24 October 2023: Original Paper
Naples Prognostic Score for Graft Functions After Renal Transplantation: A Retrospective Analysis
İsmail Aytaç1ABCDEFG, Betül Güven Aytaç1ABCDEFG*, Oya Kilci1ABCDEFG, Erkan Ölçücüoğlu2ABCDEFGDOI: 10.12659/AOT.942007
Ann Transplant 2023; 28:e942007
Abstract
BACKGROUND: The Naples prognostic score is a comprehensive measure of patients’ inflammation and nutritional status, consisting of serum albumin, total cholesterol, neutrophil/lymphocyte ratio (NLR), and lymphocyte/monocyte ratio (LMR). We compared the Naples prognostic scores of kidney transplant patients with a creatinine reduction ratio of less than 30% vs those with greater than 30%.
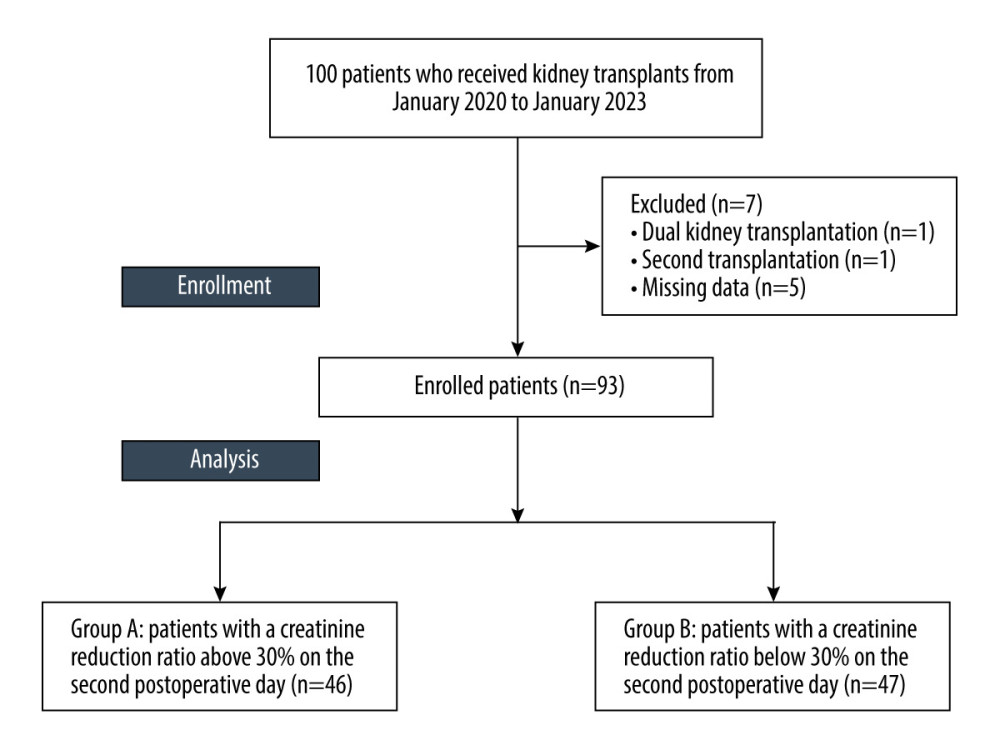
MATERIAL AND METHODS: We conducted a retrospective study on 93 patients who received kidney transplants at our hospital from January 2020 to January 2023. Naples prognostic scores were used to calculate the preoperative condition of transplant recipients. The patients were divided into 2 groups based on their creatinine reduction ratio on the second day after surgery. Group A consisted of patients with a ratio above 30%, while group B consisted of those with a ratio below 30%.
RESULTS: Our analysis revealed that the total cholesterol and albumin values of groups A and B showed no substantial difference. Group B had clearly more patients with Naples prognostic score 3-4 compared to the other group (P=0.032). Multivariate analysis determined that patients with Naples prognostic score 3-4 had a 3.151-fold higher likelihood of experiencing creatinine reduction below 30% (95% CI 1.209-8.215, P value 0.019).
CONCLUSIONS: The preoperative inflammatory and nutritional status of patients may have an impact on the functioning of grafts during the postoperative period. A high Naples prognostic score may be linked with a decrease in creatinine reduction ratio in post-transplant kidneys, which could lead to graft dysfunction.
Keywords: Graft Survival, Kidney Transplantation, Protein-Energy Malnutrition, Humans, Retrospective Studies, Prognosis, Creatinine, Cholesterol
Background
Kidney transplantations, the criterion standard treatment for end-stage renal disease, are increasingly common worldwide. The most concerning issues with graft function are impairment, acute rejection, and subsequent complications. The factors that affect graft function have been studied for years. The quality of the transplanted kidney, recipient age, primary disease, HLA compatibility, ethnic background, and dialysis time were preoperative factors affecting graft function, and delayed graft function, creatinine decrease ratio, chronic allogeneic dysfunction, and immunosuppressant drugs were also associated with graft function [1]. Based on the available literature, monitoring graft function after transplantation can help predict prognosis in the early period by observing the gradual decrease in creatine values compared to their initial levels. Rodrigo et al and Govani et al previously used creatinine reduction ratio to classify graft function, showing that grafts with less than a 10% decrease in creatine on the first postoperative day or less than a 30% decrease on the second day may lead to graft dysfunction within 1 year [2–4].
