06 December 2022: Original Paper
Changes in Physical Activity Due to Fear of COVID-19 and Its Impact on Depression Among Post-Liver Transplant Patients in Japan: A Longitudinal Survey Study
Satomi TanakaDOI: 10.12659/AOT.938239
Ann Transplant 2022; 27:e938239
Abstract
BACKGROUND: Regular physical activity (PA) is important for maintaining mental and physical health after liver transplantation (LT); however, the fluctuations in routine PA during COVID-19 and its putative impacts are currently unknown. This study examined the changes in PA during the COVID-19 pandemic and explored its association with fear and depression during the pandemic.
MATERIAL AND METHODS: This longitudinal study included 83 LT patients whose PA was measured using the short form of the International Physical Activity Questionnaire before and during COVID-19. Fear of COVID-19 was estimated based on previous studies, and depression was assessed using the Patient Health Questionnaire-9. Participants were also asked about important sources of information on COVID-19. PA was classified as inactive or active depending on the changes in PA, and logistic regression analyses with PA as a dependent variable were conducted to explore the associations among PA, depression, and fear of COVID-19.
RESULTS: Moderate and high PA exhibited decreasing trends before and during the COVID-19 pandemic, especially in males. Fear of being infected with SARS-CoV-2, the virus that causes COVID-19, while shopping was significantly higher in females and was significantly independent of inactivity during the COVID-19 pandemic. Only 1 patient reported that their transplant center was their main source of information about COVID-19. Only 4.9% of the LT participants were depressed.
CONCLUSIONS: Our study results indicate the need to support the provision of accurate information about COVID-19 by health care professionals in transplant centers, especially for patients with low PA, to prevent PA decline in LT patients.
Keywords: COVID-19, Depression, Physical activity, Fear, Liver Transplantation, Male, Female, Humans, Pandemics, SARS-CoV-2, Longitudinal Studies, Japan, Exercise, Surveys and Questionnaires
Background
The five-year survival rate after liver transplantation (LT) reached 75% in 2019 owing to advancements in surgical techniques and improved immunosuppressants [1]. However, LT patients are considered at high risk of developing coronavirus disease 2019 (COVID-19), and experience severe symptoms owing to continued use of immunosuppressants and blunted immune response to vaccination [2,3]. A review of COVID-19 and organ transplant patients after transplant reported that the mortality rate of post-transplant patients infected with SARS-CoV-2, the virus that causes COVID-19, is 13–30%, which is higher than the mortality rate of 12.5% in the general population [4–6].
Physical activity (PA) after LT is effective in preventing the onset and severity of metabolic syndrome, including hypertension and obesity, which are long-term post-transplant complications, and improving physical function and quality of life (QOL) [7–9]. A study on PA and depression in kidney transplant recipients 6 years after transplant revealed that higher PA levels were associated with a lower risk of depression [10]. Therefore, promoting PA after organ transplantation is important to maintain patients’ mental and physical health.
A study on the PA of the general Japanese population before, during, and after COVID-19 was declared an emergency showed that total PA (TPA) in the general population was 15–32% lower than before its onset [11]. A systematic review reported that PA decreased during the COVID-19 pandemic among the general population as well as among diabetes and heart failure patients, for whom PA is highly recommended [12,13]. There are concerns regarding COVID-19 associated hindrances in execution of PA in post-LT patients; however, the changes in PA during the COVID-19 pandemic in this population are still unknown.
Although mental QOL improves in the long term after LT [14], depression may be higher in post-LT patients as they are a COVID-19-vulnerable population. Systematic reviews have shown that depression after organ transplantation increases the risk of mortality and graft dysfunction by 65% [15]; therefore, prevention of depression after transplantation is an important postoperative issue. A review on mental health during the COVID-19 pandemic reported that patients with chronic diseases such as diabetes have higher levels of depression and anxiety than those with non-chronic diseases [16]. Studies indicated that PA was a predictor of depression in the general population during the COVID-19 pandemic [17] and that the promotion of moderate-to-vigorous PA reduced depression by 12–32% [18]. However, the relationship between depression associated with the COVID-19 pandemic and PA in post-LT patients has not been clarified yet.
A moderate level of fear of COVID-19 has a positive effect by promoting infection-preventive public health behaviors, such as hand washing and social distance, whereas extreme fear causes psychological and physical problems [15]. A study found that post-LT patients in Germany were more fearful of COVID-19 and went out less frequently than their household members, and approximately 40% of patients avoided going out during the COVID-19 pandemic [16].
Systematic reviews evaluating the fear levels of contracting COVID-19 in the general population and healthcare providers have indicated sex-associated differences in their fear levels [17]. A comparative study revealed that females were approximately 3 times more likely to have moderate/higher fear levels of contracting COVID-19 compared with males [18]. In addition, fear of COVID-19 and PA were shown to be negatively correlated [19]. Excessive fear after LT may lead to mental health problems as well as decreased PA and deterioration of the transplanted organ.
This study aimed to: 1) compare PA before and during the COVID-19 pandemic in patients who had undergone LT, 2) identify depression and fear of COVID-19 in post-LT patients, 3) examine sex-specific differences in PA changes, depression, and fear of COVID-19, and 4) explore the relationship between PA during the COVID-19 pandemic, depression, and levels of fear of contracting COVID-19.
Material and Methods
SAMPLING:
This was a longitudinal study. The sample population included 94 patients from the Kyushu University Hospital LT Surgery outpatient department who had their PA measured before the COVID-19 pandemic, from 2016 to 2019. A further 94 individuals were invited to take part in the survey during the pandemic, which was conducted from February to March 2021. During this study period, a state of emergency was declared by the national and prefectural governments. The inclusion criteria were: 1) ≥20 years of age, 2) time since LT ≥6 months, and 3) living at home. The exclusion criteria were having a gait disorder, such as severe arthritis. Self-administered questionnaires and consent forms were distributed to 94 patients who met the eligibility criteria, and 86 patients responded (response rate of 91.5%). Two patients were excluded owing to missing data in the International Physical Activity Questionnaire (IPAQ); therefore, 84 patients were included in the analysis (valid response rate of 89.4%). One of the analyzed patients had missing data in the self-administered questionnaire for the fear of COVID-19. Consequently, 83 patients were analyzed for fear of COVID-19. A sample of 82 patients was calculated to yield an ability to detect a type 2 error of 0.8 and an effect size of 0.3 at the 5% significance level (G*Power, Heinrich-Heine Universität, Düsseldorf, Germany).
This study was approved by the Kyushu University Ethics Review Board (ID: 2020-663). The privacy of the study participants was protected and their personal information was kept confidential. Participants were informed that their participation was voluntary, that it would not affect their treatment, that they could withdraw from the study at any time, and that only the aggregated data would be reported. All participants then provided written informed consent.
PROCEDURE:
LT patients who met the eligibility criteria were informed of the research purpose, ethical considerations, research protocol, and the instructions for the self-administered questionnaire by the first researcher during their outpatient visits in February and March 2021. Participants who agreed to participate completed a written consent form at home after their outpatient visit and answered a self-administered questionnaire. After completing the questionnaire, they mailed the consent form and the questionnaire to the researcher.
