03 October 2023: Original Paper
Impact of Blood Pressure on Risk of Graft Failure or Death Among Patients After Kidney Transplantation in a 10-Year Observational Period: A Single-Center Retrospective Analysis
Tomasz Pilecki1ABCDEF, Bożena Czarkowska-PączekDOI: 10.12659/AOT.939472
Ann Transplant 2023; 28:e939472
Abstract
BACKGROUND: Hypertension is a risk factor for graft failure and mortality among kidney transplant recipients (KTRs). The aim of the study was to examine blood pressure (BP) as a factor that contributes to graft failure or death during a 10-year observation period.
MATERIAL AND METHODS: The study group comprised 70 KTRs who were treated according to their clinical state. Data were collected at 1 month and 1 year after transplantation and included office and ambulatory BP monitoring (ABPM) BP values, eGFR, proteinuria, and BMI. During the observation period, 6 patients died, and 10 lost the graft, but not during the first year.
RESULTS: Office and ABPM BP values were within normal ranges and did not differ from each other. eGRF and BMI were higher at 1 year compared to 1 month after transplantation, and proteinuria decreased. Among those who died, DBP was lower compared to those of survivors with graft failure. Proteinuria and donor age were positively correlated with BP.
CONCLUSIONS: Monitoring of BP and adequate treatment of hypertension resulting in BP values within normal values among KTRs contribute to longer survival of the graft and recipient. Older donor age and proteinuria could predict post-transplant hypertension. Low diastolic BP of the recipient could increase the risk of death among KTRs. Despite the fact that ABPM is the blood pressure measurement method of choice, appropriate standard office measurement could also be used for BP monitoring.
Keywords: Kidney Transplantation, Hypertension, Graft Rejection, Humans, Blood Pressure, Retrospective Studies, Blood Pressure Monitoring, Ambulatory, Proteinuria
Background
Transplantation is currently the treatment of choice for patients with end-stage renal disease (ESRD) and is associated with reduced mortality due to many factors, including cardiovascular disease (CVD). However, the population of kidney transplant recipients (KTRs) still remains at higher risk for CVD compared to the general population [1–3]. Hypertension is one of the most common traditional risk factors for CVD in this population, with prevalence between 70% and 95% [2,4–7].
The differences in the epidemiological data regarding hypertension in KTRs derive from different cut-off values. According to the Kidney Disease Improving Global Outcomes Guidelines (KDIGO) issued in 2021, hypertension is diagnosed when office blood pressure (BP) is higher than 130/80 mmHg and ambulatory BP monitoring (ABPM) exceeds 125/75 mmHg [2,8]. These values are in line with those proposed by the American College of Cardiology/American Heart Association in 2017 [9], but they differ from those established by the European Society of Cardiology/European Society of Hypertension in 2018, in which the cut-off values were 140/90 mmHg and 130/80 mmHg for office measurement and ABPM, respectively [2,10].
Risk factors for post-transplant hypertension include recipient factors present before transplantation, such as longstanding hypertension, genetic profile, age, increased body mass index (BMI), and endocrine factors. They also include factors related to ESKD and the transplantation itself, such as the donor’s pre-transplantation hypertension, donor age, higher than recommended sodium intake, poor allograft quality, the specific donor’s genetic profile or acute or chronic allograft rejection, and immunosuppressive medications, particularly steroids [11–13]. Literature data indicate that lowering systolic BP (SBP) decreases the risk of CVD and the overall mortality among KTRs. Is has also been attributed to better kidney function and graft survival. But despite these facts, the optimal BP among KTRs is still uncertain [2,14].
The main goal of post-transplant care is to improve graft and patient survival. Hypertension is established as a risk factor that could interfere with this goal. Therefore, we aimed to evaluate blood pressure monitoring and the possible impact on graft failure (GF) or patient death during a 10-year follow-up period.
Material and Methods
STATISTICAL ANALYSIS:
Statistical analyses were performed using IBM SPSS Statistics 25.0. Descriptive statistics were generated using standard parameters, including percentage, mean, and standard deviation. Between-group differences were analysed using a
To detect significant relationships between variables, Pearson’s methods were applied for quantitative variables. For categorical variables and quantitative variables, predictive solution Eta was applied. Cox proportional-hazards regression analysis was used to estimate the impact on GF (death or graft lost) of SBP, DBP, and the coefficient of variation (CV) of BP. Results were considered significant at
Results
The selected clinical parameters, eGFR, proteinuria, and BMI evaluated at 1mTx and 1yTx are shown in Table 1. eGRF and BMI significantly increased at 1yTx compared to 1mTx, and proteinuria significantly decreased.