Individuals with chronic kidney disease (CKD) frequently experience systemic inflammation and concurrent protein-energy malnutrition [5]. The inflammation-malnutrition status of patients who undergo renal transplantation can lead to post-transplant complications, resulting in a dysfunctional graft and increased mortality.
The hypothesis of this study is that monitoring the inflammatory and malnutrition status of patients with alternative scoring systems used in the literature before transplantation surgery may be useful in predicting possible complications. In clinical practice, there are various scoring systems that are utilized, and there is ongoing debate regarding their effectiveness.
The Naples prognostic score (NPS), which measures inflammatory and nutritional parameters, is often utilized to predict cancer patient prognosis [6–9]. NPS was first described as a new prognostic scoring system for colorectal cancer by Galizia et al [10]. The NPS is a comprehensive measure of patients’ inflammation and nutritional status, consisting of serum albumin, total cholesterol, neutrophil/lymphocyte ratio (NLR), and lymphocyte/monocyte ratio (LMR). Studies have shown that it can accurately predict the prognosis of patients with myocardial infarction and congestive heart failure and identify malnutrition in hypertensive patients, acute renal failure following a myocardial infarction, and postoperative complications after diverticulitis [11–15].
The CONUT score, calculated from serum albumin, total lymphocyte counts, and total cholesterol concentration, is a biomarker used to predict survival in cancer patients. A high CONUT score is associated with lower levels of albumin, lymphocytes, and cholesterol, which may indicate poor nutritional and immune status in patients, and could lead to decreased survival rates [16].
The systemic inflammation score (SIS), based on preoperative albumin level and LMR, is a strong prognostic marker for clear cell renal cell carcinoma and colorectal cancer [17,18]. The scoring systems are commonly used in the medical literature, primarily for cancer patients. They can also predict the likelihood of complications and mortality after a transplant.
Our study aimed to compare kidney transplant patients with a creatinine reduction ratio of less than 30% vs greater than 30% in terms of the prognostic scores.
Material and Methods
STATISTICAL ANALYSIS:
We used IBM SPSS version 20 software from Chicago, Illinois, USA for the evaluations. For continuous data, the descriptive statistics provided were the mean, standard deviation, median, minimum, and maximum values. To test for normal distribution of continuous data, we used the Shapiro-Wilk test. To express continuous variables, medians and interquartile ranges (IQR) were used. When the data had a normal distribution, we used the
In assessing creatinine reduction ratio, we assessed the usefulness of the NPS scoring method using ROC curve analysis. Area under the curve (AUC) values provided clarity in analyzing the results. The cut-off value was determined based on the Youden index calculation. We used multivariate logistic regression analysis to examine the correlation between NPS and creatinine reduction ratio. Regression analysis results are presented as odds ratio (OR) and a 95% confidence interval, with statistical significance defined as
SAMPLE SIZE ESTIMATION:
According to Hogendorf et al, 26.7% of adult cadaveric donor renal transplant recipients had an EGFR value higher than 30% [21]. We calculated that at least 82 kidney transplant patients should be included with a 15% difference rate assumption using the “Proportion: One group: Difference from constant” test, d=0.15 effect size, 80% power, and 0.05 error level. The calculation was performed using the “GPower 3.1.9.2” package.
Results
The study involved 100 patients who had kidney transplant surgery. One patient received a dual kidney transplant, another received a second kidney transplant, and data for 5 patients were unavailable; therefore, 7 patients were excluded from the study, leaving 93 patients for analysis (Figure 1). Table 2 presents the demographic and preoperative information of patients. Out of all patients, 73.1% received a transplant from a living donor, while 27.9% received a transplant from a cadaver. In 51% of patients, the rate of reduction in creatinine was below 30%. Out of 93 patients, 63 (67.7%) had NPS scores of 0–2 and 30 (32.2%) had NPS scores of 3–4. The average lymphocyte count was 1.72±0.6/mm3, while the average neutrophil count was 4.36±2.02/mm3. Additionally, the mean albumin was 41.9±4.9 mg/dL, and the mean total cholesterol was 168.2±52.3 mg/dL.
Based on the data from our study, there were 4 cases of patient exitus and 1 case of myocardial infarction and all of these patients experienced acute rejection.
No significant difference was found when comparing the age, height, weight, BMI values, duration of dialysis, sex distribution, and additional disease rates between patients in group A and group B (
No significant differences were discovered in terms of operation times, warm ischemia time, and cold ischemia times when comparing patients from group A and group B (
After analyzing the preoperative hemogram and biochemistry values of patients in groups A and B, we found no variations in the levels of hemoglobin, lymphocytes, monocytes, platelets, creatinine, albumin, and PLR (
The comparison between group A and group B showed no significant difference in terms of total cholesterol and albumin values. However, the number of patients with NPS 3–4 was significantly higher in group B (
The cut-off values for patients with a creatinine reduction ratio less than 30% are presented in Table 3. The values of potent markers were determined by maximizing the Youden index, which takes into account the sensitivity and specificity of the test. To establish the cut-off values for albumin, total cholesterol, NLR, and LMR, the ROC curve was utilized.
