05 December 2023: Database Analysis
Survival Outcomes After Double-Lung Transplantation for Refractory Lung-Limited Cancers and Incidence of Post-Transplant Lung Cancer
Jeeyeon LeeDOI: 10.12659/AOT.941301
Ann Transplant 2023; 28:e941301
Abstract
BACKGROUND: To evaluate the role of double-lung transplantation (DLT) for lung cancer, the survival outcomes of patients who underwent DLT for lung cancer and the incidence of de novo lung cancer after DLT were assessed.
MATERIAL AND METHODS: Data from all cases reported in the literature were pooled for analysis and additional data were collected from the Organ Procurement Transplantation Network (OPTN) registry. Recurrence-free survival (RFS), overall survival (OS), and cancer-specific survival (CSS) of patients who underwent DLT for lung cancer were determined. Moreover, the incidence of de novo lung cancer and associated OS in lung transplant recipients were examined.
RESULTS: Of the 20 cases series and 15 cases from the OPTN registry, the 5-year RFS was 55.0% and 66.7% and the 5-year OS was 55.0% and 26.7%, respectively, and the median CSS was 48.0 (range, 2.0-144.0) and 27.7 (range, 0.2-66.6) months, respectively. In the OPTN data, the incidence of post-transplant lung cancer in patients who underwent DLT for the non-cancerous disease was 0.8% and the 5-year OS was 47.3%.
CONCLUSIONS: In conclusion, our integrated analysis of the case series and the OPTN registry demonstrated promising survival outcomes for patients with refractory bilateral lung cancer who underwent DLT. Although there are limitations to consider, the results of this study underscore the potential benefits of DLT in managing refractory lung-limited lung cancer.
Keywords: Lung Neoplasms, Lung Transplantation, Survival Analysis
Background
Since the first lung transplantation was attempted by Hardy and colleagues in 1963 for a patient with lung cancer [1], many advanced surgical techniques in lung transplantation have been developed for various lung diseases. According to the International Society of Heart and Lung Transplant (ISHLT) report, the most common indication of lung transplantation is chronic obstructive pulmonary disease, and double-lung transplantation (DLT) is almost 2 times more frequent than single-lung transplantation [2,3]. However, only 0.1% of the indications for lung transplantation were for lung cancer from 1995 to 2015 [2].
Although not widely available, lung transplantation may be one of the remaining treatment options for patients with refractory lung cancer or those with concomitant respiratory failure. The major concern regarding the application of lung transplantation in patients with lung cancer is the heightened risk of cancer recurrence attributed to the use of immunosuppressive treatment after transplantation. Additionally, the prevalence of postoperative complications may be amplified due to the extensive prior treatments received by these patients before undergoing transplantation [4–6]. Nevertheless, in some previous reports, the 5-year overall survival (OS) of patients receiving DLT for lung cancer was 39–57% [7,8], which is not inferior to the survival rate of 50–59% for patients with non-malignant disease [9–11]. Furthermore, although lung cancer is an unusual indication for lung transplantation, adenocarcinoma in situ (AIS) and minimally invasive adenocarcinoma (MIA) of the lung have been accepted as special disease considerations for lung transplantation when conventional medical treatments fail [12]. According to this guideline, if patients with lung cancer limited to the lung alone meet these criteria, they can be considered candidates for DLT. However, to date, the role of DLT in lung cancer has not been sufficiently elucidated.
To better understand the role of DLT for lung-limited cancers, we assessed the survival outcomes of patients who underwent DLT for lung cancer. Additionally, to understand the potential impact of immunosuppression in lung cancer progression, we investigated the incidence of de novo lung cancer following transplant and its impact on survival.
Material and Methods
In this study, only patients aged >18 years who underwent DLT for lung disease were included. We used the following datasets: 1) data pooled from published case series and 2) data obtained from Organ Procurement Transplantation Network (OPTN). This study was approved by the Institutional Review Board Committee of Northwestern University, Chicago, IL, USA (IRB#: STU00207117).
To evaluate the data pooled from the case series of DLT for lung cancer, we searched the literature using the terms “Lung cancer,” “Double or Bilateral,” and “Transplantation” in PubMed and Embase. After screening titles and abstracts, 74 related original or review articles and 26 case series were selected. Of 26 case series of lung transplantation for lung cancer, 18 were excluded because these patients had incidental cancer or lung metastasis in the explanted lungs. Subsequently, 6 reports of intentional DLT for primary lung cancer were manually identified, and data from each case were pooled to determine clinical and oncologic outcomes [7,13–17]. Additionally, the 3 cases of DLT performed at our institute for lung cancer to date as part of a clinical registry (double-lung transplant registry aimed for lung-limited malignancies – DREAM, NCT05671887) were included, and 20 cases were finally pooled (Supplementary Figure 1A).
The OPTN data were provided by United Network for Organ Sharing (UNOS) – a mission-driven non-profit organization serving as the nation’s transplant system under contract with the federal government (www.unos.org). The OPTN data were de-identified, anonymized, and presented with coding files as STATA format data files. Based on the data from the thoracic transplant registry of OPTN, until October 7, 2022, there were 29 335 cases of DLT conducted between 1993 and June 2022. Of these, the indications for DLT were lung cancer in 15 cases and non-cancerous disease in 29 320 cases (Supplementary Figure 1B).
Each dataset on DLT for lung cancer revealed the age of the patient during DLT, sex, smoking history, histology of tumor, type of DLT (sequential vs non-sequential), and use of cardiopulmonary bypass (CPB) during DLT surgery were collected and analyzed, separately. Survival outcomes were investigated with tumor recurrence, death, cause of death, and cancer-specific death. Moreover, from the OPTN registry, DLT for non-cancerous diseases revealed the incidence of post-transplant lung cancer, the period from the date of transplant to the date of occurrence of lung cancer, death, and survival rates.
We performed an assessment of annual and cumulative risks. Recurrence-free survival (RFS), OS, and cancer-specific survival (CSS) were examined using Kaplan-Meier survival curves. OS rates were compared between patients who underwent DLT for lung cancer and non-cancerous disease and between patients with and without post-transplant lung cancer. The RFS, OS, and CSS of each cohort were assessed at 3 and 5 years from DLT, and the median values of each survival parameter were calculated. The incidence of post-transplant lung cancer in the OPTN data was also calculated. All statistical analyses were performed using SPSS (version 29.0 SPSS, IBM, Chicago, IL, USA), and a
Results
RISKS FOR TUMOR RECURRENCE:
There were 9 cases (9/20, 45.0%) of tumor recurrence in the pooled case series and 5 cases each in the OPTN (5/15, 33.3%) (Figure 1A). Among the 9 cases of tumor recurrence in the pooled data, most tumors recurred in transplanted donor lungs (8/9, 88.9%), and only 1 case (1/9, 11.1%) recurred in the brain and bone simultaneously.
In the pooled case series, there was no association between recurrence of lung cancer and clinical factors, including age at transplantation, sex, smoking history, histology of tumor, and type of DLT. However, when the DLT was performed under CPB, the recurrence risk was significantly lower (P=0.016). In OPTN dataset, the age at transplantation, sex, and smoking history were not associated with tumor recurrence. Since the histologic type of tumor, type of DLT, and use of CPB in OPTN dataset showed the same result in all patients, statistical analysis was impossible to perform. Regarding death after DLT for lung cancer, there were no factors showing significant association in both datasets (Table 1).