Table 2 shows the results of SO, ABPM SBP and DBP (mean values from a 24-h period), and a comparison between these measures. All values were within normal ranges, but SBP was significantly lower at 1yTx compared to 1mTx (SO: 130.76±12.39 vs 134.67±15.05,
Table 3 shows the mean values of ABPM SBP and DBP during the daytime (D, 6 am to 10 pm) and night (N, 10 pm to 6 am the next day) at 1mTx and 1yTx and a comparison between these measures. 1mTx SBP was higher at night compared to the day, whereas DBP did not differ. At 1yTx, both SBP and DBP were higher during the day compared to night.
We assessed the correlations between mean values of SBP and DBP measured by ABPM at 1mTx and 1yTx, recipient and donor age, recipient and donor sex, recipient eGFR, proteinuria, and BMI. A positive correlation was found between SBP at 1mTx and donor age (r=0.33,
To investigate the impact of hypertension on both GF (graft failure or recipient death [RD]) and RD alone, we observed the recipients for 10 years. During this period, 6 recipients died (but not during the first year of observation), while 10 patients experienced graft lost and were referred to dialysis. The comparison between GF and survivors did not show any differences at 1mTx or 1yTx in mean values of SBP and DBP measured by ABPM, day and night ABPM SBP and DBP. The results are shown in Table 4.
To show the potential impact of BP values on the risk of death among GF group, we compared those who lost the graft (GL) with the group of patients who died (RD). This revealed a significantly lower mean value of DBP measured by ABPM and values during day and night at 1mTx, but not after 1yTx in the RD group. The results are shown in Table 5.
We investigated the impact of mean values of SBP and DBP measured with ABPM and the CV of SBP and DBP (standard deviation/mean value) at 1mTx and 1yTx on the GF using Cox regression analysis. SBP and DBP and the CV of SBP and DBP did not influence GF.
Discussion
LIMITATIONS:
KTRs are a special group of patients with multiple diseases, who undergo complex therapy, and several factors that are different from the general population could influence the hypertension outcomes. The number of patients included into the study was limited, which could have biased the results.
Conclusions
In conclusion, close monitoring of BP and adequate treatment of possible hypertension resulting in BP values within normal and advised ranges among KTRs contribute to longer graft and recipient survival. Older donor age and proteinuria could predict post-transplant hypertension. Low diastolic BP of the recipient could increase the risk of death among KTRs. Despite the fact that ABPM is the BP measurement method of choice, appropriate standard office measurement could also be used for BP monitoring.
Tables
Table 1. eGFR (ml/min), proteinuria (g/24 hours), and BMI evaluated at 1 month (1mTx) and 1 year (1yTx) after transplantation.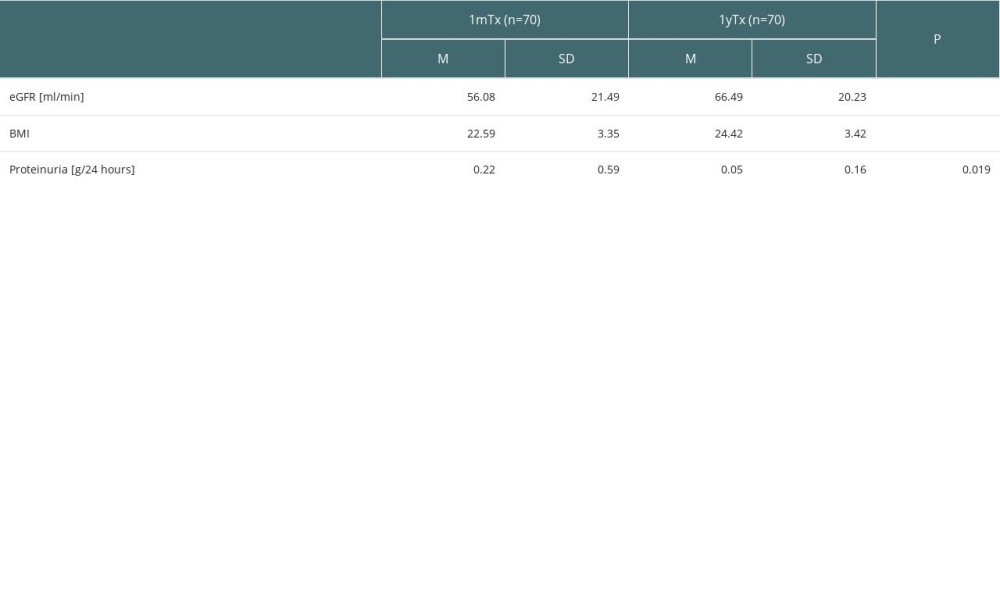 Table 2. The results of standard office BP and ABPM (mean values from 24-hour period) at 1 month after transplantation (1mTX) and 1 year after transplantation (1yTx) and comparison between these measures.