PHYSICAL ACTIVITY: PA levels were assessed using the Japanese version of IPAQ short form [20,21]. The IPAQ is a self-administered questionnaire consisting of 7 items, including the duration (minutes) and frequency (days) of 4 PA domains (leisure, domestic and gardening, work, and transport) performed in the preceding week. The PA intensity equivalent for Vigorous PA=8.0 Metabolic equivalents (METs), Moderate PA=4.0 METs, and Walking=3.3 METs. PA (METs/min/week) was calculated as each PA intensity (METs)*duration (minutes)*days. TPA (METs/min/week) was calculated using the sum of PA intensity for vigorous, moderate, and walking. In addition, to classify the population, PA levels were divided into the following 3 categories according to the IPAQ scoring [22]:
In this study, PA was classified into categories by calculating vigorous, moderate, walking time (min/week), and total PA (METs*min/week). Inactive and active groups were categorized based on changes in PA during the pandemic. The inactive group was defined as participants with moderate and high PA before the pandemic and low PA during the pandemic, or participants with low PA both before and during the pandemic. The active group was defined as participants with moderate and high PA before and during the pandemic.
FEAR OF COVID-19: The fear of COVID-19 was evaluated using a 5-point Likert scale (5=agree; 1=disagree) with a 4-item self-administered questionnaire based on Reuken et al [16]. LT patients were asked to choose the 2 most important sources of COVID-19 information among the following 10 options: 1) other transplant patients, 2) Ministry of Health, Labour and Welfare website, 3) lectures on transplants, 4) television, 5) news website, 6) family/friends, 7) newspapers, 8) social networking service, 9) transplant center, and 10) hospitals other than Kyushu University Hospital. In addition, participants were asked if they had ever been diagnosed with COVID-19.
DEPRESSION: The Japanese version of the Patient Health Questionnaire-9 (PHQ-9) was used to assess depression [23]. The PHQ-9 is a 9-item self-administered questionnaire that has been tested for reliability and validity and translated into many languages as a rating scale for depression [24]. The original English version of the PHQ-9 had a Cronbach’s α of 0.89 [25], while our study had a Cronbach’s α of 0.75.
PHQ-9 evaluates the frequency of depressive symptoms over the last week (“not at all,” “several days,” “more than half the day,” “half the day nearly every day,” and “nearly every day”). The level of depression is classified according to the total score: 0–9 (minimal–mild), 10–14 (moderate), 15–19 (moderate–severe), and 20–27 (severe). In the present study, a score of 10 or higher (≥moderate) was used as the cut-off for depression based on the observations obtained from previous studies [26].
PATIENT CHARACTERISTICS:
Clinical and demographic characteristics of patients were collected from medical records. Body mass index (BMI) was calculated using the patient’s height and weight measurement data before the pandemic, although self-reported data were evaluated during the pandemic. Patients were asked questions about their exercising habits only during the pandemic.
STATISTICAL ANALYSIS:
After calculating descriptive statistics, PA categories were classified into 2 groups: low and moderate-and-high. Mann-Whitney U and chi-square tests were used to compare the PA changes, medical and demographic attributes, fear of contracting the virus, and sex differences before and during the pandemic.
Mann-Whitney U and chi-square tests were used to compare fear of COVID-19, depression, and demographic characteristics in inactive and active groups. In addition, logistic regression analyses were conducted with inactive and active groups during the pandemic as dependent variables to examine the association between PA, fear of COVID-19, and depression. The independent variables included: fear of COVID-19, which was significant in the univariate analysis, and presence of depression, sex, age, and BMI, among the known factors associated with PA. We used BMI before the pandemic because BMI during the pandemic was self-reported.
All statistical analyses were conducted using SPSS Ver. 27 (IBM Corp., Armonk, NY, USA), and
Results
SAMPLING:
Table 1 shows the demographic and clinical characteristics of the participants before and during the pandemic. The mean age before the pandemic was 58.6 years, and 44.6% of the total sample population was male. The average time since LT before the pandemic was 4.7 years. Hypertension and diabetes mellitus were significantly increased among the sample population before and during the pandemic (P<.001).
None of the participants had been infected with COVID-19. Television was the main source of information about COVID-19 for 81 (96.4%) patients, followed by newspapers for 32 (38.1%), and news websites for 30 (35.7%). Only 1 patient (1.2%) used a transplant center as a main source of information.
CHANGES IN PA BEFORE AND DURING THE PANDEMIC:
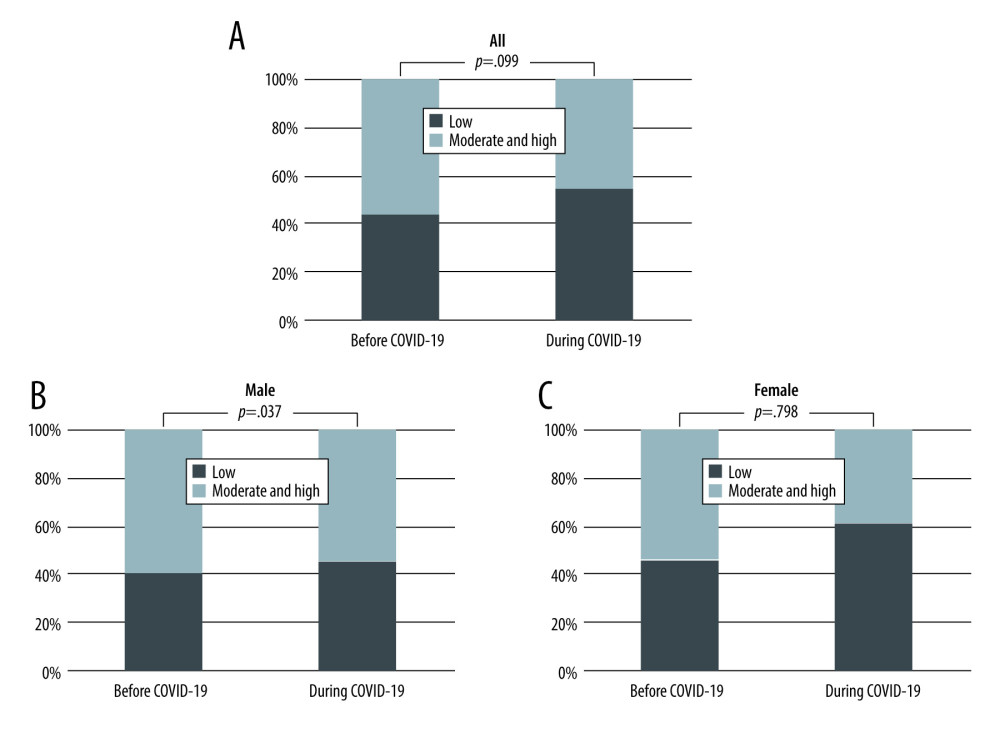
Table 1 shows the PA with IPAQ before and during the pandemic. Moderate-and-high PA reported by 56.0% of the participants before the pandemic decreased to 45.2% during the pandemic. Conversely, low PA increased from 44.0% to 54.8% before and during the pandemic, respectively. Overall, there was no statistically significant difference in PA levels before and during the pandemic (P=.099; Figure 1A). However, males had decreased moderate and high PA and increased low PA during the pandemic compared to before the pandemic (P=.037; Figure 1B). Females showed no change in PA before and during the pandemic (P=.798, Figure 1C).
FEAR OF COVID-19 AND DEPRESSION:
Table 2 displays a comparison of depression and fear of COVID-19 among the participants. Fear of shopping during the pandemic was stronger for females than for males (P=.023). There were no sex differences in the other 3 questions regarding the fear of COVID-19.
Only 4 participants (4.8%) had PHQ-9 scores of 10 or higher, indicating depression. The level of depression was moderate in 3 patients (3.6%), moderate-to-severe in 1 patient (1.2%), and there were no patients with severe depression (Table 2).
RELATIONSHIP BETWEEN PA AND FEAR OF COVID-19 AND DEPRESSION DURING THE PANDEMIC:
Table 3 shows demographic characteristics, depression, and fear of COVID-19 during the pandemic in the inactive and active groups. Univariate analysis showed that the inactive group was significantly more fearful of immunosuppressants and hospital/shopping infections during the pandemic than the active group. The active group had stronger exercise habits than the inactive group (P=.045). There were no differences in the level of depression between the 2 groups.