SURVIVAL OUTCOMES:
Nine (45.0%) and 5 (33.3%) patients had experienced tumor recurrence after DLT for lung cancer in pooled case series and UNOS dataset, respectively, and 10 (50.0%) and 12 (80.0%) patients died during the follow-up period, respectively (Figure 1A). The median RFS was 2-fold longer in pooled case series than in UNOS data [pooled case series, 23.0 (range, 6.0–76.0) months; OPTN, 11.2 (range, 0.2–27.7) months]. Although the 3-year RFS rate was higher in pooled case series [pooled case series, 16/20 (80.0%); OPTN, 10/15 (66.7%)], the 5-year RFS rate was higher in OPTN data [pooled case series, 11/20 (55.0%); OPTN, 10/15 (66.7%)] (Table 2). However, there was no significant difference between the 2 groups (P=0.132) (Figure 1B).
In all datasets, the rates of CSS were higher than those of OS due to the presence of patients who died from causes other than cancer (Figure 2). In the analysis of pooled data, the 5-year CSS rate was 61.1% (11/18), with a median CSS of 48.0 (range, 2.0–144.0) months. However, the 5-year CSS rate in the OPTN dataset (3/7, 42.9%) was lower compared to the CSS rate in the pooled data (Table 2). Additionally, while there were 6 (6/10, 60.0%) cancer-related deaths in the pooled data, there were only 4 (4/12, 33.3%) cancer-related deaths in the OPTN data (Supplementary Table 1).
Although the OS of patients who underwent DLT for lung cancer was significantly lower in the OPTN registry compared to those with non-cancerous diseases (P<0.001), there was no significant difference in the OS of patients who underwent DLT for lung cancer in pooled cases compared to those with non-cancerous diseases in the OPTN registry (P=0.485) (Figure 3). The median OS was 38.0 (range, 2.0–144.0) months in pooled case series and 15.9 (range, 0.2–149.1) months in OPTN data, and the 3-year and 5-year OS rates were 70.0% (14/20) and 55.0% (11/20), respectively, in pooled case series. In the OPTN data, the 3-year and 5-year OS rates were 26.7% (4/15) and 20.0% (3/15), respectively.
DE NOVO LUNG CANCER AFTER DLT:
In OPTN data, there were 29,320 cases of patients who received DLT for non-cancerous disease. Among them, 220 cases (0.8%) had developed post-transplant lung cancer after DLT. The mean period to post-transplant lung cancer from transplantation in patients who received DLT for non-cancerous disease was 54.0 (SD, ±54.3) months. Post-transplant lung cancer was most frequently developed in the first 2 years (n=84) from the transplantation, and its incidence gradually decreased during the follow-up period (Figure 4A). Among 220 patients with post-transplant lung cancer after DLT, 205 patients (93.2%) had died and median OS was 51.3 (range, 0.9–352.8). The 3-year and 5-year OS of patients who had post-transplant lung cancer after DLT were 63.6% (140/220) and 47.3% (104/220), respectively (Table 3). However, during the 30 years of follow-up, the OS rate of patients with post-transplant lung cancer was significantly lower than those without post-transplant cancer (P<0.001) (Figure 4B).
Discussion
To the best of our knowledge, this is the first study to evaluate the comprehensive data related to the survival of patients who underwent DLT. The results of this study revealed the RFS, OS, and CSS of patients with lung cancer who underwent DLT as well as the incidence and survival outcomes of patients with post-transplant lung cancer after DLT for non-cancerous disease. Most oncologic outcomes, including recurrence and survival after DLT for lung cancer, were better in the pooled data compared with the OPTN data. This may be attributed to the fact that the pooled data have publication bias, which is defined as the failure to publish the results of research based on the direction or strength of study outcomes [18]. Therefore, based on the assumption that OPTN data are closer to the real-world data, the 3-year overall survival after DLT for lung cancer was almost 5–10 times higher than that of previously known stage IV lung cancer and 5–8 times higher than that of non-localized lung cancers [19–21]. Furthermore, the causes of death were varying, and we found that cancer-related deaths were only 33% in the OPTN data [22,23].
Although a consensus document for the selection of lung transplant candidates recommended that lung cancer may be a special consideration in cases of AIS or MIA of histological type and refractory to conventional medical treatments or those associated with respiratory failure [12], only 0.1% of lung transplantations have been performed for lung cancer during the last 2 decades [2]. However, the incidence of unexpected malignancy found in removed lungs after lung transplantation is approximately 2.2%, which is higher than the incidence of lung cancer as a primary indication for lung transplantation [21]. These findings indicate that the practice of excluding patients with a lung cancer diagnosis from lung transplantation should be reassessed. AIS and MIA, being localized forms of lung cancer, were specifically mentioned as potential considerations for lung transplant candidates in the consensus document [12]. However, if any type of lung cancer is confined to the lungs and can be completely removed, lung transplantation could be a treatment option, and this approach can be applied to both lungs, suggesting that DLT can also be considered for bilateral lung cancer. This rationale is similar to liver transplants being performed for primary hepatocarcinoma as well as metastatic hepatic disease from colorectal metastasis in current medical practice [24,25].
Another reason why physicians do not consider lung cancer as an indication for lung transplantation is that immunosuppressive management after lung transplantation may promote tumor recurrence and post-transplant malignancy. However, the 5-year RFS in the case series and OPTN dataset were approximately 52–80%, which is not lower than the known RFS of stage IV lung cancer [26,27]. Using the OPTN dataset, we observed significantly lower survival rates for patients with lung cancer compared to patients with non-cancerous disease when DLTs were indicated. However, analysis of the pooled data set showed no significant difference in survival for recipients of OPTN with non-cancerous diseases. Although one must be careful about publication bias, it is worth noting that a potential limitation of the OPTN data set is the lack of continuous long-term follow-up for each case. Therefore, it is hard to definitively conclude that the survival rate of lung cancer patients who received DLT is significantly lower than that of patients with non-cancerous diseases.
Furthermore, it is important to note that the actual 5-year CSS exceeded 40%, even if the reported 5-year OS rate in patients who received DLT for lung cancer was only 20% in OPTN data. This result indicates that many post-transplantation deaths were due to causes unrelated to cancer. Therefore, the notion that lung transplantation should not be considered due to concerns about cancer recurrence or progression warrants reconsideration. If patients with lung cancer could undergo transplantation earlier, rather than first undergoing multiple other invasive treatments, they would be better prepared for DLT, potentially leading to improved survival rates.
According to a systemic analysis of 21 studies, the risk of all cancers increased by 4.28 times (95% CI: 3.18–5.77;
When DLT is performed as a sequential procedure, generally CPB or extracorporeal membrane oxygenation (ECMO) are not necessary [30,31]. After one side of the lung is resected, the ipsilateral lung transplantation is performed while maintaining ventilation with the remaining lung, and the contralateral side of the lung is removed while maintaining ventilation with the transplanted lung. During each single-lung ventilation, the floating cells from the lung cancer can spread to or contaminate the bronchus, trachea, and the opposite side of the lung. If these cells are malignant, they can directly affect tumor recurrence or metastasis. This can be explained by the fact that most cases of recurrence of lung cancer are detected in the first implanted lung and demonstrate molecular patterns similar to the initial lung cancer [14,32]. Therefore, if DLT is planned for treating lung cancer, a non-sequential technique of excising both lungs using CPB or ECMO may be safer to prevent contamination with cancer cells during lung transplantation. Although sufficient information could not be obtained from the OPTN registry, the pooled analysis in our study demonstrated that the application of CPB significantly reduced tumor recurrence, and this result is consistent with the previously mentioned theory.