Table 2. The results of standard office BP and ABPM (mean values from 24-hour period) at 1 month after transplantation (1mTX) and 1 year after transplantation (1yTx) and comparison between these measures.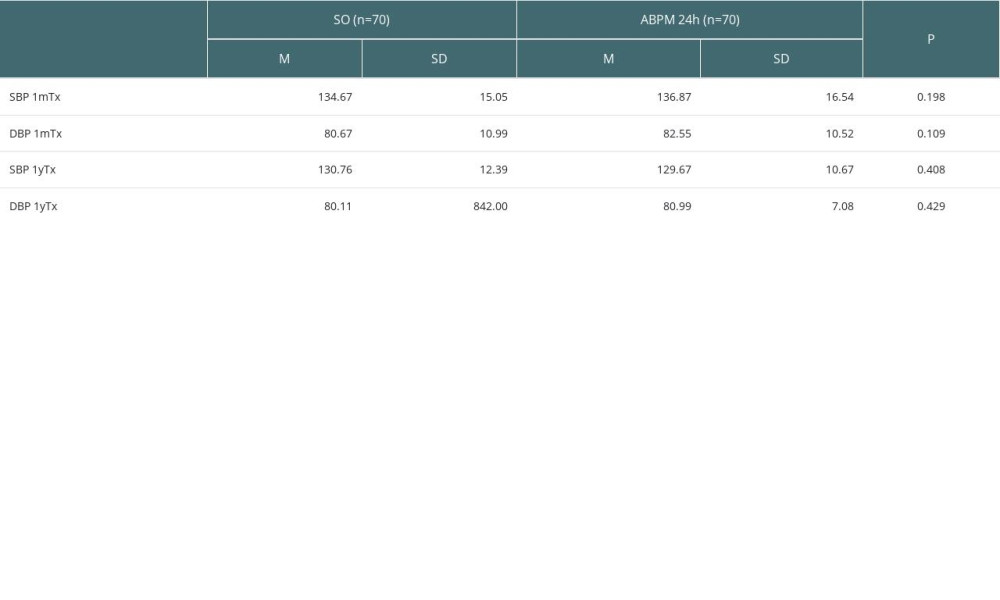 Table 3. Mean values of systolic (SBP) and diastolic BP (DBP) measured with ABPM during daytime (D, 6 am to 10 pm) and during night (N, 10 pm to 6 am the next day) at 1 month after transplantation (1mTx) and 1 year after transplantation (1yTx).
Table 3. Mean values of systolic (SBP) and diastolic BP (DBP) measured with ABPM during daytime (D, 6 am to 10 pm) and during night (N, 10 pm to 6 am the next day) at 1 month after transplantation (1mTx) and 1 year after transplantation (1yTx).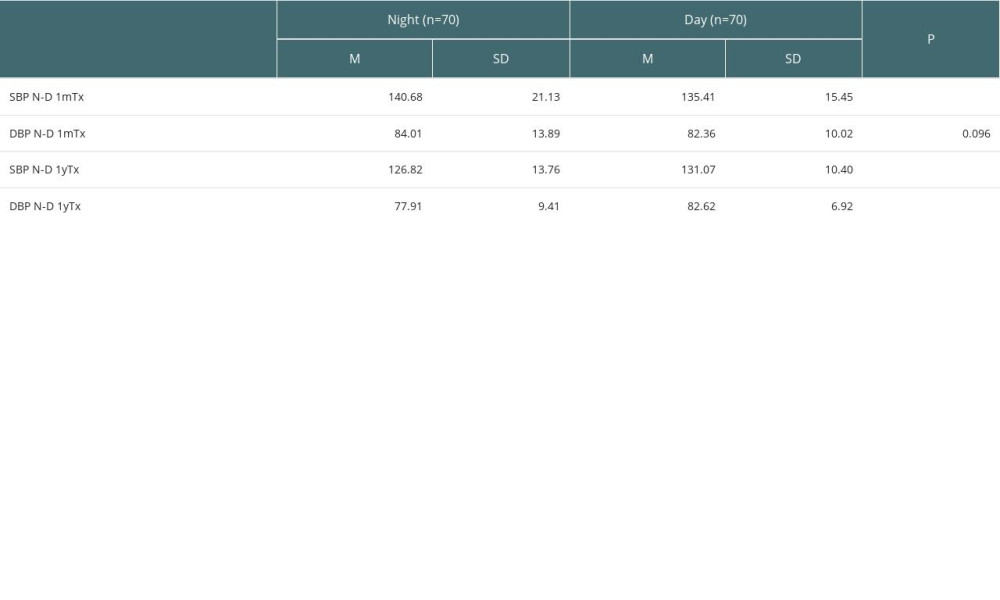 Table 4. Comparison of mean values of SBP and DBP measured by ABPM, mean values of SBP and DBP measured by ABPM during daytime (D) and night (N) at 1 month (1mTx) and 1 year after transplantation (1yTx) between those with graft failure (graft loss or death) and 10-year survivors.