Multivariate analysis showed that patients with NPS 3–4 had a 3.151-fold higher likelihood of experiencing creatinine reduction below 30% (95% CI 1.209–8.215,
Discussion
The nutritional and inflammatory status of a patient, along with other factors related to the preoperative process, can have an impact on the function of a transplanted graft after surgery [22,23]. Finding an objective and easily applicable criterion in the preoperative period to detect inflammatory and nutritional status is a crucial issue. After reviewing the literature, it is evident that many studies have explored different prognostic indicators and scoring systems related to inflammation and nutrition. It is important to note that no single marker of inflammation or nutrition can provide a complete representation of a patient’s overall condition. The NPS scoring system does not have a single marker that can be used as an independent prognostic factor. This indicates that a marker with limited predictive ability cannot be applied to a wide variety of cases. To evaluate the prognosis of patients, several scoring systems have been developed, which incorporate various parameters like NPS, CONUT, and SIS [8,10,18,24]. These systems have been increasingly used in recent years.
Research studies have found that patients who experience lower-than-expected reductions in creatinine levels after a transplant may be at risk for delayed graft function [2,25,26]. Our study aimed to determine the various factors that impact the creatinine reduction ratio, which serves as a predictor of graft function.
We conducted a retrospective analysis of 93 renal transplantation patients who were treated at our hospital. Out of these patients, 51% had a creatinine decrease rate of less than 30% on the 2nd day, while the remaining 49% had a creatinine decrease rate of over 30% on the same day.
We calculated the NPS based on the preoperative complete blood count and biochemistry results of the patients. We found that patients with a creatinine reduction ratio below 30% had a significantly higher rate of NPS 3–4, significantly higher levels of neutrophil and NLR, and significantly lower levels of LMR (
Aa study on kidney transplant patients by Halper et al found that patients with delayed graft function had significantly higher NLR and PLR values [27]. Naranjo et al observed that patients with acute graft rejection had significantly higher preoperative NLR and PLR values [23]. A study conducted by Baral et al found that for patients who received kidney transplants from cadaveric donors, the recipient’s preoperative NLR and PLR levels can predict development of delayed graft function, and also revealed that NLR is a more effective predictor than PLR. Multivariate analysis showed that NLR exceeding 3.5 and PLR exceeding 120 were independently responsible for delayed graft function [28]. In our research, we observed that patients with creatine reduction ratio <30% had elevated preoperative NLR values. This finding was consistent with previous studies conducted on the same topic. We did not observe a significant variation in PLR values during our study, which could be due to the inclusion of both living and cadaveric donors for kidney transplantation.
Patients who received a kidney transplant from a living donor and had delayed kidney function showed noticeably higher preoperative NLR values, according to a study conducted by Halazun et al [29]. Ergin et al conducted a study showing that kidney transplant patients with acute graft rejection had notably higher preoperative NLR values [30]. Research conducted on patients who underwent organ transplants (eg, kidney and liver) has also confirmed the relationship between low graft function and elevated NLR values, which agrees with the findings of our study. Our study confirms the correlation with the cut-off values of NLR detected in other studies.
Inflammation has become an increasingly recognized risk factor for malnutrition. Inflammatory signals can significantly hinder the synthesis of visceral protein, which has led to discussions about using these proteins as biomarkers of nutritional status. This is because inflammation strongly influences these proteins, which are less affected by protein-energy stores. In conclusion, laboratory markers can complement a comprehensive physical examination [31].
In their study, Molnar et al found that the MIS, a straightforward tool for assessing the malnutrition-inflammation complex syndrome, can predict mortality in kidney transplant recipients [32]. Djukanovic et al found a correlation between malnutrition and negative outcomes for patients who underwent renal transplantation, in which patients who experienced malnutrition had a higher risk of graft failure and poor prognosis [33]. Santos et al found that patients who had higher malnutrition risk scores had worse outcomes and allograft survival. Being able to predict short-term outcomes in kidney transplantation is beneficial in anticipating long-term outcomes and minimizing the requirement for re-transplantation [34]. According to Tutal et al’s research, individuals who have received a renal transplant may experience malnutrition at an early stage due to a decrease in muscle and fat mass. This decrease is strongly associated with a lack of increase in GFR [35]. According to a study by Eckart et al, albumin is not just an indicator of nutritional status, but is also a negative acute-phase protein, indicating that it may also reflect the severity of inflammation or acute disease, rather than just nutritional status alone [36]. According to Evans et al, serum albumin and prealbumin are not reliable indicators of total body protein or nutrition. They found that these proteins are negative acute-phase reactants that can lead to negative outcomes in patients, rather than being indicators of protein-energy malnutrition [37].
In our study, we did not find a significant difference in the albumin values of our patients, which we used as a nutritional marker. The literature indicates that it is now increasingly important to assess inflammation and malnutrition together.
According to Galizia et al, the NPS is a straightforward tool that is highly correlated with long-term results for individuals receiving surgery for colorectal cancer [10].
In their research, Peng et al found that NPS can be a useful predictor for overall survey and progression-free survival in non-small cell lung cancer patients, regardless of their TNM stage [8].
Our findings align with previous research indicating that a patient’s nutritional and inflammatory state plays a significant role in the prognosis and monitoring of the graft. It was observed that using scoring systems was more effective than relying on a single parameter, and the NPS was found to be more effective than CONUT and SIS. A strength of the present study is that it utilized the NPS scoring system to assess prognosis in individuals with cancer and diverse heart conditions, and our study was the first to investigate the correlation with creatinine reduction ratio. During the preoperative examination, it is crucial to ensure that NPS can be easily applied. If possible, prehabilitation should be conducted before the operation to prepare the patient, which can help reduce the occurrence of postoperative complications.