This study determined that there are reasonable survival outcomes for patients receiving DLT for lung cancer, based on a survival outcomes study using pooled data and dataset provided by OPTN. However, as a limitation of this study, it is not possible to directly distinguish the duplications between the 2 cohorts due to the anonymization of the provided datasets. Assuming that all organ transplant patients are recorded in the OPTN data, all cases except for 2 could potentially overlap with the OPTN dataset. Another limitation may exist in selection of best candidates for DLT. While histological and imaging techniques have advanced, there remain inherent limitations in determining lung-limited cancer. Even when histological assessments indicate lung-limited cancer, there is a possibility that penetrated parts may exist in areas not biopsied. To address these limitations, more advanced biopsy techniques can be applied, such as endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA), for biopsy. It is also essential to meticulously verify that the results obtained are consistent. Physicians will only consider a candidate for DLT if both the histological and imaging results are consistent, and this consensus should be achieved through multidisciplinary treatment.
Conclusions
The CSS of patients who received DLT for bilateral lung cancer was similar to that of patients with de novo lung cancer after DLT. Moreover, CSS was higher than OS in both datasets. In conclusion, based on the reasonable survival outcomes of patients receiving DLT for lung cancer, we propose that DLT could be one of the treatment options for lung-limited cancer. Further prospective studies are required to evaluate the risk of de novo lung cancer in patients undergoing DLT for bilateral lung cancer to better determine the role of DLT in medically refractory lung-limited cancers.
Figures
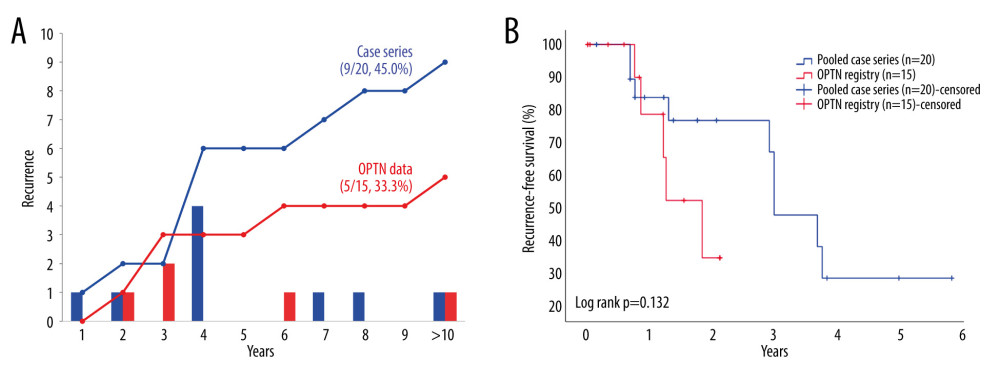 Figure 1. Outcomes of tumor recurrence after double-lung transplantation for lung cancer in pooled case series and Organ Procurement Transplantation Network (OPTN). (A) Incidence of tumor recurrence after double-lung transplantation for lung cancer, (B) Recurrence-free survival after double-lung transplantation for lung cancer. Created using Microsoft Excel 2021.
Figure 1. Outcomes of tumor recurrence after double-lung transplantation for lung cancer in pooled case series and Organ Procurement Transplantation Network (OPTN). (A) Incidence of tumor recurrence after double-lung transplantation for lung cancer, (B) Recurrence-free survival after double-lung transplantation for lung cancer. Created using Microsoft Excel 2021. 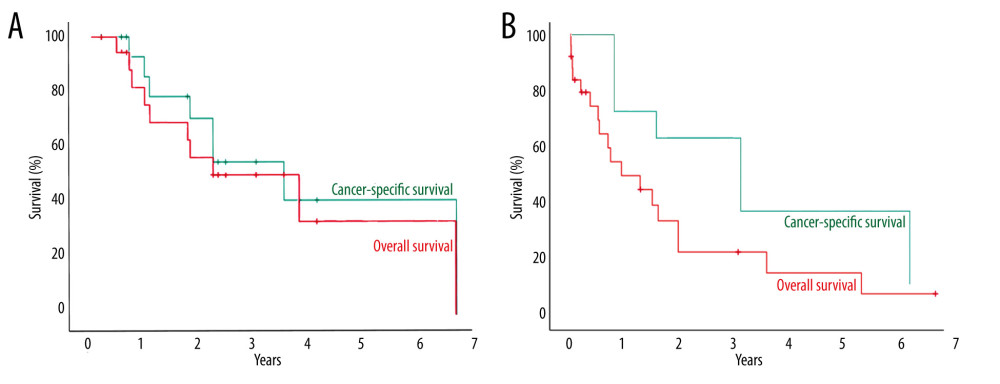 Figure 2. Overall and cancer-specific survival of patients who received double-lung transplantation for lung cancer from pooled case series (A) and from Organ Procurement Transplantation Network (OPTN) registry (B). SPSS, Inc. SPSS version 29.0, IBM, Chicago, IL, USA.
Figure 2. Overall and cancer-specific survival of patients who received double-lung transplantation for lung cancer from pooled case series (A) and from Organ Procurement Transplantation Network (OPTN) registry (B). SPSS, Inc. SPSS version 29.0, IBM, Chicago, IL, USA. 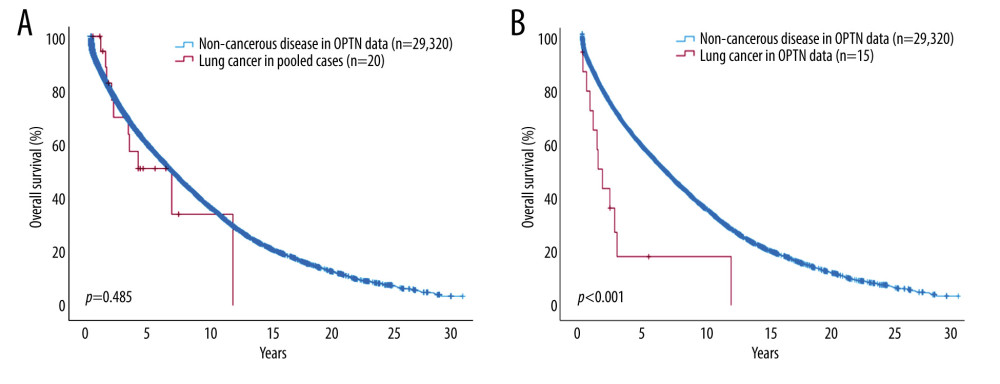 Figure 3. Comparison of overall survival between patients who received double-lung transplantation for lung cancer and for non-cancerous lung disease. (A) Overall survival of patients who received double-lung transplantation for lung cancer in pooled cases and for non-cancerous lung disease in Organ Procurement Transplantation Network (OPTN) registry. (B) Overall survival between patients who received double-lung transplantation for lung cancer and non-cancerous lung disease in OPTN registry. SPSS Inc. SPSS version 29.0, IBM, Chicago, IL, USA.