In a comparison by sex, among males, the inactive group was significantly more fearful of immunosuppressants and hospital/shopping infections during the pandemic than the active group (
Logistic regression analysis was conducted to explore the association between PA and depression during the pandemic and the fear of COVID-19 based on univariate analysis results. “I am afraid of becoming infected in the hospital” was strongly correlated with “I am afraid of becoming infected while shopping” (r=0.8) and was excluded owing to multicollinearity considerations. “I am afraid of becoming infected while shopping” was a significant independent factor for inactivity during the pandemic (OR=1.917, CI=1.059, 3.468, P=.032; Table 4).
Discussion
This study investigated the changes in PA levels among patients approximately 8 years post-LT before and 1 year after the onset of the COVID-19 pandemic. The results revealed a decrease in moderate- and high-intensity PA and an increase in low-intensity PA during the pandemic, especially in males. Fear of being infected with COVID-19 while shopping was higher among females and was an independent factor of inactivity during the pandemic. Only 4.8% of post-LT patients were depressed during the pandemic.
A previous study using IPAQ in healthy participants reported that high-and-moderate PA significantly decreased and low PA increased during the pandemic [27], which was in line with the findings of our study. The COVID-19 pandemic has resulted in widespread global lockdowns, with people confined to their homes except for work and essential activities. These precautionary measures may have led to a decrease in moderate-and-high PA, as they discouraged outdoor PA-intensive activities such as walking and running [28] that are involved in moderate-and-high PA [21]. Male patients had significantly increased low PA before and during the pandemic. Those who work from home during the pandemic had reported significantly lower levels of PA than those not working from home [29]. Although it is not clear whether employed workers in this study work from home, more males are employed than females, and the increase in working from home may have influenced the change in PA levels. Overall, the lack of statistically significant differences in PA levels before and during the pandemic may be because LT patients generally have lower PA levels than the general population, even before the start of the pandemic. In the general population, 53.5% of those met the World Health Organization (WHO) PA recommendations for health [30] before the pandemic [31]. Conversely, only approximately 25% of patients 6 years after LT have met the WHO PA recommendations [7].
The study participants with moderate-and-high intensity PA levels had more regular exercise habits than those with low-intensity PA levels, and they voluntarily performed high-intensity PA activity even during COVID-19 restrictions. Therefore, support for patients with low-intensity PA requires essential considerations. Renal transplant recipients who underwent a PA program offered by a healthcare provider showed no decrease in PA during the pandemic, with 56% of patients exhibiting an active daily life of ≥30 METs-h/week, indicating the importance of PA support by healthcare providers [32]. The study suggests the need for developing new interventions for healthcare professionals, such as providing correct information on COVID-19 and individualized instructions, to promote and encourage routine above-moderate-intensity activities and exercise that can be performed indoors by patients with low PA.
Univariate analysis showed that inactive patients were more fearful of immunosuppressants and hospital/shopping-acquired infections than were active patients, and logistic regression analyses revealed that patients with a particularly strong fear of getting infected while shopping were approximately twice as likely to be inactive. In a comparative study of fear among post-LT patients and their household members, patients’ fear of being infected with SARS-CoV-2 was higher than that of their household members, although there was no significant difference in their fear of infection while shopping [16]. In Japan, as in the rest of the world, females were more fearful of becoming infected with SARS-CoV-2 while shopping compared to males. Divergent beliefs may be sex-related, as traditional sex roles dictate that females should undertake most of the housework, including grocery shopping [33,34]. Males in the inactive group were more fearful of infection while shopping than those in the active group, which may be because they went out less frequently outside of work.
Only 1 patient in this study used a transplant center as the important information source regarding COVID-19. Transplant centers should strengthen health literacy education and provide correct information on COVID-19 prevention behavior, especially for female patients.
Only 4 patients (4.9%) were depressed after LT, and most patients maintained good mental health during the pandemic. In a previous study of patients approximately 8 years after LT, 10.5% of patients were depressed during the pandemic, with PHQ ≥10, which was higher than the present findings [26]. The participants of the present study were likely less to be depressed than those in the previous studies because fewer had chronic diseases such as hypertension and diabetes, which are considered as risk factors for severe COVID-19. A systematic review analyzing the incidence of depression, stress, and anxiety during the pandemic in the general global population found depression in approximately 33% of individuals [35], with post-transplant patients exhibiting lower rates of depression than the general population. Although a French study on depression in pre-transplant renal transplant patients found that 51.6% of patients had depressive symptoms [36], transplant recipients were resilient and had previously overcome a life-threatening crisis. Therefore, LT patients are considered to have lower rates of depression than the general population, even during the pandemic. Only 4.9% of the patients in this study were depressed, which suggests that there was no significant association between PA and depression.
This study has several limitations. First, patients whose PA was not measured prior to the pandemic were not included, which may have created a participation bias. Second, the assessment of PA using self-administered questionnaires had the potential limitation of poor recall. Third, the reliability and validity of the items related to fear of COVID-19 have not been tested owing to the urgent need to conduct the survey. Fourth, due to the small sample size, logistic regression analysis was not conducted to examine differences between males and females in the relationship among PA during the pandemic, depression, and levels of fear of COVID-19 infection. Future studies should include a larger sample size and should measure PA, depression, and fear of being infected in post-LT patients during the COVID-19 pandemic using objective measures equipped with accelerometers and longitudinally validated tools.
Conclusions
This study demonstrated that moderate and high-intensity PA among post-LT patients decreased during the COVID-19 pandemic, especially in males, with more than half of the patients performing low-intensity activities in daily life. Fear of being infected with COVID-19 while shopping was stronger in females than in males, and was an independent factor affecting inactivity during the pandemic. Only 4.8% of post-LT patients were depressed. This study suggests the need to include the provision of transmitting accurate information about COVID-19 by healthcare professionals through transplant centers, especially for patients with low PA, to prevent PA decline in these patients.
Tables
Table 1. Demographic characteristics and physical activity of liver transplant patients before and during the COVID-19 pandemic.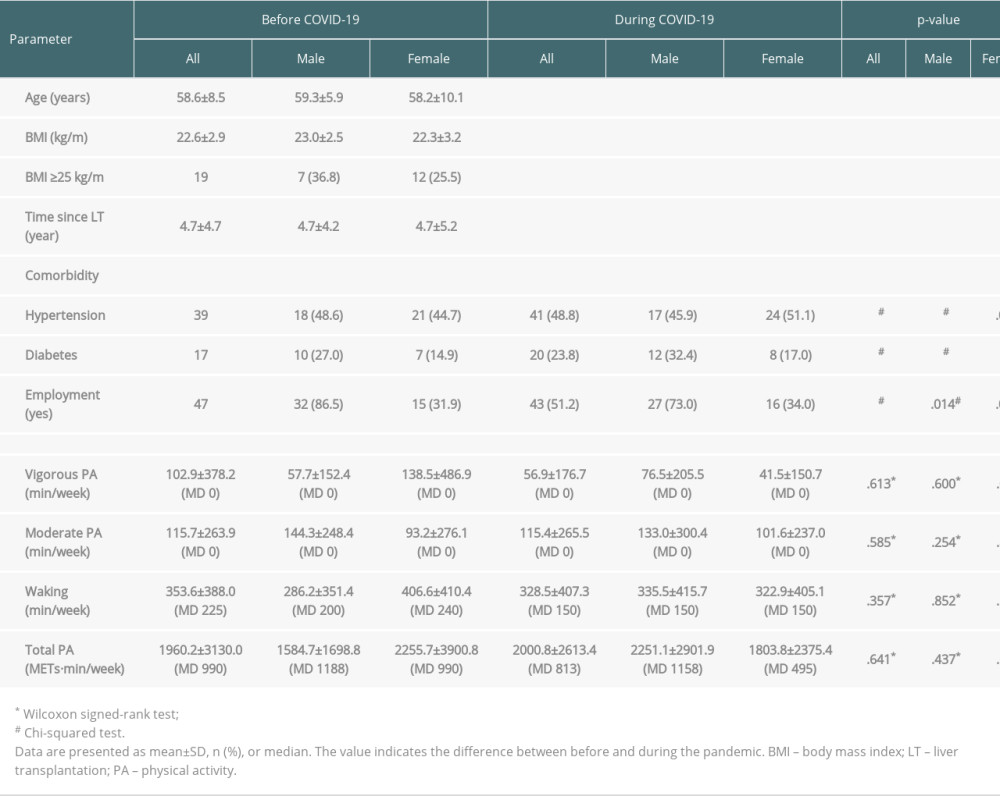 Table 2. Comparison of depression and fear of COVID-19 in liver transplant patients.