Table 4. Comparison of mean values of SBP and DBP measured by ABPM, mean values of SBP and DBP measured by ABPM during daytime (D) and night (N) at 1 month (1mTx) and 1 year after transplantation (1yTx) between those with graft failure (graft loss or death) and 10-year survivors.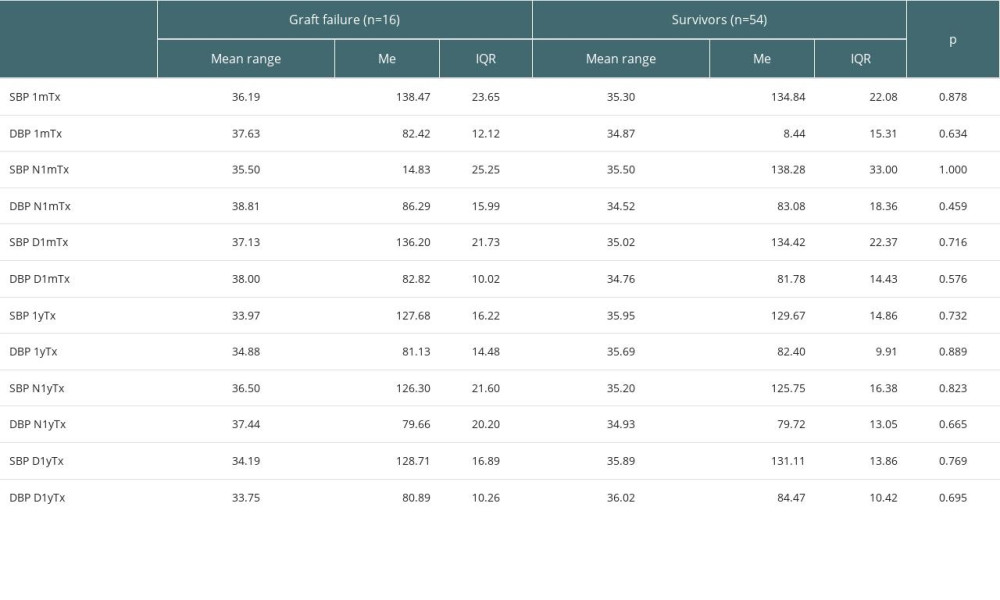 Table 5. Comparison of mean values of SBP and DBP measured by ABPM, mean values of SBP and DBP measured by ABPM during day (D) and during night (N) after 1 month after transplantation (at 1mTx) between those who died (RD) and those who lost the graft (GL).
Table 5. Comparison of mean values of SBP and DBP measured by ABPM, mean values of SBP and DBP measured by ABPM during day (D) and during night (N) after 1 month after transplantation (at 1mTx) between those who died (RD) and those who lost the graft (GL).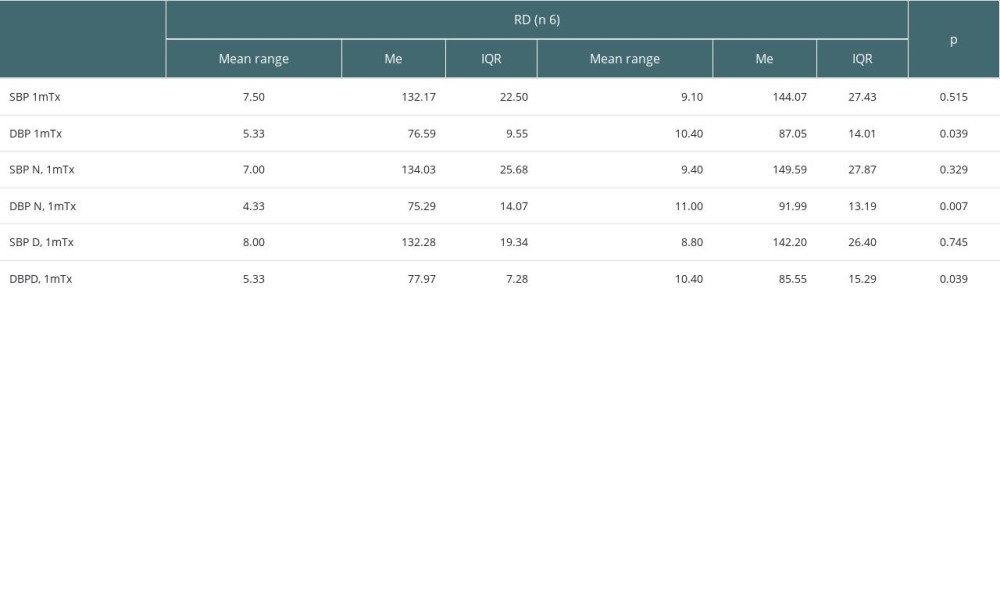
References
1. Rangaswami J, Mathew RO, Parasuraman R, Cardiovascular disease in the kidney transplant recipient: Epidemiology, diagnosis and management strategies: Nephrol Dial Transplant, 2019; 34; 760-73
2. Alexandrou ME, Ferro CJ, Boletis I, Hypertension in kidney transplant recipients: World J Transplant, 2022; 12; 211-22
3. Kramer BK, Boger C, Kruger B, Cardiovascular risk estimates and risk factors in renal transplant recipients: Transplantation Proceedings, 2005; 37; 1868-70
4. Loutradis C, Sarafidis P, Marinaki S, Role of hypertension in kidney transplant recipients: J Hum Hypertens, 2021; 35; 958-69
5. Ku E, Lee BJ, Wei J, Weir MR, Hypertension in CKD: Core curriculum 2019: Am J Kidney Dis, 2019; 74; 120-31
6. Zbroch E, Małyszko J, Myśliwiec M, Hypertension in solid organ transplant recipients: Ann Transplant, 2012; 17; 100-7
7. Czyżewski Ł, Wyzgał J, Kołek A, Evaluation of selected risk factors of cardiovascular diseases among patients after kidney transplantation, with particular focus on the role of 24-hour automatic blood pressure measurement in the diagnosis of hypertension: an introductory report: Ann Transplant, 2014; 19; 188-98
