-induced platelet aggregation, AA-induced platelet aggregation and PLT ratio for the survival at 3 months after transplantation.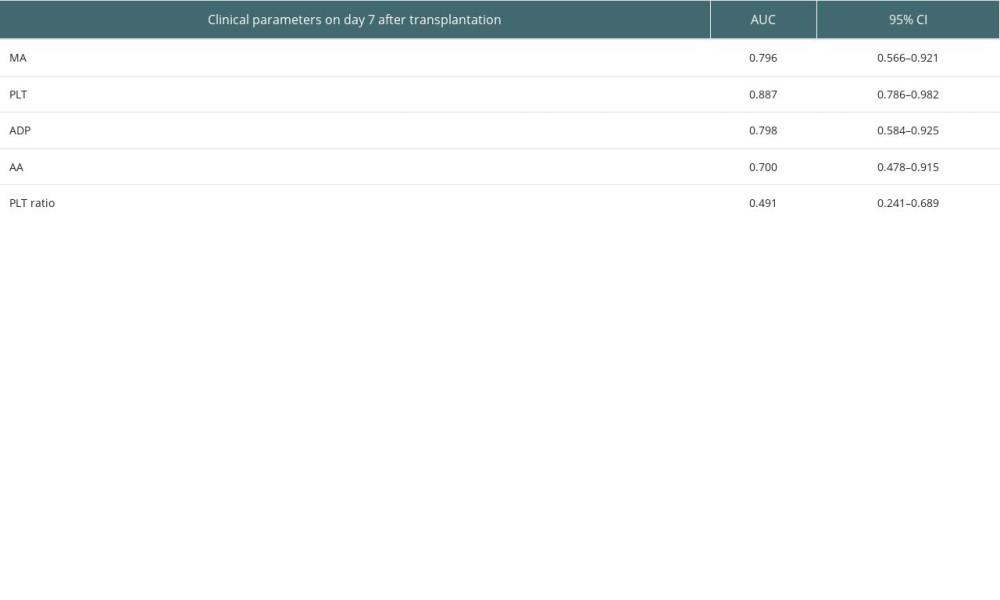 Table 8. Predictive values of MA value, PLT, ADP-induced platelet aggregation, AA-induced platelet aggregation and PLT ratio for the survival at 14 days after transplantation.
Table 8. Predictive values of MA value, PLT, ADP-induced platelet aggregation, AA-induced platelet aggregation and PLT ratio for the survival at 14 days after transplantation.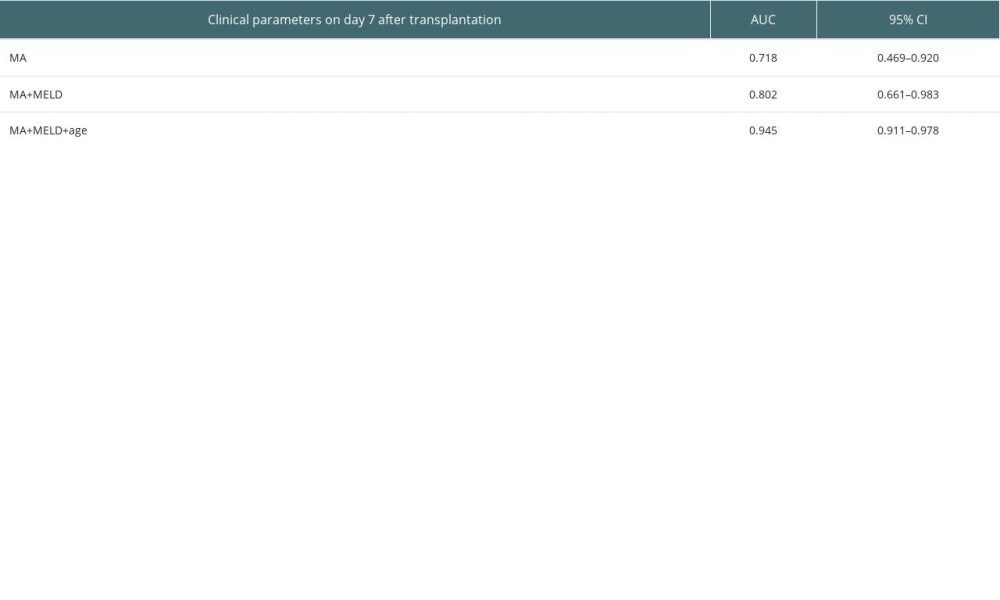 Table 9. Predictive values of MA value, MELD, and age for the survival at 3 months after transplantation.
Table 9. Predictive values of MA value, MELD, and age for the survival at 3 months after transplantation. In Press
20 Mar 2024 : Original article
Transplant Nephrectomy: A Comparative Study of Timing and Techniques in a Single InstitutionAnn Transplant In Press; DOI: 10.12659/AOT.942252
28 Mar 2024 : Original article
Association Between FEV₁ Decline Rate and Mortality in Long-Term Follow-Up of a 21-Patient Pilot Clinical T...Ann Transplant In Press; DOI: 10.12659/AOT.942823
02 Apr 2024 : Original article
Liver Transplantation from Brain-Dead Donors with Hepatitis B or C in South Korea: A 2014-2020 Korean Organ...Ann Transplant In Press; DOI: 10.12659/AOT.943588
02 Apr 2024 : Original article
Effect of Dexmedetomidine Combined with Remifentanil on Emergence Agitation During Awakening from Sevoflura...Ann Transplant In Press; DOI: 10.12659/AOT.943281
Most Viewed Current Articles
05 Apr 2022 : Original article
Impact of Statins on Hepatocellular Carcinoma Recurrence After Living-Donor Liver TransplantationDOI :10.12659/AOT.935604
Ann Transplant 2022; 27:e935604
12 Jan 2022 : Original article
Risk Factors for Developing BK Virus-Associated Nephropathy: A Single-Center Retrospective Cohort Study of ...DOI :10.12659/AOT.934738
Ann Transplant 2022; 27:e934738
22 Nov 2022 : Original article
Long-Term Effects of Everolimus-Facilitated Tacrolimus Reduction in Living-Donor Liver Transplant Recipient...DOI :10.12659/AOT.937988
Ann Transplant 2022; 27:e937988
15 Mar 2022 : Case report
Combined Liver, Pancreas-Duodenum, and Kidney Transplantation for Patients with Hepatitis B Cirrhosis, Urem...DOI :10.12659/AOT.935860
Ann Transplant 2022; 27:e935860