There were limitations in our study, such as not differentiating between cadaveric and living donors when analyzing patients. Variable cold ischemia times and graft quality can be confounding factors in cadaveric donors. It is necessary to conduct studies that differentiate between different types of donors. Furthermore, our study was restricted to patients with a 1-year follow-up, which is another limitation. Conducting longer follow-ups could have enabled us to observe any alterations in the graft functions of the patients. It is important to conduct additional studies that involve a larger number of patients and assess long-term graft function to obtain more conclusive results.
Conclusions
To ensure the best outcomes for patients, it is important for the transplant team to work together and actively reduce any potential complications or risks following surgery. This collaborative effort can ultimately help to increase patient survival rates and promote overall wellness. Addressing preoperative assessment, intraoperative management, and postoperative care is vital for the whole team to ensure the best possible outcome. The preoperative inflammatory and nutritional status of patients may have an impact on the functioning of grafts during the postoperative period. Our study found that patients with a post-transplant kidney creatinine reduction ratio below 30% had higher NPS scores. Previous studies suggest that those with less than 30% reduction may experience graft dysfunction. Detailed scoring systems that consider various indicators can be useful in identifying patients who may be at risk of post-transplant complications and mortality. By using these systems prior to surgery, patients can be better prepared and transplantation can be performed more safely.
References
1. Legendre C, Canaud G, Martinez F, Factors influencing long-term outcome after kidney transplantation: Transpl Int, 2014; 27(1); 19-27
2. Govani MV, Kwon O, Batiuk TD, Creatinine reduction ratio and 24-hour creatinine excretion on posttransplant day two: Simple and objective tools to define graft function: J Am Soc Nephrol, 2002; 13(6); 1645-49
3. Rodrigo E, Ruiz JC, Piñera C, Creatinine reduction ratio on post-transplant day two as criterion in defining delayed graft function: Am J Transplant, 2004; 4(7); 1163-69
4. Maraghi E, Rahimi Foroushani A, Younespour S, Longitudinal assessment of serum creatinine levels on graft survival after renal transplantation: Joint modeling approach: Nephrourol Mon, 2016; 8(4); e37666
5. Hanna RM, Ghobry L, Wassef O, A practical approach to nutrition, protein-energy wasting, sarcopenia, and cachexia in patients with chronic kidney disease: Blood Purif, 2020; 49(1–2); 202-11
6. Chen F, Xie C, Ren K, Xu X, Prognostic value of the naples prognostic score in patients with gastrointestinal cancers: A meta-analysis: Nutr Cancer, 2023; 75(7); 1520-30
7. Li J, Yang W, Yuan Y, Preoperative Naples prognostic score is a reliable prognostic indicator for newly diagnosed glioblastoma patients: Front Oncol, 2022; 12; 775430
8. Peng S-M, Ren J-J, Yu N, The prognostic value of the Naples prognostic score for patients with non-small-cell lung cancer: Sci Rep, 2022; 12(1); 5782
9. Li Q, Cong R, Wang Y, Naples prognostic score is an independent prognostic factor in patients with operable endometrial cancer: results from a retrospective cohort study: Gynecol Oncol, 2021; 160(1); 91-98
10. Galizia G, Lieto E, Auricchio A, Naples prognostic score, based on nutritional and inflammatory status, is an independent predictor of long-term outcome in patients undergoing surgery for colorectal cancer: Dis Colon Rectum, 2017; 60(12); 1273-84
11. Russell B, Zager Y, Mullin G, Naples prognostic score to predict postoperative complications after colectomy for diverticulitis: Am Surg, 2023; 89(5); 1598-604
12. Karakoyun S, Cagdas M, Celik AI, Predictive value of the Naples prognostic score for acute kidney injury in ST-elevation myocardial infarction patients undergoing primary percutaneous coronary intervention: Angiology, 2023 Online ahead of print
13. Erdogan A, Genc O, Inan D, Impact of Naples Prognostic Score on midterm all-cause mortality in patients with decompensated heart failure: Biomark Med, 2023; 17(4); 219-30
14. Yang Z-w, Wei X-b, Fu B-q, Prevalence and prognostic significance of malnutrition in hypertensive patients in a community setting: Front Nutr, 2022; 9; 822376