Table 2. Comparison of depression and fear of COVID-19 in liver transplant patients.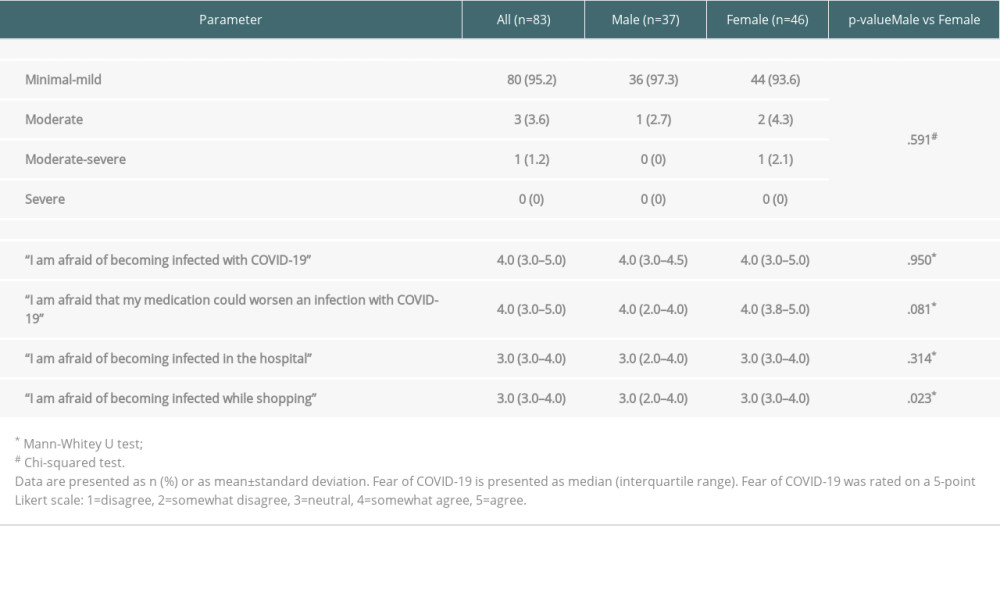 Table 3. Comparison of demographic characteristics, depression, and fear of COVID-19 among inactive and active groups.
Table 3. Comparison of demographic characteristics, depression, and fear of COVID-19 among inactive and active groups.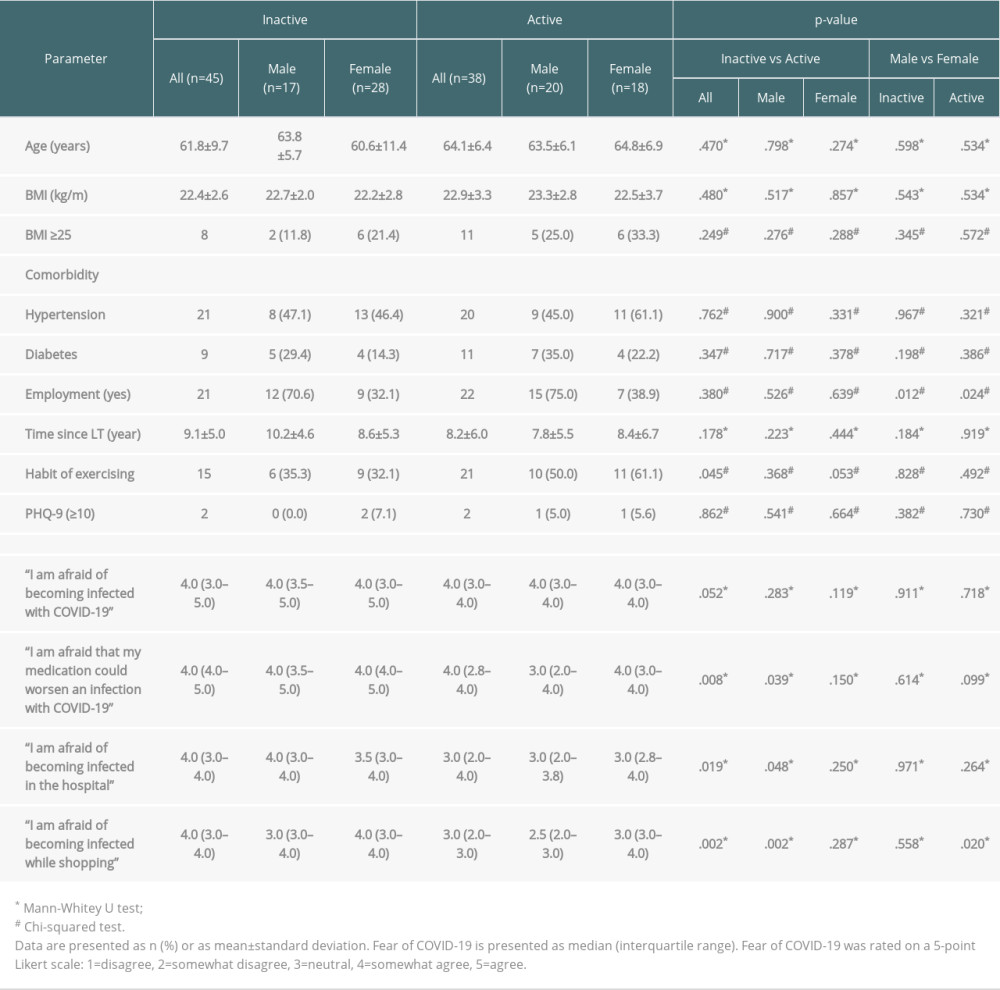 Table 4. Results of multiple logistic regression analysis for the association between physical activity, depression, and fear of COVID-19.