8. : KDIGO 2021 clinical practice guideline for the management of blood pressure in CKD Available from: https://kdigo.org/wp-content/uploads/2021/03/KDIGO-2021-BP-Guideline-Speakers-Guide.pdf
9. Whelton PK, Carey RM, Aronow WS, 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines: J Am Coll Cardiol, 2018; 71; e127-e248
10. Williams B, Mancia G, Spiering W, 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: J Hypertens, 2018; 36; 1953-2041
11. Weir MR, Burgess ED, Cooper JE, Assessment and management of hypertension in transplant patients: J Am Soc Nephrol, 2015; 26; 1248-60
12. Halimi JM, Ortiz A, Sarafidis PA, Hypertension in kidney transplantation: A consensus statement of the ‘hypertension and the kidney’ working group of the European Society of Hypertension: J Hypertens, 2021; 39; 1513-21
13. Rodrigo E, Monfá E, Albines Z, Sodium excretion pattern at 1 year after kidney transplantation and high blood pressure: Ann Transplant, 2015; 20; 569-75
14. Malhotra R, Katz R, Weiner DE, Blood pressure, chronic kidney disease progression, and kidney allograft failure in kidney transplant recipients: A secondary analysis of the FAVORIT trial: Am J Hypertens, 2019; 32; 816-23
15. Ghelichi-Ghojogh M, Ghaem H, Mohammadizadeh F, Graft and patient survival rates in kidney transplantation, and their associated factors: A systematic review and meta-analysis: Iran J Public Health, 2021; 50; 1555-63
16. Poggio ED, Augustine JJ, Arrigain S, Long-term kidney transplant graft survival-Making progress when most needed: Am J Transplant, 2021; 21; 2824-32
17. : Polstransplant Biuletyn Informacyjnty, 2022; 1(31) Available at: in Polishhttps://files.poltransplant.org.pl/Biuletyn_2022_www.pdf
18. Hariharan S, Israni AK, Danovitch G, Long-term survival after kidney transplantation: N Engl J Med, 2021; 385; 729-43
19. Ueki K, Tsuchimoto A, Matsukuma Y, Development and validation of a risk score for the prediction of cardiovascular disease in living donor kidney transplant recipients: Nephrol Dial Transplant, 2021; 36; 365-74
20. Bielopolski D, Rahamimov R, Zingerman B, Microalbuminuria after kidney transplantation predicts cardiovascular morbidity: Front Med (Lausanne), 2021; 8; 635847