15. Erdogan A, Genc O, Ozkan E, Impact of Naples Prognostic Score at admission on in-hospital and follow-up outcomes among patients with ST-segment elevation myocardial infarction: Angiology, 2023 Online ahead of print
16. Toyokawa T, Kubo N, Tamura T, The pretreatment Controlling Nutritional Status (CONUT) score is an independent prognostic factor in patients with resectable thoracic esophageal squamous cell carcinoma: Results from a retrospective study: BMC Cancer, 2016; 16(1); 1-11
17. Zheng R-r, Huang M, Jin C, Cervical cancer systemic inflammation score: A novel predictor of prognosis: Oncotarget, 2016; 7(12); 15230
18. Suzuki T, Ishibashi Y, Tsujimoto H, A novel systemic inflammatory score combined with immunoinflammatory markers accurately reflects prognosis in patients with esophageal cancer: In Vivo, 2020; 34(6); 3705-11
19. Fu X, Li T, Dai Y, Li J, Preoperative systemic inflammation score (SIS) is superior to neutrophil to lymphocyte ratio (NLR) as a predicting indicator in patients with esophageal squamous cell carcinoma: BMC cancer, 2019; 19(1); 1-10
20. Ignacio de Ulíbarri J, González-Madroño A, de Villar NG, CONUT: A tool for controlling nutritional status. First validation in a hospital population: Nutr Hosp, 2005; 20(1); 38-45
21. Hogendorf P, Suska A, Skulimowski A, Neutrophil-lymphocyte ratio and creatinine reduction ratio predict good early graft function among adult cadaveric donor renal transplant recipients. Single institution series: Pol Przegl Chir, 2018; 90(2); 28-33
22. Betjes MG, Immune cell dysfunction and inflammation in end-stage renal disease: Nat Rev Nephrol, 2013; 9(5); 255-65
23. Naranjo M, Agrawal A, Goyal A, Rangaswami J, Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio predict acute cellular rejection in the kidney allograft: Ann Transplant, 2018; 23; 467-74
24. Suzuki Y, Okabayashi K, Hasegawa H, Comparison of preoperative inflammation-based prognostic scores in patients with colorectal cancer: Ann Surg, 2018; 267(3); 527-31
25. Vilar E, Varagunam M, Yaqoob MM, Creatinine reduction ratio: A useful marker to identify medium and high-risk renal transplants: Transplantation, 2010; 89(1); 97-103
26. Hariharan S, Mcbride MA, Cherikh WS, Post-transplant renal function in the first year predicts long-term kidney transplant survival: Kidney Int, 2002; 62(1); 311-18
27. Halpern SE, Moris D, Shaw BI, The systemic immune-inflammation index predicts clinical outcomes in kidney transplant recipients: In Vivo, 2020; 34(6); 3349-60
28. Baral D, Yang Y, Katwal G, Recipient pre-operative neutrophil lymphocyte ratio better predicts delayed graft function than platelet lymphocyte ratio in donation after brain death kidney transplantation: Medical Journal of Pokhara Academy of Health Sciences, 2019; 2(2); 209-16
29. Halazun K, Marangoni G, Hakeem A, Elevated preoperative recipient neutrophil-lymphocyte ratio is associated with delayed graft function following kidney transplantation: Transplant Proc, 2013; 45(9); 3254-57
30. Ergin G, Değer SM, Köprü B, High neutrophil-to-lymphocyte ratio predicts acute allograft rejection in kidney transplantation: A retrospective study: Turk J Med Sci, 2019; 49(2); 525-30
31. Keller U, Nutritional laboratory markers in malnutrition: J Clin Med, 2019; 8(6); 775
32. Molnar MZ, Czira ME, Rudas A, Association of the malnutrition-inflammation score with clinical outcomes in kidney transplant recipients: Am J Kidney Dis, 2011; 58(1); 101-8
33. Djukanović L, Ležaić V, Blagojević R, Co-morbidity and kidney graft failure – two main causes of malnutrition in kidney transplant patients: Nephrol Dial Transplant, 2003; 18(Suppl 5); v68-v70
34. Santos MRO, Lasmar MF, Nascimento E, Fabreti-Oliveira RA, Impact of pretransplantation malnutrition risk on the clinical outcome and graft survival of kidney transplant patients: J Bras Nefrol, 2023 Online ahead of print
35. Tutal E, Sezer S, Uyar ME, Evaluation of nutritional status in renal transplant recipients in accordance with changes in graft function: Transplant Proc, 2013; 45(4); 1418-22
36. Eckart A, Struja T, Kutz A, Relationship of nutritional status, inflammation, and serum albumin levels during acute illness: A prospective study: Am J Med, 2020; 133(6); 713-22e7
37. Evans DC, Corkins MR, Malone A, The use of visceral proteins as nutrition markers: an ASPEN position paper: Nutr Clin Pract, 2021; 36(1); 22-28
Tables
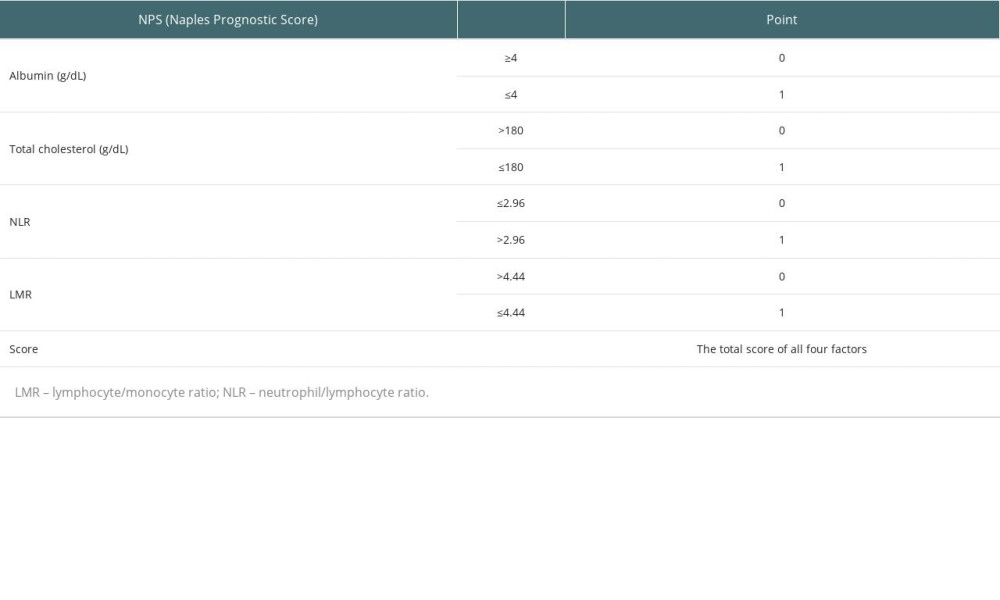 Table 1. Naples Prognostic Score.