Figure 3. Comparison of overall survival between patients who received double-lung transplantation for lung cancer and for non-cancerous lung disease. (A) Overall survival of patients who received double-lung transplantation for lung cancer in pooled cases and for non-cancerous lung disease in Organ Procurement Transplantation Network (OPTN) registry. (B) Overall survival between patients who received double-lung transplantation for lung cancer and non-cancerous lung disease in OPTN registry. SPSS Inc. SPSS version 29.0, IBM, Chicago, IL, USA. 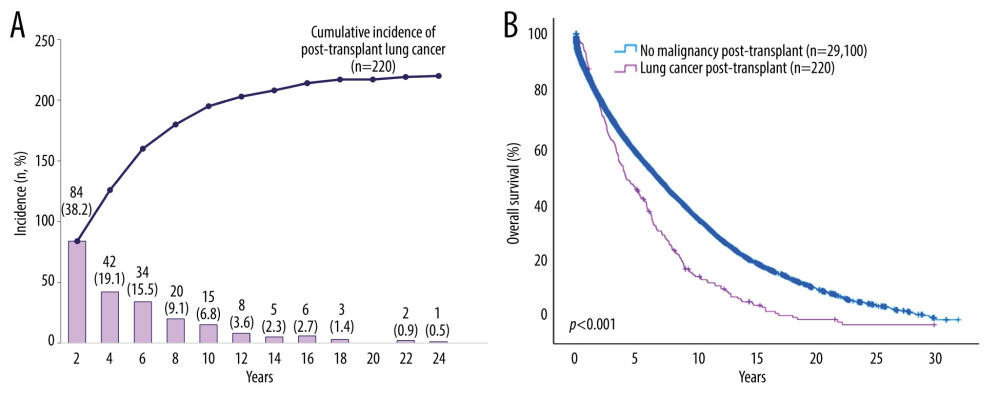 Figure 4. Incidence of post-transplant lung cancer and overall survival (OS) of patients who received double-lung transplantation (DLT) from OPTN data. (A) Annual and cumulative incidence of post-transplant lung cancer in patients who underwent DLT for non-cancerous disease. (B) Comparison of OS between patients with and without post-transplant lung cancer after DLT for non-cancerous disease. Created using Microsoft Excel 2021 and SPSS, Inc. SPSS version 29.0, IBM, Chicago, IL, USA.
Figure 4. Incidence of post-transplant lung cancer and overall survival (OS) of patients who received double-lung transplantation (DLT) from OPTN data. (A) Annual and cumulative incidence of post-transplant lung cancer in patients who underwent DLT for non-cancerous disease. (B) Comparison of OS between patients with and without post-transplant lung cancer after DLT for non-cancerous disease. Created using Microsoft Excel 2021 and SPSS, Inc. SPSS version 29.0, IBM, Chicago, IL, USA. Tables
Table 1. Cancer-related factors in patients who received double-lung transplantation (DLT) for lung cancer from case series, Organ Procurement Transplantation Network (OPTN) registry.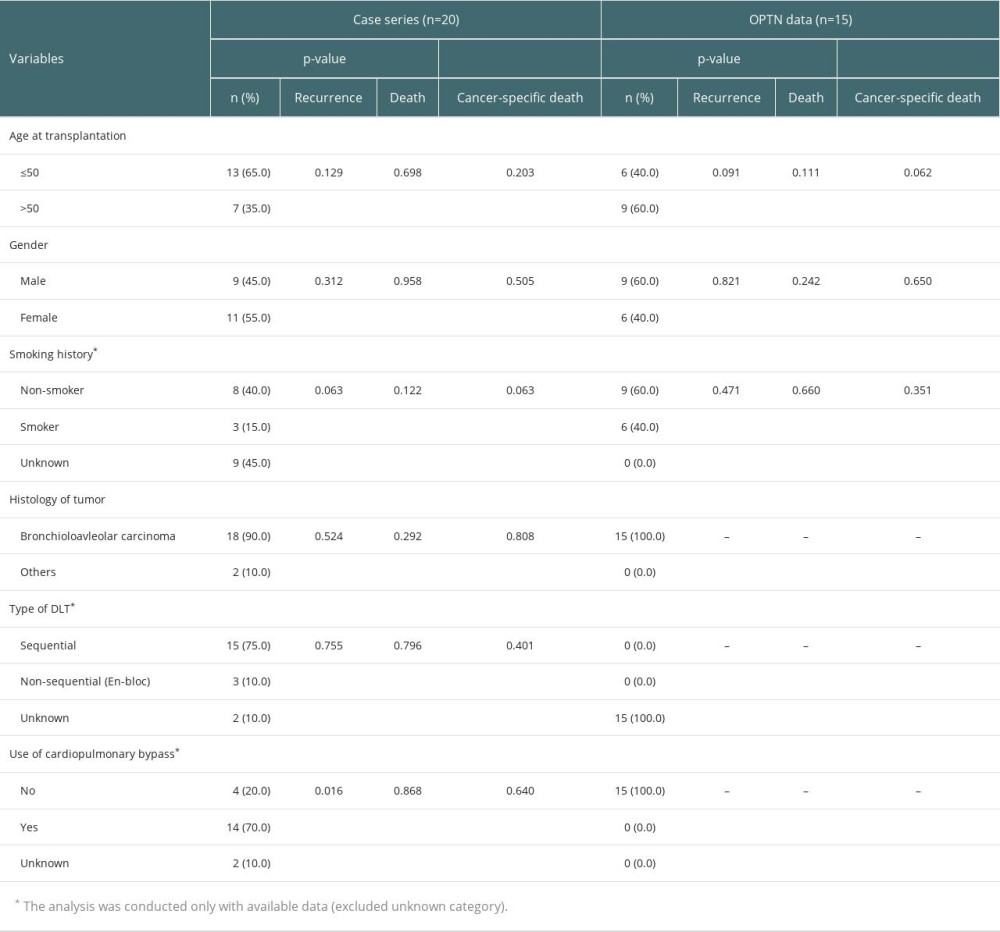 Table 2. Comparison of survivals in patients who received double-lung transplantation for lung cancer between case series and data from Organ Procurement Transplantation Network (OPTN).
Table 2. Comparison of survivals in patients who received double-lung transplantation for lung cancer between case series and data from Organ Procurement Transplantation Network (OPTN).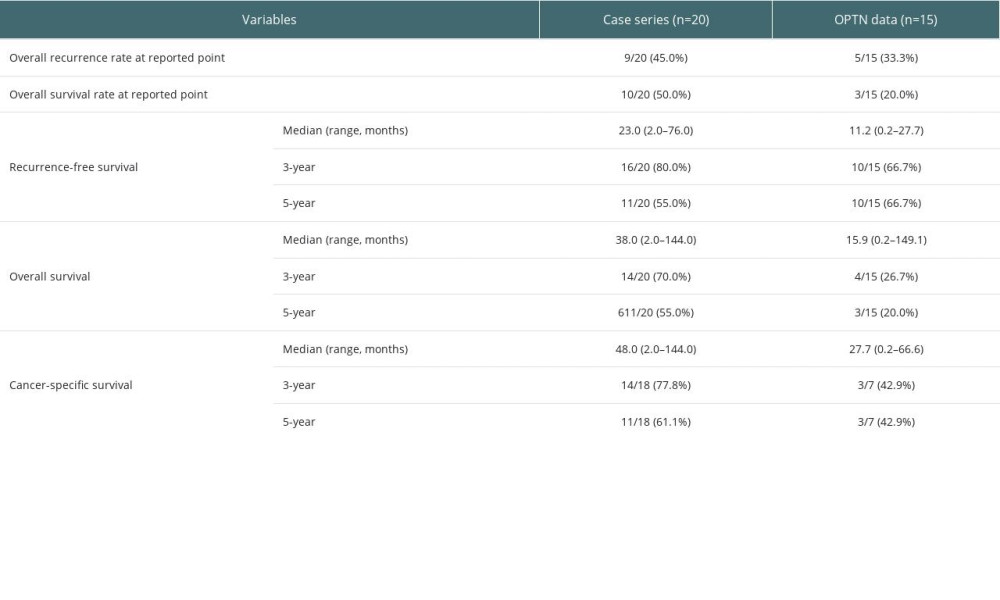 Table 3. Clinical characteristics in patients who received double-lung transplantation (DLT) for non-cancerous disease from Organ Procurement Transplantation Network (OPTN) registry.