Table 4. Results of multiple logistic regression analysis for the association between physical activity, depression, and fear of COVID-19.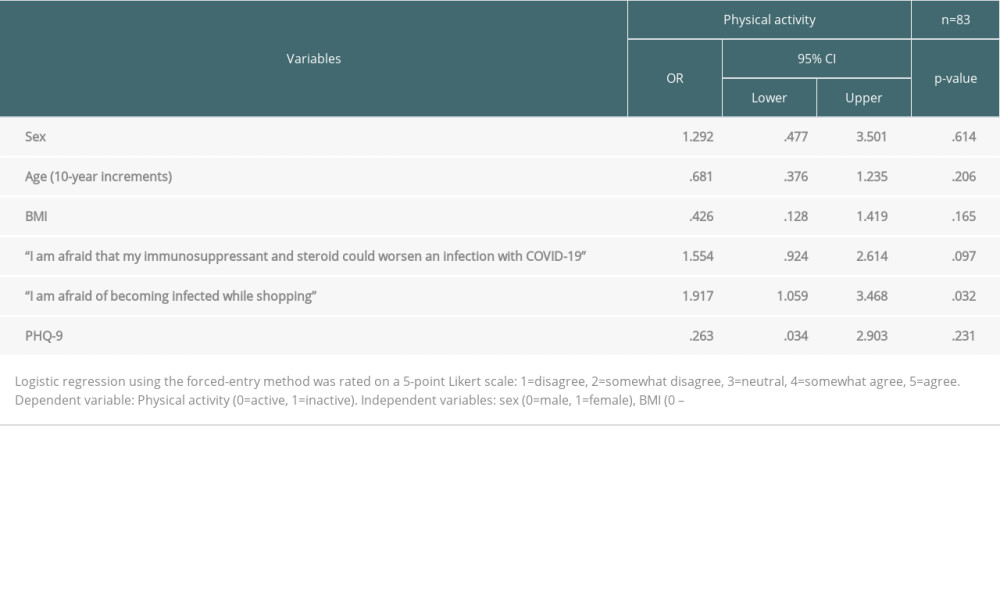
References
1. Kwong AJ, Kim WR, Lake JR, OPTN/SRTR 2019 annual data report: Liver: Am J Transplant, 2021; 2; 208-315
2. Avery RK, Chiang TP, Marr KA, Inpatient COVID-19 outcomes in solid organ transplant recipients compared to non-solid organ transplant patients: A retrospective cohort: Am J Transplant, 2021; 21; 2498-508
3. Boyarsky BJ, Antibody response to 2-dose SARS-CoV-2 mRNA vaccine series in solid organ transplant recipients: JAMA, 2021; 325; 2204-6
4. Azzi Y, Bartash R, Scalea J, Loarte-Campos P, Akalin E, COVID-19 and solid organ transplantation: A review article: Transplantation, 2021; 105; 37-55
5. Belsky JA, Tullius BP, Lamb MG, COVID-19 in immunocompromised patients: A systematic review of cancer, hematopoietic cell and solid organ transplant patients: J Infect, 2021; 82; 329-38
6. Munoz Serrano A, Arias A, Moreno-Torres V, Coronavirus disease 2019 (COVID-19) in solid organ transplant recipients: A case-control study: Ann Transplant, 2021; 26; e933152
7. Tanaka S, Fujita K, Makimoto K, Relationships of accelerometer-determined physical activity with obesity, hypertension, diabetes, dyslipidemia, and health-related quality of life in patients after liver transplantation: Clin Transplant, 2020; 34; e14117
8. Dunn MA, Rogal SS, Duarte-Rojo A, Lai JC, Physical function, physical activity, and quality of life after liver transplantation: Liver Transpl, 2020; 26; 702-8
9. Tanaka S, Fujita K, Kanaoka M, Prospective study of objective physical activity and quality of life in living donor liver transplant recipients: Jpn J Nurs Sci, 2020; 17; e12362
10. Zelle DM, Dorland HF, Rosmalen JG, Impact of depression on long-term outcome after renal transplantation: A prospective cohort study: Transplantation, 2012; 94; 1033-40
11. Makizako H, Akaida S, Shono S, Physical activity and perceived physical fitness during the COVID-19 epidemic: A population of 40- to 69-year-olds in Japan: Int J Environ Res Public Health, 2021; 18; 4832
12. Stockwell S, Trott M, Tully M, Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: A systematic review: BMJ Open Sport Exerc Med, 2021; 7; e000960
13. Zaccagni L, Toselli S, Barbieri D, Physical activity during COVID-19 lockdown in Italy: A systematic review: Int J Environ Res Public Health, 2021; 18; 6416
14. Yang LS, Shan LL, Saxena A, Morris DL, Liver transplantation: A systematic review of long-term quality of life: Liver Int, 2014; 34; 1298-313
15. Harper CA, Satchell LP, Fido D, Latzman RD, Functional fear predicts public health compliance in the COVID-19 pandemic: Int J Ment Health Addict, 2021; 19; 1875-88
16. Reuken PA, Rauchfuss F, Albers S, Between fear and courage: Attitudes, beliefs, and behavior of liver transplantation recipients and waiting list candidates during the COVID-19 pandemic: Am J Transplant, 2020; 20; 3042-50
17. Luo F, Ghanei Gheshlagh R, Dalvand S, Systematic review and meta-analysis of fear of COVID-19: Front Psychol, 2021; 12; 661078
18. Broche-Perez Y, Fernandez-Fleites Z, Jimenez-Puig E, Gender and fear of COVID-19 in a Cuban population sample: Int J Ment Health Addict, 2022; 20; 83-91
19. Bosselmann V, Amatriain-Fernandez S, Gronwald T, Physical activity, boredom and fear of COVID-19 among adolescents in Germany: Front Psychol, 2021; 12; 624206