21. Mucha K, Foroncewicz B, Ryter M, Weight gain in renal transplant recipients in a Polish single centre: Ann Transplant, 2015; 20; 16-20
22. Magga L, Maturana S, Olivares M, Identifying factors predicting kidney graft survival in Chile using elastic-net-regularized Cox’s regression: Medicina (Kaunas), 2022; 58; 1348
23. Coemans M, Süsal C, Döhler B, Analyses of the short- and long-term graft survival after kidney transplantation in Europe between 1986 and 2015: Kidney Int, 2018; 94; 964-73
24. Kasiske BL, Anjum S, Shah R, Hypertension after kidney transplantation: Am J Kidney Dis, 2004; 43; 1071-81
25. Carpenter MA, John A, Weir MR, BP, cardiovascular disease, and death in the Folic Acid for Vascular Outcome Reduction in Transplantation trial: J Am Soc Nephrol, 2014; 25; 1554-62
26. Ari E, Fici F, Robles NR, Hypertension in kidney transplant recipients: Where are we today?: Curr Hypertens Rep, 2021; 23; 21
27. Pagonas N, Markakis K, Bauer F, The impact of blood pressure variability and pulse pressure on graft survival and mortality after kidney transplantation: Clin Transplant, 2019; 33; e13448
28. Del Pinto R, Pietropaoli D, Dobre M, Ferri C, Prognostic importance of long-term SBP variability in high-risk hypertension: J Hypertens, 2020; 38; 2237-44
29. Korogiannou M, Sarafidis P, Alexandrou ME, Ambulatory blood pressure trajectories and blood pressure variability in kidney transplant recipients: A comparative study against haemodialysis patients: Clin Kidney J, 2021; 15; 951-60
Tables
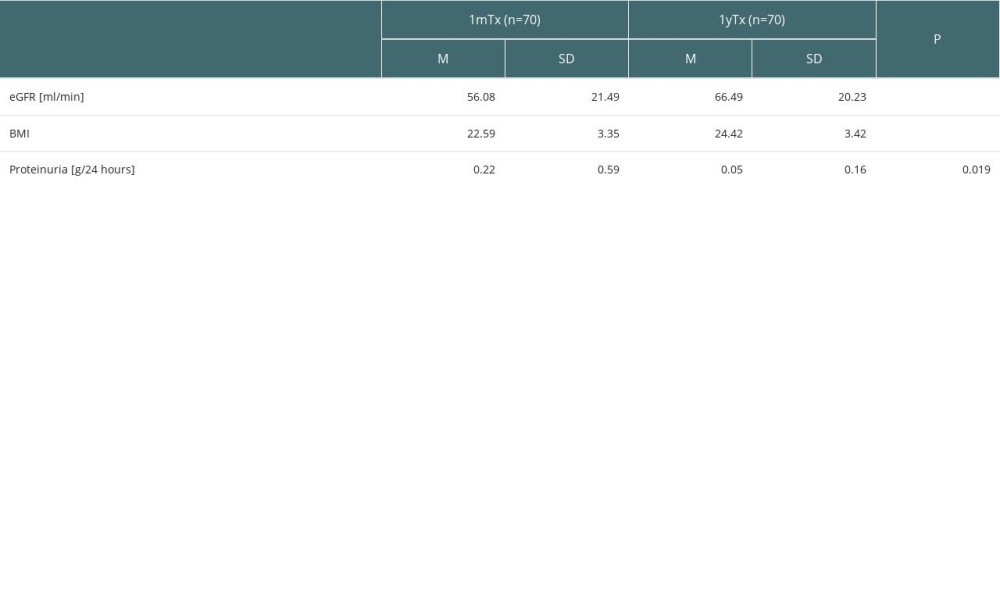 Table 1. eGFR (ml/min), proteinuria (g/24 hours), and BMI evaluated at 1 month (1mTx) and 1 year (1yTx) after transplantation.
Table 1. eGFR (ml/min), proteinuria (g/24 hours), and BMI evaluated at 1 month (1mTx) and 1 year (1yTx) after transplantation.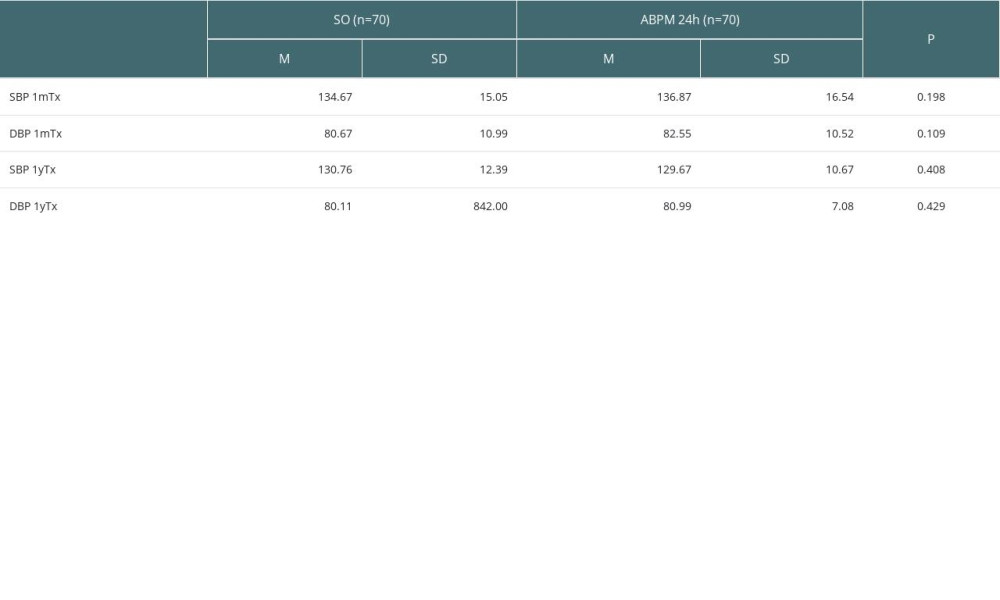 Table 2. The results of standard office BP and ABPM (mean values from 24-hour period) at 1 month after transplantation (1mTX) and 1 year after transplantation (1yTx) and comparison between these measures.