Table 1. Naples Prognostic Score.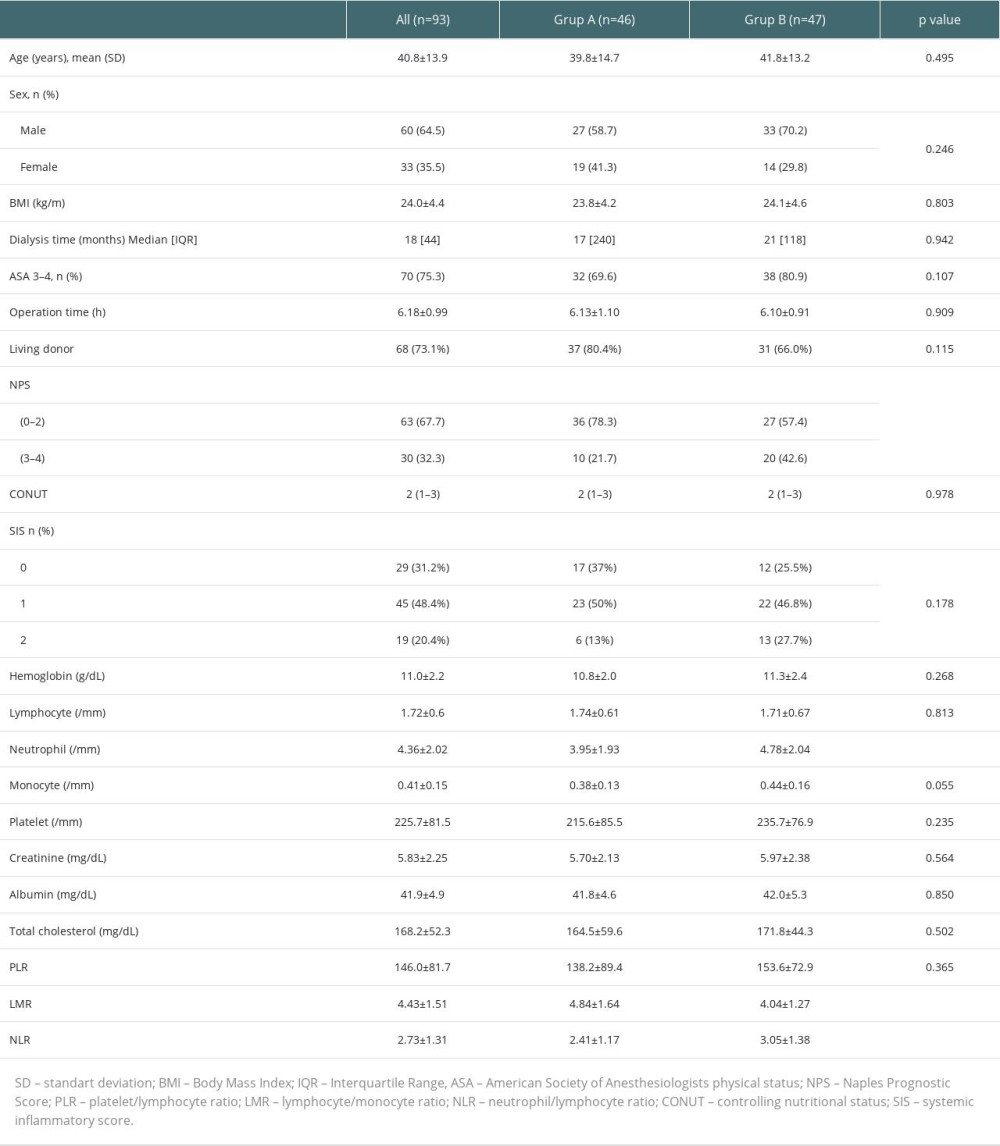 Table 2. Baseline demographic and clinical characteristics of patients.
Table 2. Baseline demographic and clinical characteristics of patients.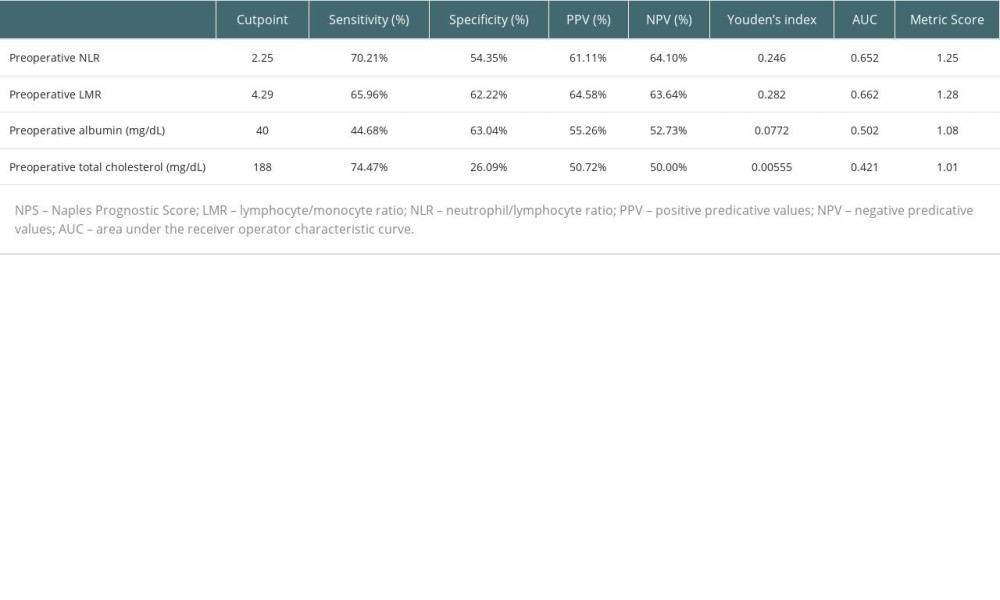 Table 3. The optimal cut-off values of NPS components for creatinine reduction ratio below 30%.