20. Craig CL, Marshall AL, Sjostrom M, International Physical Activity Questionnaire: 12-Country reliability and validity: Med Sci Sports Exerc, 2003; 35; 1381-95
21. Murase N, Katsumura T, Ueda C, Validity and reliability of Japanese version of International Physical Activity Questionnaire (in Japanese): J Health Welfare Stat, 2002; 49; 1-9
22. IPAQ-Group, International Physical Activity Questionnaire: Cultural adaptation [cited 2022 Jun 14]
23. Muramatsu K, Miyaoka H, Kamijima K, Performance of the Japanese version of the Patient Health Questionnaire-9 (J-PHQ-9) for depression in primary care: Gen Hosp Psychiatry, 2018; 52; 64-69
24. Spitzer RL, Kroenke K, Williams JB, Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study: JAMA, 1999; 282; 1737-44
25. Kroenke K, Spitzer RL, Williams JB, The PHQ 9: Validity of a brief depression severity measure: J Gen Intern Med, 2001; 16; 606-13
26. Cuadrado A, Gaite LM, Odriozola A, Impact of the COVID-19 lockdown on liver transplant recipients. A single center observational study: Rev Esp Enferm Dig, 2022; 114(8); 448-54
27. Maugeri G, Castrogiovanni P, Battaglia G, The impact of physical activity on psychological health during COVID-19 pandemic in Italy: Heliyon, 2020; 6; e04315
28. Ainsworth BE, Haskell WL, Herrmann SD, 2011 compendium of physical activities: A second update of codes and MET values: Med Sci Sports Exerc, 2011; 43; 1575-81
29. World Health Organization: WHO guidelines on physical activity and sedentary behaviour [;cited 2022 Jul 1]https://www.who.int/publications/i/item/9789240015128
30. Macniven R, Bauman A, Abouzeid M, A review of population-based prevalence studies of physical activity in adults in the Asia-Pacific region: BMC Public Health, 2012; 12; 41
31. Hanke AA, Sundermeier T, Boeck HT, Influence of officially ordered restrictions during the first wave of COVID-19 pandemic on physical activity and quality of life in patients after kidney transplantation in a telemedicine-based aftercare program-A KTx360 degrees sub study: Int J Environ Res Public Health, 2020; 17; 9144
32. D’Acunto F, Malmendier U, Weber M, Gender roles produce divergent economic expectations: Proc Natl Acad Sci, 2021; 118; 2008534118
33. Oshio T, Nozaki K, Kobayashi M, Division of household labor and marital satisfaction in China, Japan, and Korea: J Family Econ Issues, 2012; 34; 211-23
34. Salari N, Hosseinian-Far A, Jalali R, Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis: Glob Health, 2020; 16; 57
35. Oshio T, Nozaki K, Kobayashi M, Division of household labor and marital satisfaction in China, Japan, and Korea: JFEI, 2012; 34; 211-23
36. Corruble E, Barry C, Varescon I, Report of depressive symptoms on waiting list and mortality after liver and kidney transplantation: A prospective cohort study: BMC Psychiatry, 2011; 11; 182
Tables
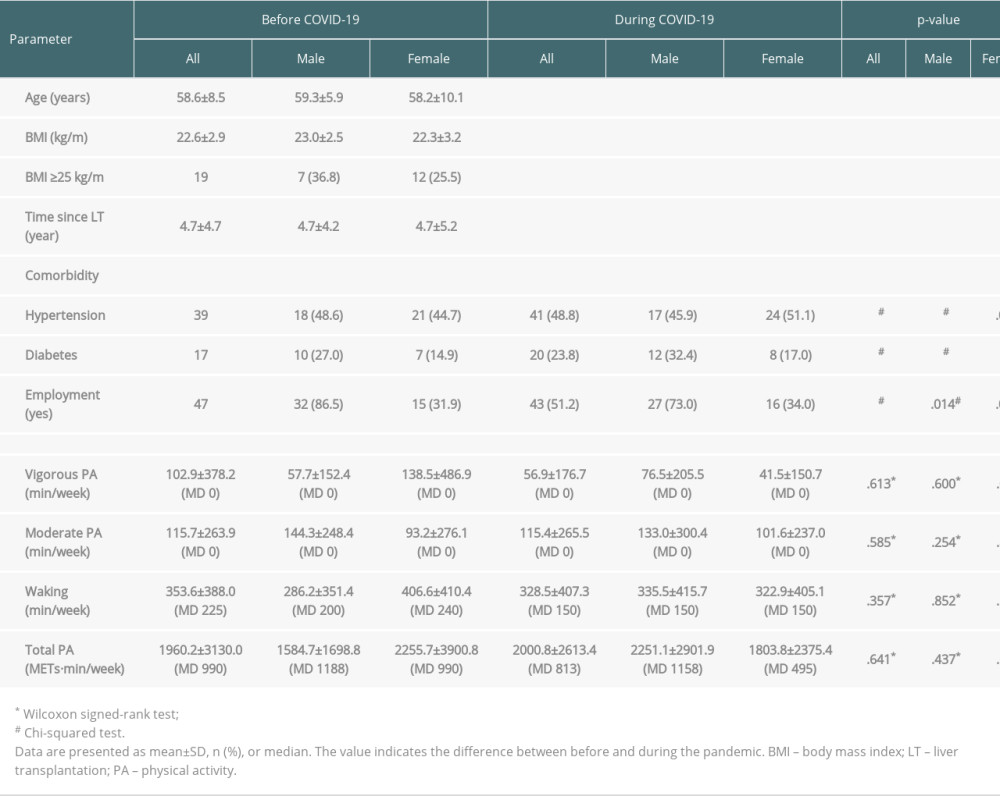 Table 1. Demographic characteristics and physical activity of liver transplant patients before and during the COVID-19 pandemic.
Table 1. Demographic characteristics and physical activity of liver transplant patients before and during the COVID-19 pandemic.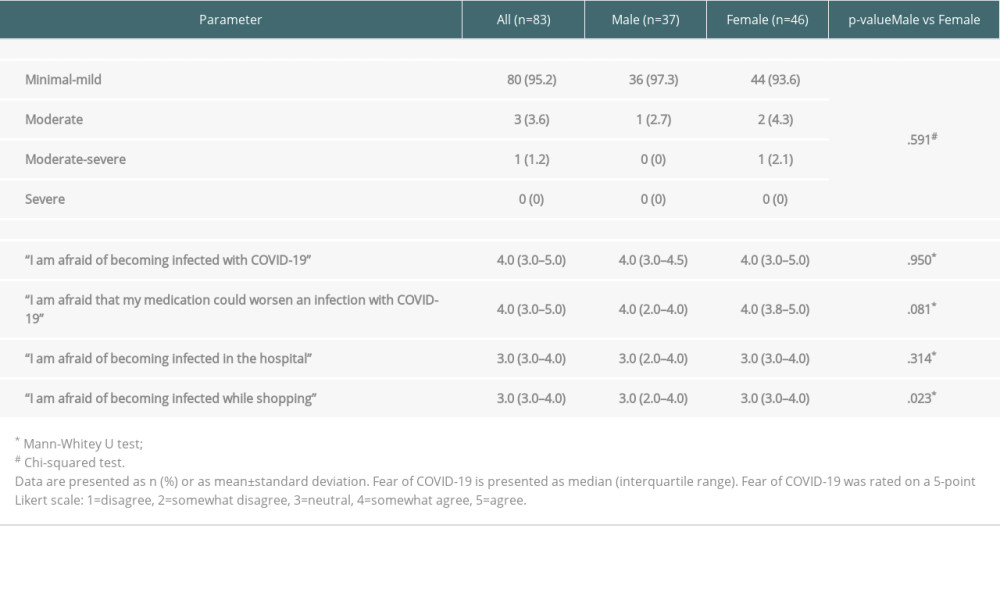 Table 2. Comparison of depression and fear of COVID-19 in liver transplant patients.
Table 2. Comparison of depression and fear of COVID-19 in liver transplant patients.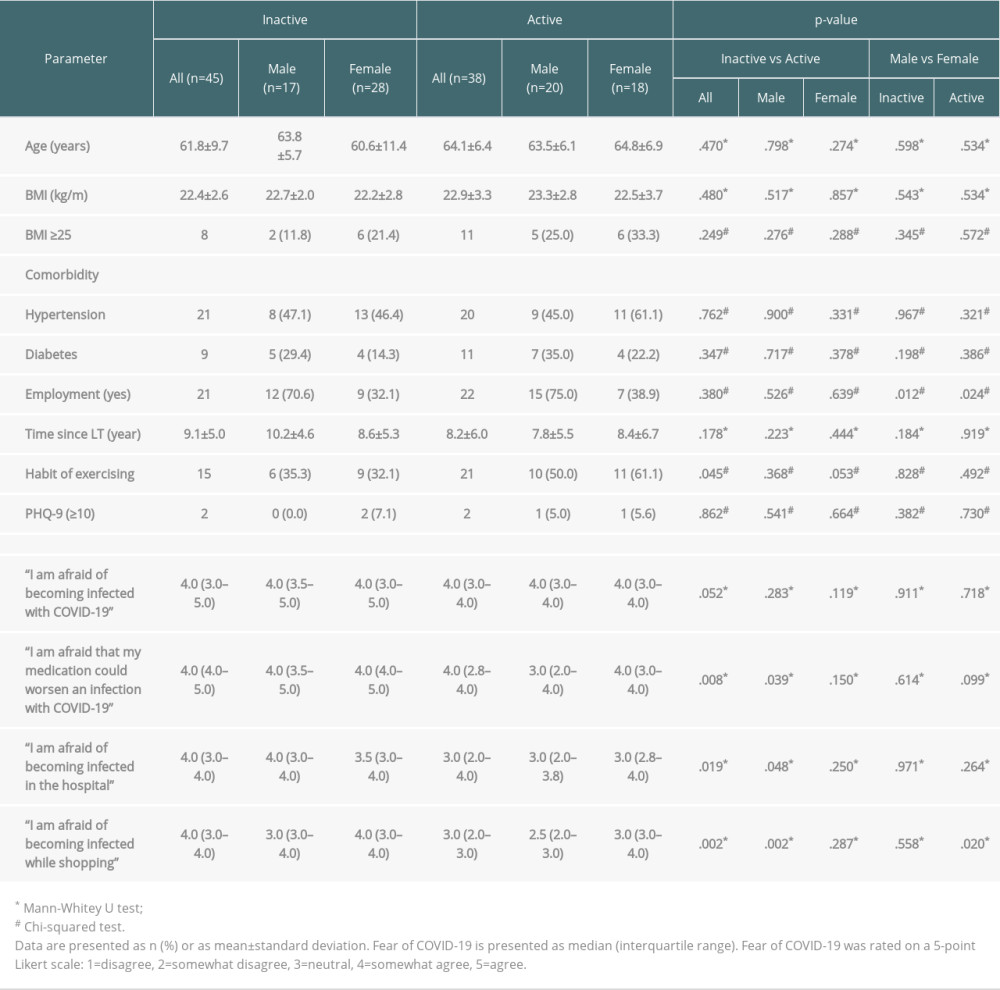 Table 3. Comparison of demographic characteristics, depression, and fear of COVID-19 among inactive and active groups.