Table 3. Clinical characteristics in patients who received double-lung transplantation (DLT) for non-cancerous disease from Organ Procurement Transplantation Network (OPTN) registry.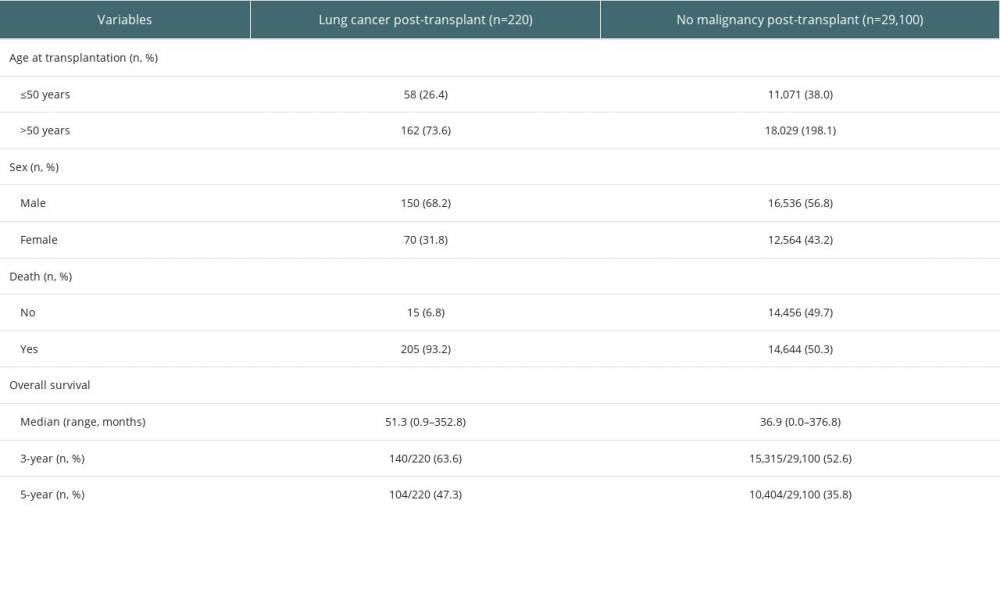 Supplementary Table 1. Cause of death in patients who received double-lung transplantation for lung cancer in pooled analysis and Organ Procurement Transplantation Network (OPTN) registry.
Supplementary Table 1. Cause of death in patients who received double-lung transplantation for lung cancer in pooled analysis and Organ Procurement Transplantation Network (OPTN) registry.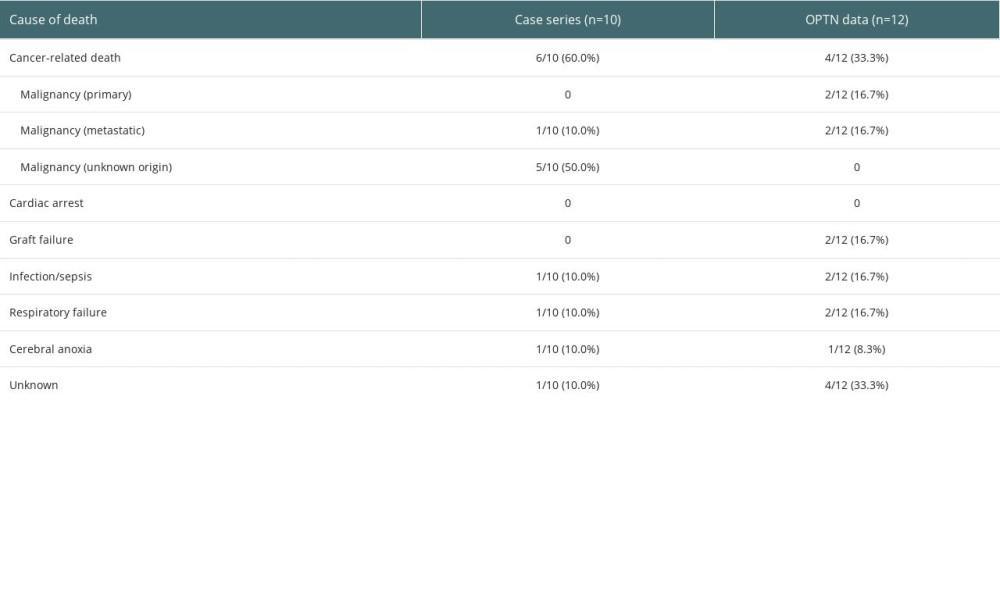
References
1. Hardy JD, Webb WR, Dalton ML, Walker GR, Lung homotransplantation in man: JAMA, 1963; 186; 1065-74
2. Yusen RD, Edwards LB, Dipchand AIInternational Society for Heart and Lung Transplantation, The Registry of the International Society for Heart and Lung Transplantation: Thirty-third adult lung and heart-lung transplant report – 2016; Focus theme: Primary diagnostic indications for transplant: J Heart Lung Transplant, 2016; 35(10); 1170-84
3. Chambers DC, Perch M, Zuckermann AInternational Society for Heart and Lung Transplantation., The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Thirty-eighth adult lung transplantation report – 2021; Focus on recipient characteristics: J Heart Lung Transplant, 2021; 40(10); 1060-72
4. Weill D, Lung transplantation: indications and contraindications: J Thorac Dis, 2018; 10(7); 4574-87
5. Mathew J, Kratzke RA, Lung cancer and lung transplantation: A review: J Thorac Oncol, 2009; 4(6); 753-60
6. Shtraichman O, Ahya VN, Malignancy after lung transplantation: Ann Transl Med, 2020; 8(6); 416
7. Zorn GL, McGiffin DC, Young KR, Pulmonary transplantation for advanced bronchioloalveolar carcinoma: J Thorac Cardiovasc Surg, 2003; 125(1); 45-48
8. de Perrot M, Chernenko S, Waddell TK, Role of lung transplantation in the treatment of bronchogenic carcinomas for patients with end-stage pulmonary disease: J Clin Oncol, 2004; 22(21); 4351-56
9. Jung F, Riley L, Lascano J, Outcomes and survival following lung transplantation in non-cystic fibrosis bronchiectasis: ERJ Open Res, 2022; 8(1); 00607-2021
10. Bos S, Vos R, Van Raemdonck DE, Verleden GM, Survival in adult lung transplantation: Where are we in 2020?: Curr Opin Organ Transplant, 2020; 25(3); 268-73
11. Riley L, Lascano J, Clinical outcomes and survival following lung transplantation in patients with Alpha-1 antitrypsin deficiency: Respir Med, 2020; 172; 106145
12. Weill D, Benden C, Corris PA, A consensus document for the selection of lung transplant candidates: 2014 – an update from the Pulmonary Transplantation Council of the International Society for Heart and Lung Transplantation: J Heart Lung Transplant, 2015; 34(1); 1-15
13. Etienne B, Bertocchi M, Gamondes JP, Successful double-lung transplantation for bronchioalveolar carcinoma: Chest, 1997; 112(5); 1423-24
14. Garver RI, Zorn GL, Wu X, Recurrence of bronchioloalveolar carcinoma in transplanted lungs: N Engl J Med, 1999; 340(14); 1071-74
15. Paloyan EB, Swinnen LJ, Montoya A, Lung transplantation for advanced bronchioloalveolar carcinoma confined to the lungs: Transplantation, 2000; 69(11); 2446-48
16. Wang Y, Wei D, Wang Z, Bilateral lung transplant for bronchioloalveolar carcinoma: First case in China: Exp Clin Transplant, 2012; 10(5); 519-21
17. Zhang-Velten ER, Gerber DE, Westover KD, Thirteen-year survival in a patient with diffuse bilateral lepidic-predominant adenocarcinoma: A case report of lung transplantation and local salvage: JTO Clin Res Rep, 2020; 1(4); 100094
18. Macaskill P, Walter SD, Irwig L, A comparison of methods to detect publication bias in meta-analysis: Stat Med, 2001; 20(4); 641-54