Table 3. The optimal cut-off values of NPS components for creatinine reduction ratio below 30%.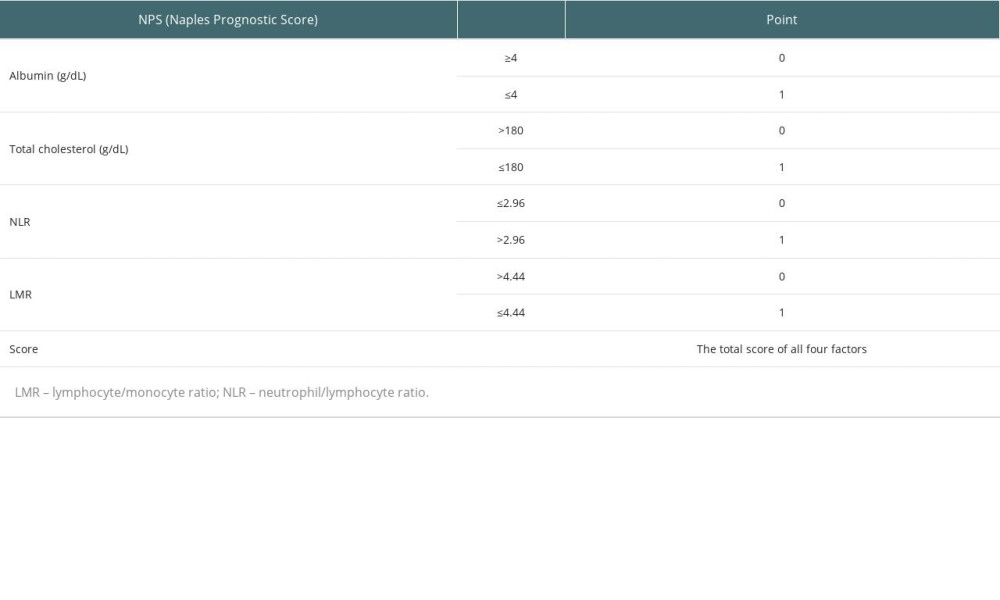 Table 1. Naples Prognostic Score.
Table 1. Naples Prognostic Score.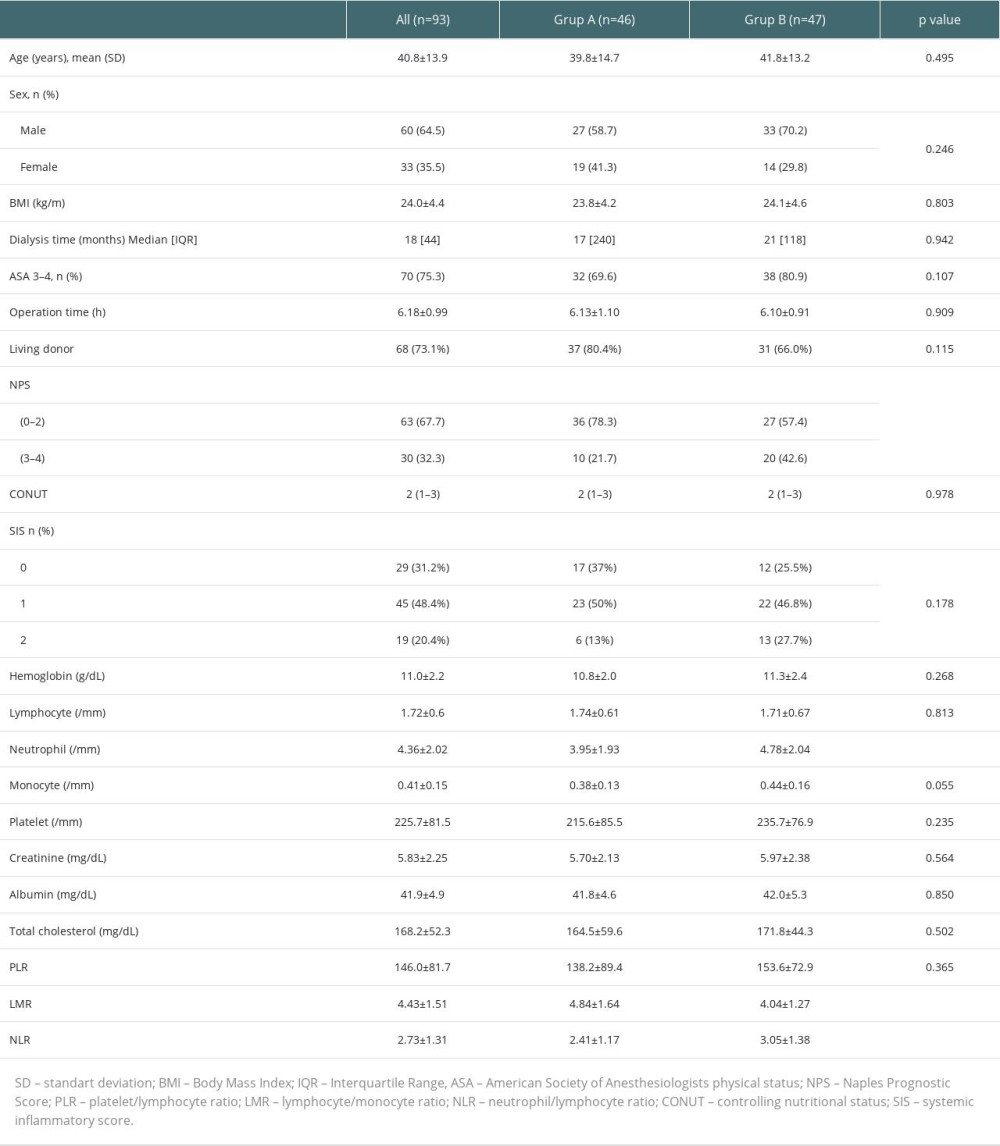 Table 2. Baseline demographic and clinical characteristics of patients.