Table 3. Comparison of demographic characteristics, depression, and fear of COVID-19 among inactive and active groups.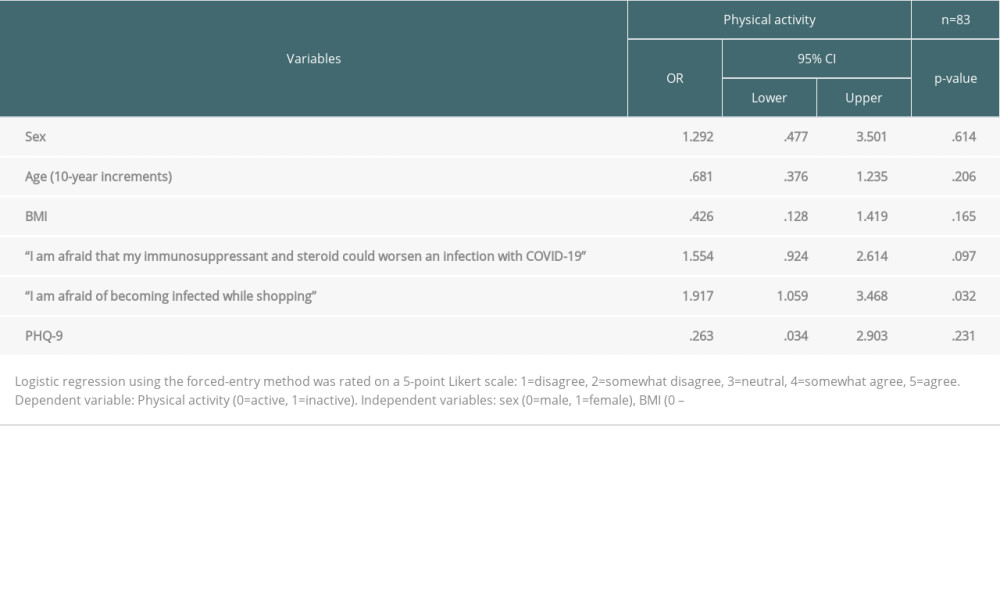 Table 4. Results of multiple logistic regression analysis for the association between physical activity, depression, and fear of COVID-19.
Table 4. Results of multiple logistic regression analysis for the association between physical activity, depression, and fear of COVID-19.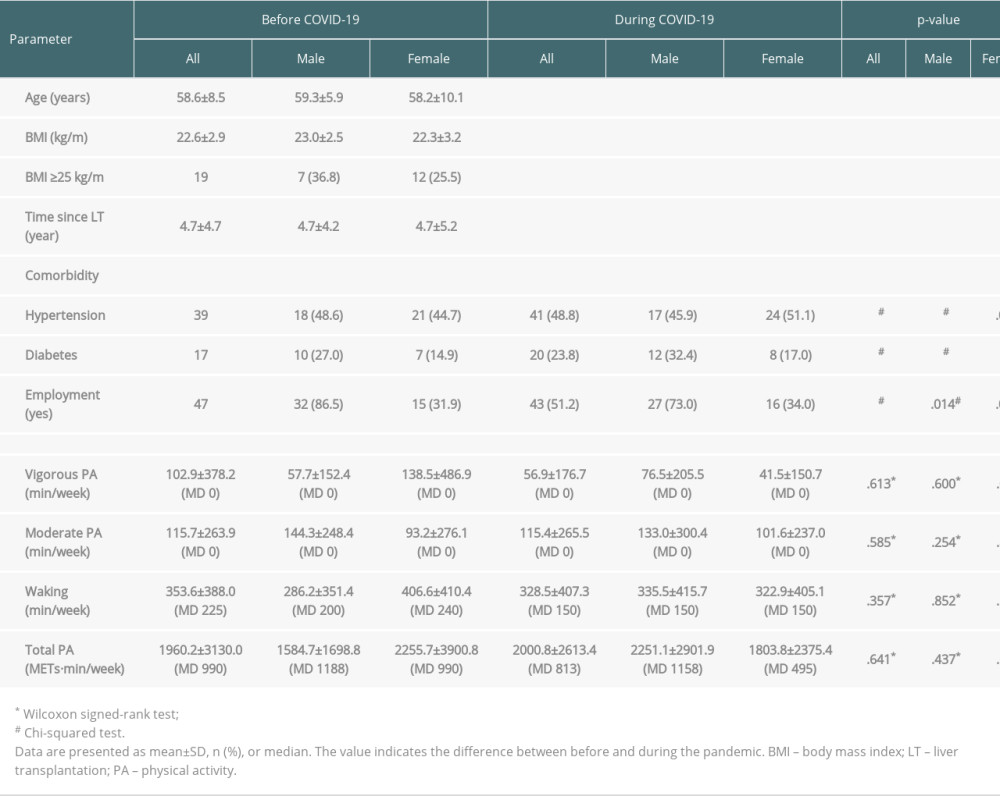 Table 1. Demographic characteristics and physical activity of liver transplant patients before and during the COVID-19 pandemic.
Table 1. Demographic characteristics and physical activity of liver transplant patients before and during the COVID-19 pandemic.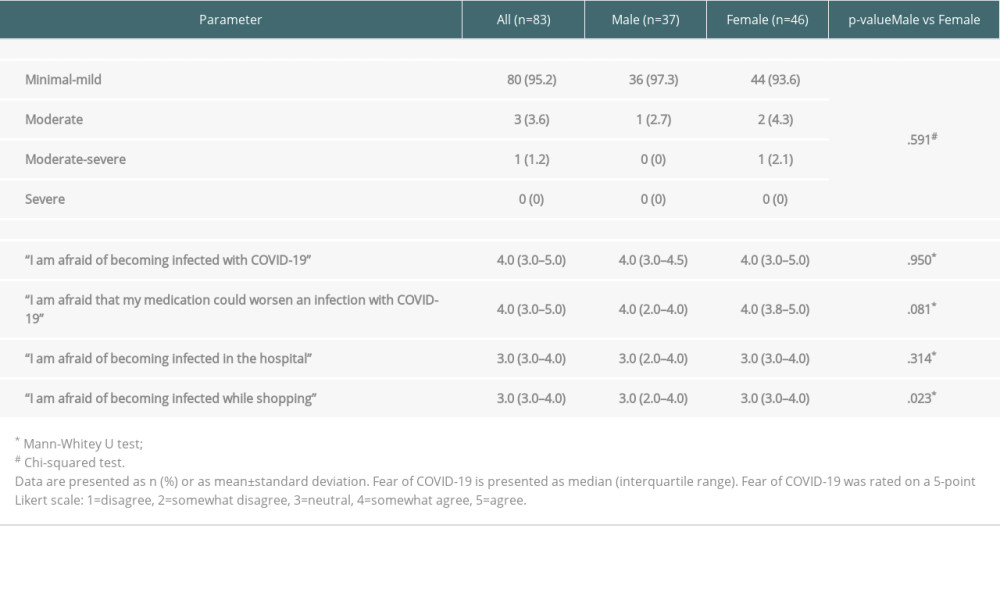 Table 2. Comparison of depression and fear of COVID-19 in liver transplant patients.