19. Amin MB, Greene FL, Edge SB, The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging: Cancer J Clin, 2017; 67(2); 93-99
20. Yang L, Wang S, Zhou Y: Oncotarget, 2017; 8(40); 66784-95
21. Amratia DA, Hunt WR, Neujahr D, Veeraraghavan S, Incidentally detected malignancies in lung transplant explants: Transplant Direct, 2019; 5(11); e503
22. Studer SM, Levy RD, McNeil K, Orens JB, Lung transplant outcomes: A review of survival, graft function, physiology, health-related quality of life and cost-effectiveness: Eur Respir J, 2004; 24(4); 674-85
23. Søborg A, Reekie J, Rasmussen A, Trends in underlying causes of death in solid organ transplant recipients between 2010 and 2020: Using the CLASS method for determining specific causes of death: PLoS One, 2022; 17(7); e0263210
24. Bonney GK, Chew CA, Lodge P, Liver transplantation for non-resectable colorectal liver metastases: The International Hepato-Pancreato-Biliary Association consensus guidelines: Lancet Gastroenterol Hepatol, 2021; 6(11); 933-46 Erratum in: Lancet Gastroenterol Hepatol. 2021;6(11):e7
25. Verna EC, Patel YA, Aggarwal A, Liver transplantation for hepatocellular carcinoma: Management after the transplant: Am J Transplant, 2020; 20(2); 333-47
26. Garon EB, Ciuleanu TE, Arrieta O, Ramucirumab plus docetaxel versus placebo plus docetaxel for second-line treatment of stage IV non-small-cell lung cancer after disease progression on platinum-based therapy (REVEL): A multicentre, double-blind, randomised phase 3 trial: Lancet, 2014; 384(9944); 665-73
27. Reck M, Kaiser R, Mellemgaard ALUME-Lung 1 Study Group, Docetaxel plus nintedanib versus docetaxel plus placebo in patients with previously treated non-small-cell lung cancer (LUME-Lung 1): A phase 3, double-blind, randomised controlled trial: Lancet Oncol, 2014; 15(2); 143-55
28. Ge F, Li C, Xu X, Huo Z, Cancer risk in heart or lung transplant recipients: A comprehensive analysis of 21 prospective cohorts: Cancer Med, 2020; 9(24); 9595-610
29. Lee J, Yang AWJ, Chung LI, A comprehensive landscape of de novo malignancy after double lung transplantation: Transpl Int, 2023; 36; 11552
30. Szeto WY, Kreisel D, Karakousis GC, Cardiopulmonary bypass for bilateral sequential lung transplantation in patients with chronic obstructive pulmonary disease without adverse effect on lung function or clinical outcome: J Thorac Cardiovasc Surg, 2002; 124(2); 241-49
31. Hayanga JW, D’Cunha J, The surgical technique of bilateral sequential lung transplantation: J Thorac Dis, 2014; 6(8); 1063-69
32. Gómez-Román JJ, Del Valle CE, Zarrabeitia MT, Recurrence of bronchioloalveolar carcinoma in donor lung after lung transplantation: Microsatellite analysis demonstrates a recipient origin: Pathol Int, 2005; 55(9); 580-84
Figures
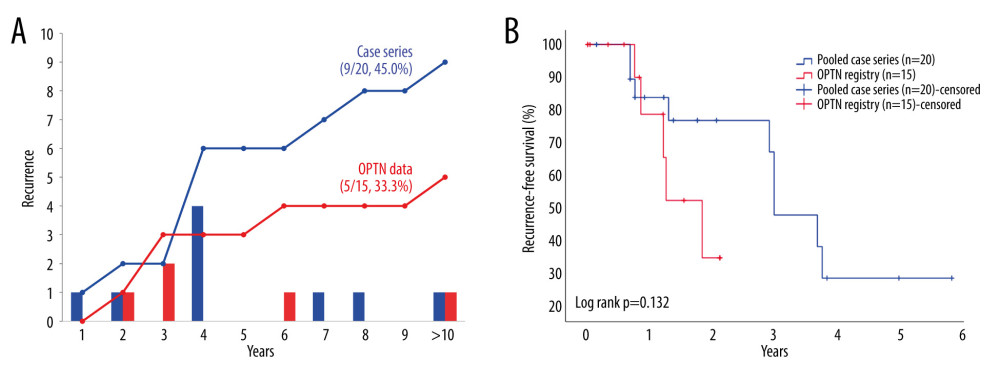 Figure 1. Outcomes of tumor recurrence after double-lung transplantation for lung cancer in pooled case series and Organ Procurement Transplantation Network (OPTN). (A) Incidence of tumor recurrence after double-lung transplantation for lung cancer, (B) Recurrence-free survival after double-lung transplantation for lung cancer. Created using Microsoft Excel 2021.
Figure 1. Outcomes of tumor recurrence after double-lung transplantation for lung cancer in pooled case series and Organ Procurement Transplantation Network (OPTN). (A) Incidence of tumor recurrence after double-lung transplantation for lung cancer, (B) Recurrence-free survival after double-lung transplantation for lung cancer. Created using Microsoft Excel 2021.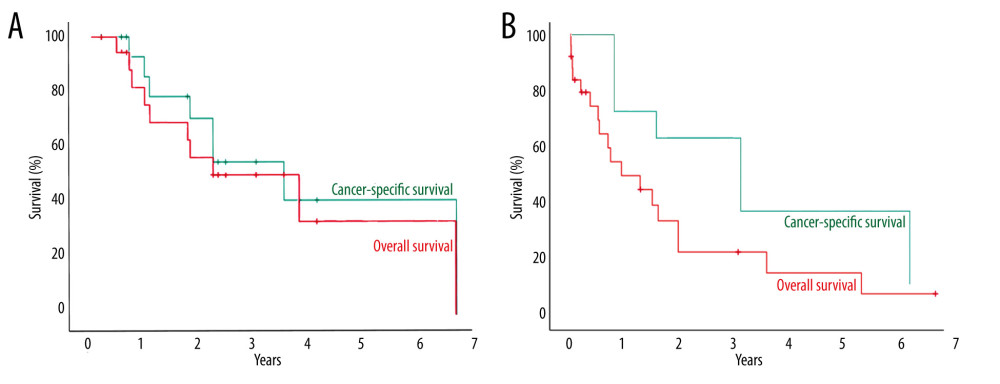 Figure 2. Overall and cancer-specific survival of patients who received double-lung transplantation for lung cancer from pooled case series (A) and from Organ Procurement Transplantation Network (OPTN) registry (B). SPSS, Inc. SPSS version 29.0, IBM, Chicago, IL, USA.