Table 2. The results of standard office BP and ABPM (mean values from 24-hour period) at 1 month after transplantation (1mTX) and 1 year after transplantation (1yTx) and comparison between these measures.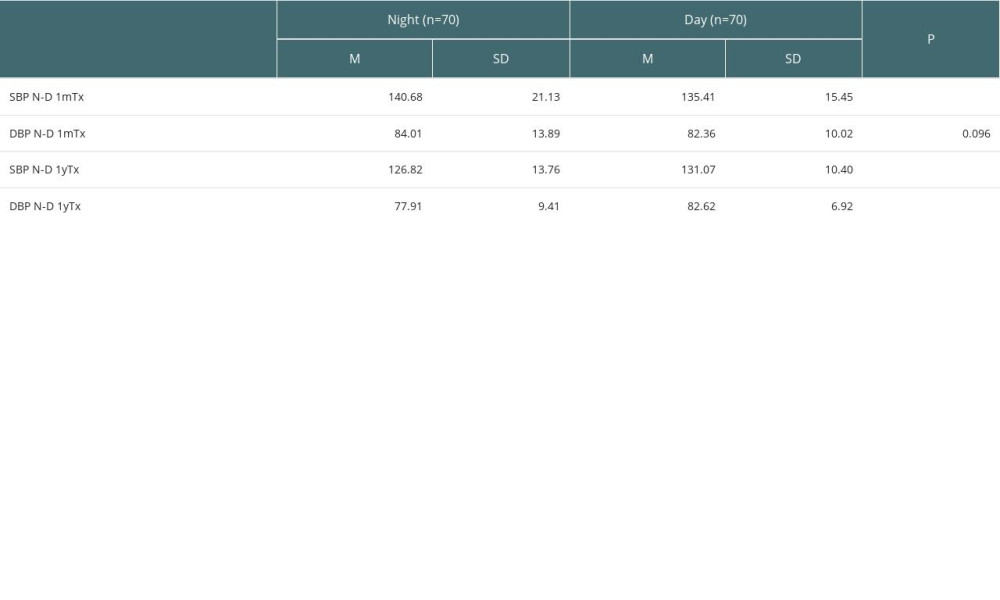 Table 3. Mean values of systolic (SBP) and diastolic BP (DBP) measured with ABPM during daytime (D, 6 am to 10 pm) and during night (N, 10 pm to 6 am the next day) at 1 month after transplantation (1mTx) and 1 year after transplantation (1yTx).
Table 3. Mean values of systolic (SBP) and diastolic BP (DBP) measured with ABPM during daytime (D, 6 am to 10 pm) and during night (N, 10 pm to 6 am the next day) at 1 month after transplantation (1mTx) and 1 year after transplantation (1yTx).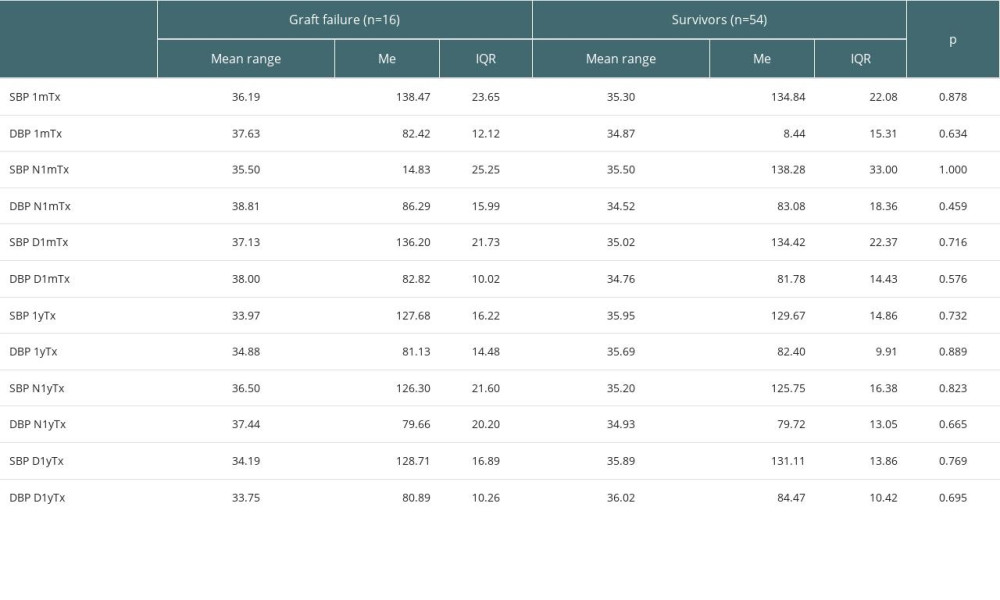 Table 4. Comparison of mean values of SBP and DBP measured by ABPM, mean values of SBP and DBP measured by ABPM during daytime (D) and night (N) at 1 month (1mTx) and 1 year after transplantation (1yTx) between those with graft failure (graft loss or death) and 10-year survivors.