Table 2. Comparison of depression and fear of COVID-19 in liver transplant patients.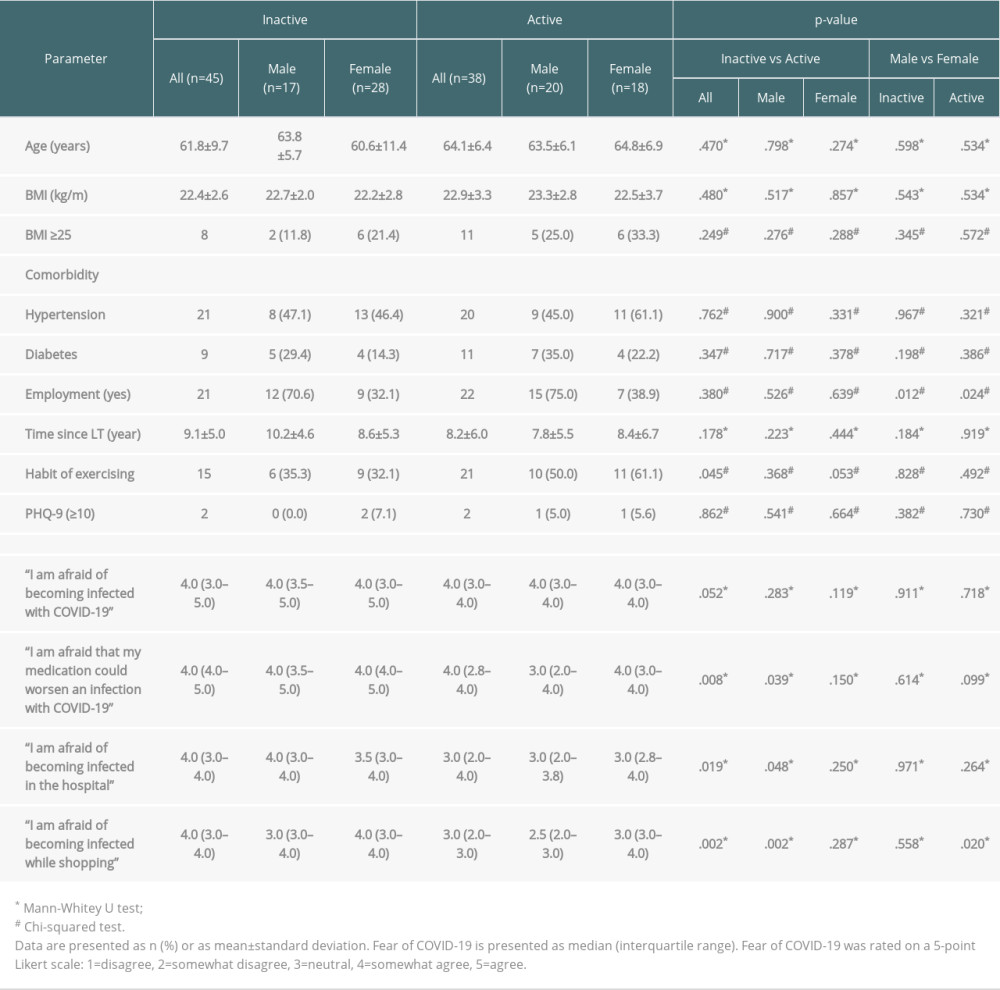 Table 3. Comparison of demographic characteristics, depression, and fear of COVID-19 among inactive and active groups.
Table 3. Comparison of demographic characteristics, depression, and fear of COVID-19 among inactive and active groups.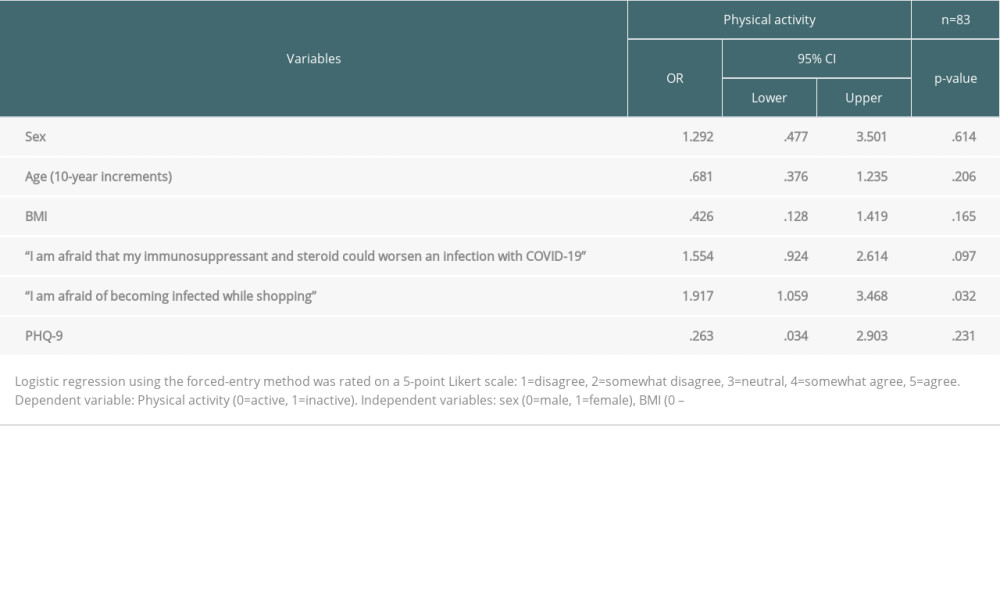 Table 4. Results of multiple logistic regression analysis for the association between physical activity, depression, and fear of COVID-19.
Table 4. Results of multiple logistic regression analysis for the association between physical activity, depression, and fear of COVID-19. In Press
18 Mar 2024 : Original article
Does Antibiotic Use Increase the Risk of Post-Transplantation Diabetes Mellitus? A Retrospective Study of R...Ann Transplant In Press; DOI: 10.12659/AOT.943282
20 Mar 2024 : Original article
Transplant Nephrectomy: A Comparative Study of Timing and Techniques in a Single InstitutionAnn Transplant In Press; DOI: 10.12659/AOT.942252
28 Mar 2024 : Original article
Association Between FEV₁ Decline Rate and Mortality in Long-Term Follow-Up of a 21-Patient Pilot Clinical T...Ann Transplant In Press; DOI: 10.12659/AOT.942823
02 Apr 2024 : Original article
Liver Transplantation from Brain-Dead Donors with Hepatitis B or C in South Korea: A 2014-2020 Korean Organ...Ann Transplant In Press; DOI: 10.12659/AOT.943588
Most Viewed Current Articles
05 Apr 2022 : Original article
Impact of Statins on Hepatocellular Carcinoma Recurrence After Living-Donor Liver TransplantationDOI :10.12659/AOT.935604
Ann Transplant 2022; 27:e935604
12 Jan 2022 : Original article
Risk Factors for Developing BK Virus-Associated Nephropathy: A Single-Center Retrospective Cohort Study of ...DOI :10.12659/AOT.934738
Ann Transplant 2022; 27:e934738
22 Nov 2022 : Original article
Long-Term Effects of Everolimus-Facilitated Tacrolimus Reduction in Living-Donor Liver Transplant Recipient...DOI :10.12659/AOT.937988
Ann Transplant 2022; 27:e937988
15 Mar 2022 : Case report
Combined Liver, Pancreas-Duodenum, and Kidney Transplantation for Patients with Hepatitis B Cirrhosis, Urem...DOI :10.12659/AOT.935860
Ann Transplant 2022; 27:e935860