Figure 2. Overall and cancer-specific survival of patients who received double-lung transplantation for lung cancer from pooled case series (A) and from Organ Procurement Transplantation Network (OPTN) registry (B). SPSS, Inc. SPSS version 29.0, IBM, Chicago, IL, USA.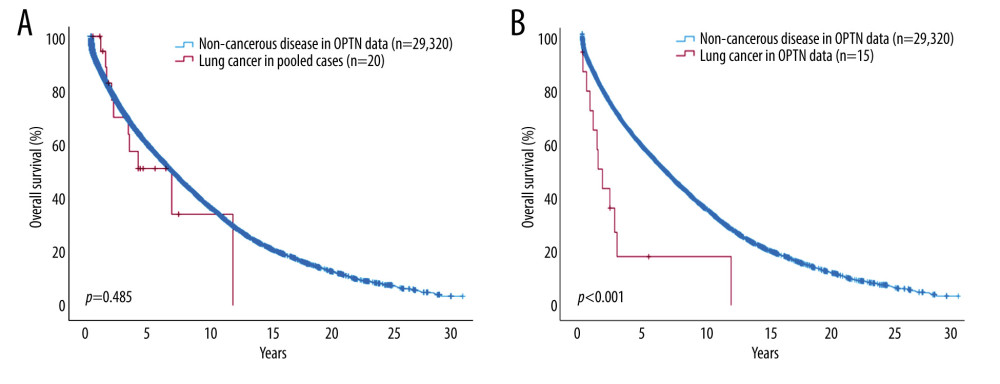 Figure 3. Comparison of overall survival between patients who received double-lung transplantation for lung cancer and for non-cancerous lung disease. (A) Overall survival of patients who received double-lung transplantation for lung cancer in pooled cases and for non-cancerous lung disease in Organ Procurement Transplantation Network (OPTN) registry. (B) Overall survival between patients who received double-lung transplantation for lung cancer and non-cancerous lung disease in OPTN registry. SPSS Inc. SPSS version 29.0, IBM, Chicago, IL, USA.
Figure 3. Comparison of overall survival between patients who received double-lung transplantation for lung cancer and for non-cancerous lung disease. (A) Overall survival of patients who received double-lung transplantation for lung cancer in pooled cases and for non-cancerous lung disease in Organ Procurement Transplantation Network (OPTN) registry. (B) Overall survival between patients who received double-lung transplantation for lung cancer and non-cancerous lung disease in OPTN registry. SPSS Inc. SPSS version 29.0, IBM, Chicago, IL, USA.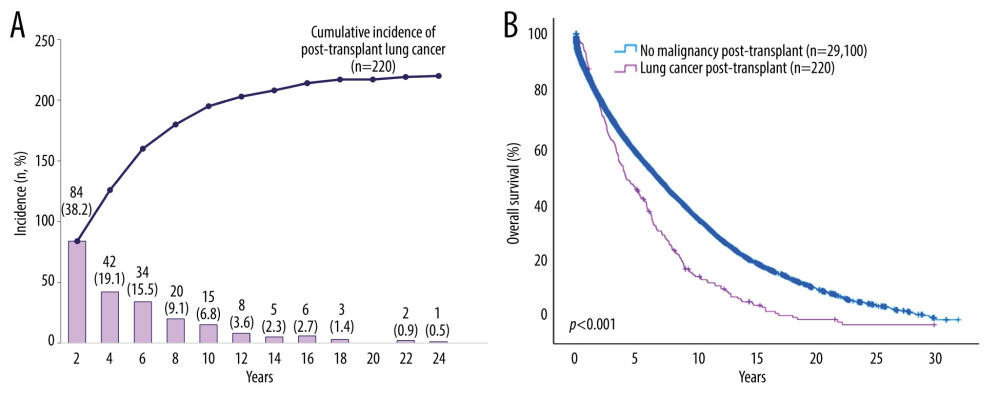 Figure 4. Incidence of post-transplant lung cancer and overall survival (OS) of patients who received double-lung transplantation (DLT) from OPTN data. (A) Annual and cumulative incidence of post-transplant lung cancer in patients who underwent DLT for non-cancerous disease. (B) Comparison of OS between patients with and without post-transplant lung cancer after DLT for non-cancerous disease. Created using Microsoft Excel 2021 and SPSS, Inc. SPSS version 29.0, IBM, Chicago, IL, USA.
Figure 4. Incidence of post-transplant lung cancer and overall survival (OS) of patients who received double-lung transplantation (DLT) from OPTN data. (A) Annual and cumulative incidence of post-transplant lung cancer in patients who underwent DLT for non-cancerous disease. (B) Comparison of OS between patients with and without post-transplant lung cancer after DLT for non-cancerous disease. Created using Microsoft Excel 2021 and SPSS, Inc. SPSS version 29.0, IBM, Chicago, IL, USA. Tables
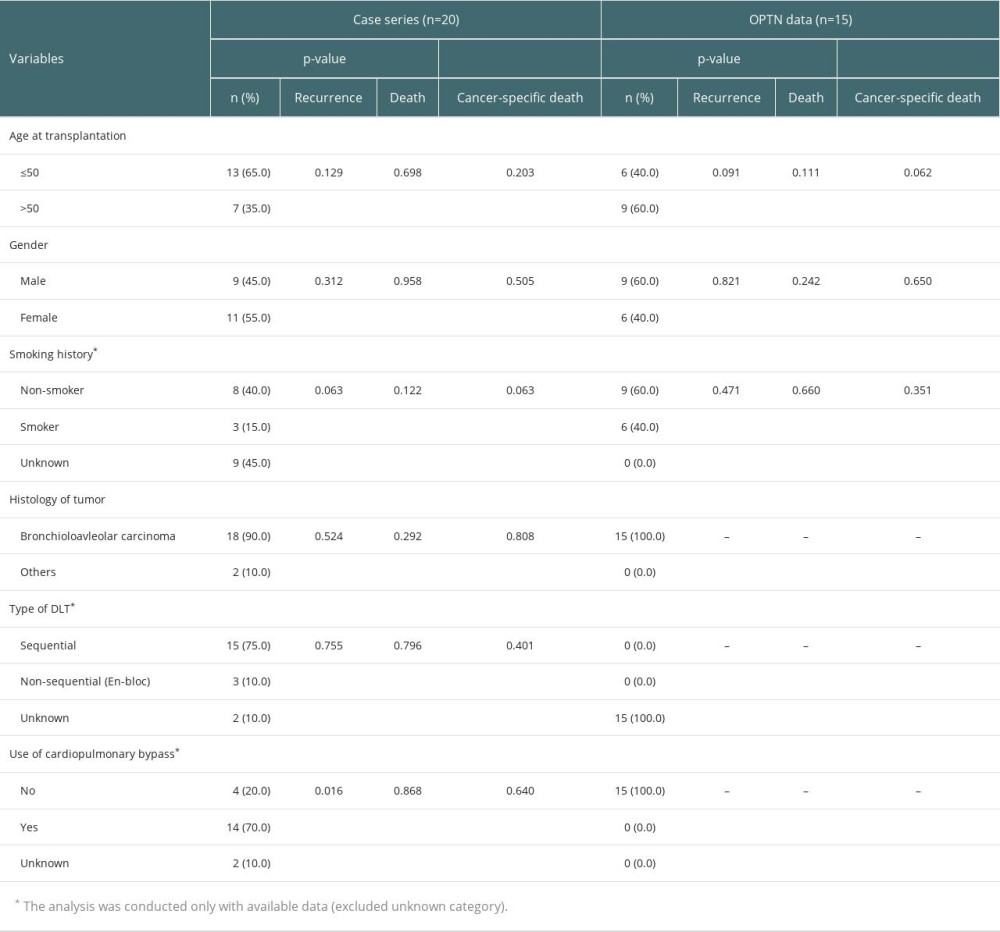 Table 1. Cancer-related factors in patients who received double-lung transplantation (DLT) for lung cancer from case series, Organ Procurement Transplantation Network (OPTN) registry.