Table 4. Comparison of mean values of SBP and DBP measured by ABPM, mean values of SBP and DBP measured by ABPM during daytime (D) and night (N) at 1 month (1mTx) and 1 year after transplantation (1yTx) between those with graft failure (graft loss or death) and 10-year survivors.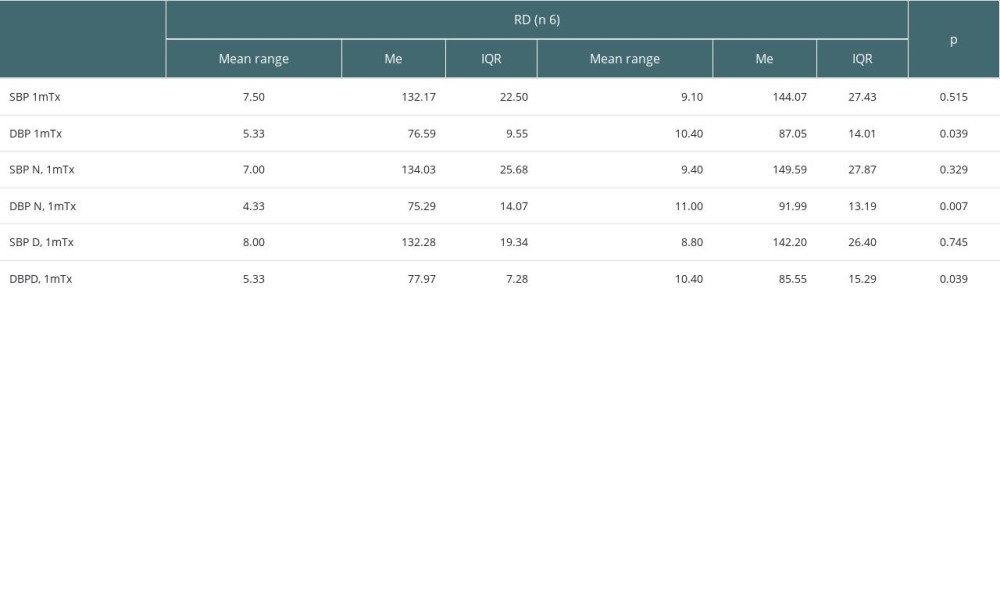 Table 5. Comparison of mean values of SBP and DBP measured by ABPM, mean values of SBP and DBP measured by ABPM during day (D) and during night (N) after 1 month after transplantation (at 1mTx) between those who died (RD) and those who lost the graft (GL).
Table 5. Comparison of mean values of SBP and DBP measured by ABPM, mean values of SBP and DBP measured by ABPM during day (D) and during night (N) after 1 month after transplantation (at 1mTx) between those who died (RD) and those who lost the graft (GL). In Press
20 Mar 2024 : Original article
Transplant Nephrectomy: A Comparative Study of Timing and Techniques in a Single InstitutionAnn Transplant In Press; DOI: 10.12659/AOT.942252
28 Mar 2024 : Original article
Association Between FEV₁ Decline Rate and Mortality in Long-Term Follow-Up of a 21-Patient Pilot Clinical T...Ann Transplant In Press; DOI: 10.12659/AOT.942823
02 Apr 2024 : Original article
Liver Transplantation from Brain-Dead Donors with Hepatitis B or C in South Korea: A 2014-2020 Korean Organ...Ann Transplant In Press; DOI: 10.12659/AOT.943588
02 Apr 2024 : Original article
Effect of Dexmedetomidine Combined with Remifentanil on Emergence Agitation During Awakening from Sevoflura...Ann Transplant In Press; DOI: 10.12659/AOT.943281
Most Viewed Current Articles
05 Apr 2022 : Original article
Impact of Statins on Hepatocellular Carcinoma Recurrence After Living-Donor Liver TransplantationDOI :10.12659/AOT.935604
Ann Transplant 2022; 27:e935604
12 Jan 2022 : Original article
Risk Factors for Developing BK Virus-Associated Nephropathy: A Single-Center Retrospective Cohort Study of ...DOI :10.12659/AOT.934738
Ann Transplant 2022; 27:e934738
22 Nov 2022 : Original article
Long-Term Effects of Everolimus-Facilitated Tacrolimus Reduction in Living-Donor Liver Transplant Recipient...DOI :10.12659/AOT.937988
Ann Transplant 2022; 27:e937988
15 Mar 2022 : Case report
Combined Liver, Pancreas-Duodenum, and Kidney Transplantation for Patients with Hepatitis B Cirrhosis, Urem...DOI :10.12659/AOT.935860
Ann Transplant 2022; 27:e935860