Table 2. Baseline demographic and clinical characteristics of patients.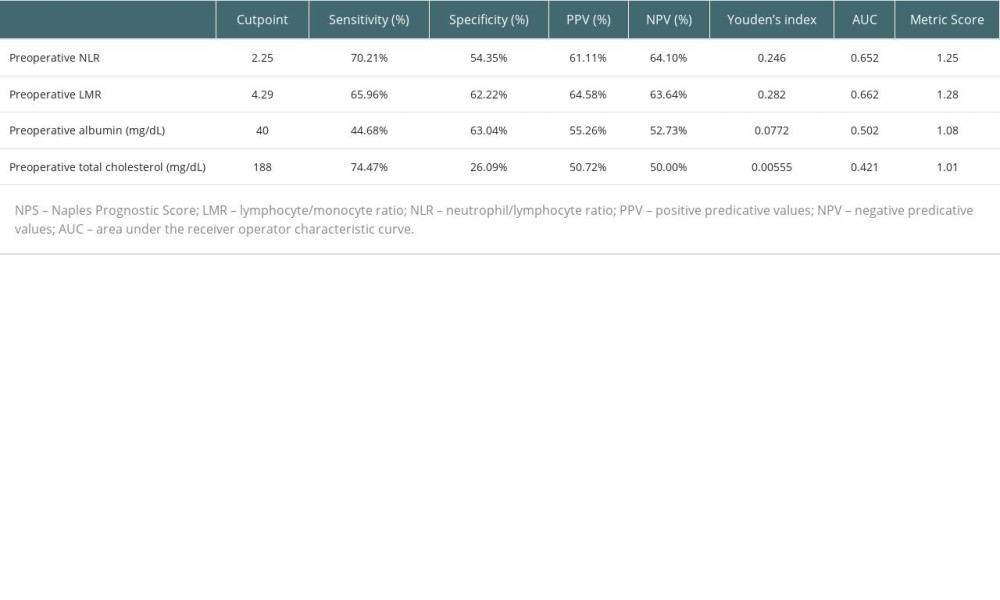 Table 3. The optimal cut-off values of NPS components for creatinine reduction ratio below 30%.
Table 3. The optimal cut-off values of NPS components for creatinine reduction ratio below 30%. In Press
20 Mar 2024 : Original article
Transplant Nephrectomy: A Comparative Study of Timing and Techniques in a Single InstitutionAnn Transplant In Press; DOI: 10.12659/AOT.942252
28 Mar 2024 : Original article
Association Between FEV₁ Decline Rate and Mortality in Long-Term Follow-Up of a 21-Patient Pilot Clinical T...Ann Transplant In Press; DOI: 10.12659/AOT.942823
02 Apr 2024 : Original article
Liver Transplantation from Brain-Dead Donors with Hepatitis B or C in South Korea: A 2014-2020 Korean Organ...Ann Transplant In Press; DOI: 10.12659/AOT.943588
02 Apr 2024 : Original article
Effect of Dexmedetomidine Combined with Remifentanil on Emergence Agitation During Awakening from Sevoflura...Ann Transplant In Press; DOI: 10.12659/AOT.943281
Most Viewed Current Articles
05 Apr 2022 : Original article
Impact of Statins on Hepatocellular Carcinoma Recurrence After Living-Donor Liver TransplantationDOI :10.12659/AOT.935604
Ann Transplant 2022; 27:e935604
12 Jan 2022 : Original article
Risk Factors for Developing BK Virus-Associated Nephropathy: A Single-Center Retrospective Cohort Study of ...DOI :10.12659/AOT.934738
Ann Transplant 2022; 27:e934738
22 Nov 2022 : Original article
Long-Term Effects of Everolimus-Facilitated Tacrolimus Reduction in Living-Donor Liver Transplant Recipient...DOI :10.12659/AOT.937988
Ann Transplant 2022; 27:e937988
15 Mar 2022 : Case report
Combined Liver, Pancreas-Duodenum, and Kidney Transplantation for Patients with Hepatitis B Cirrhosis, Urem...DOI :10.12659/AOT.935860
Ann Transplant 2022; 27:e935860