Table 1. Cancer-related factors in patients who received double-lung transplantation (DLT) for lung cancer from case series, Organ Procurement Transplantation Network (OPTN) registry.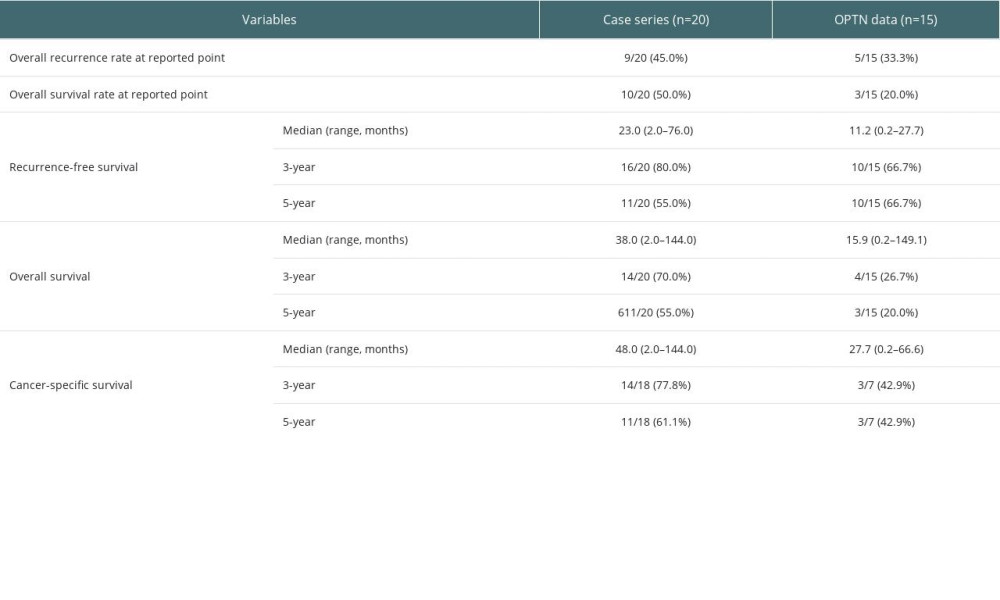 Table 2. Comparison of survivals in patients who received double-lung transplantation for lung cancer between case series and data from Organ Procurement Transplantation Network (OPTN).
Table 2. Comparison of survivals in patients who received double-lung transplantation for lung cancer between case series and data from Organ Procurement Transplantation Network (OPTN).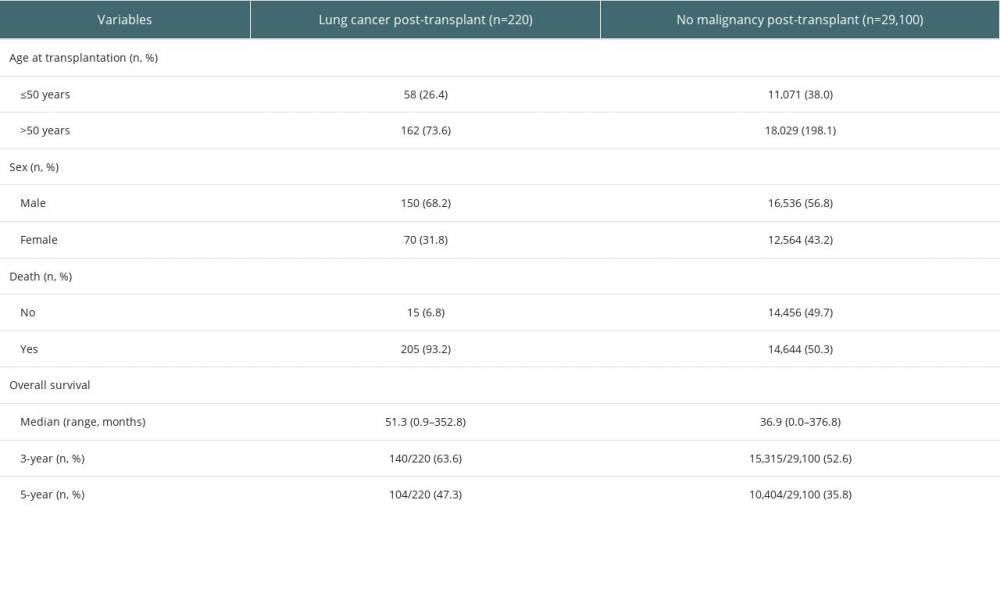 Table 3. Clinical characteristics in patients who received double-lung transplantation (DLT) for non-cancerous disease from Organ Procurement Transplantation Network (OPTN) registry.
Table 3. Clinical characteristics in patients who received double-lung transplantation (DLT) for non-cancerous disease from Organ Procurement Transplantation Network (OPTN) registry.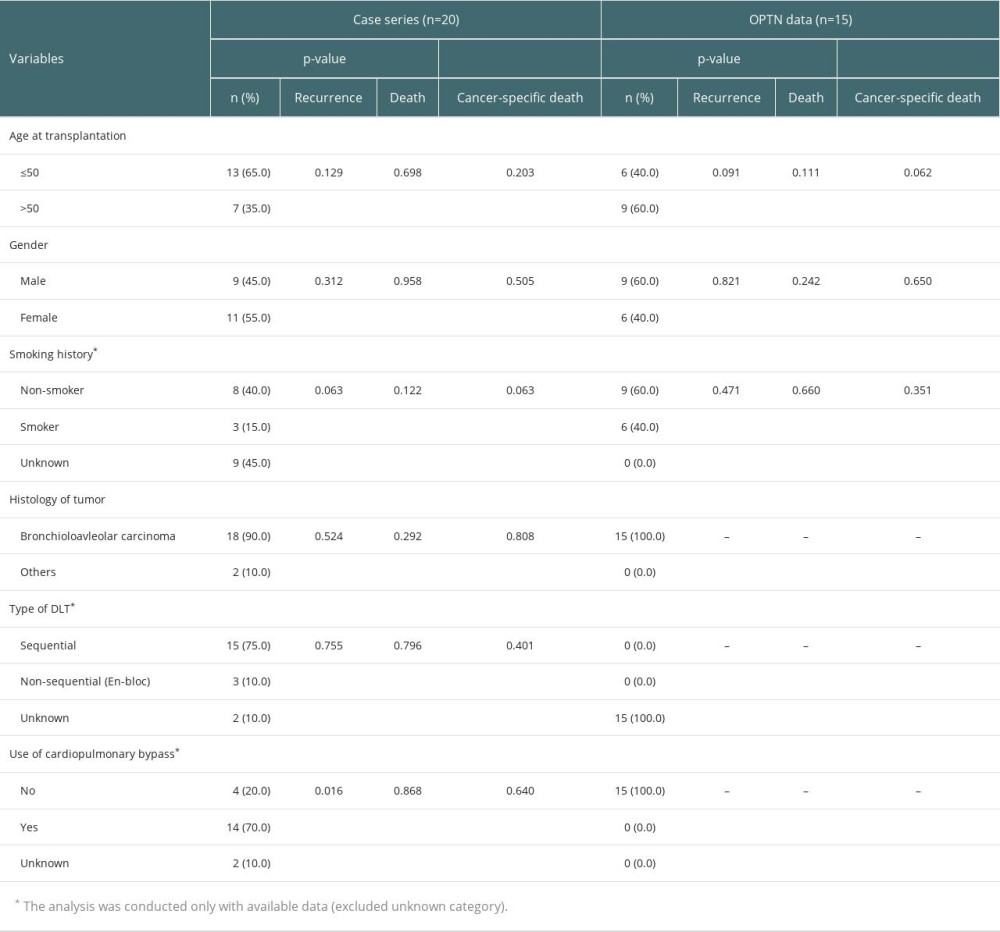 Table 1. Cancer-related factors in patients who received double-lung transplantation (DLT) for lung cancer from case series, Organ Procurement Transplantation Network (OPTN) registry.
Table 1. Cancer-related factors in patients who received double-lung transplantation (DLT) for lung cancer from case series, Organ Procurement Transplantation Network (OPTN) registry.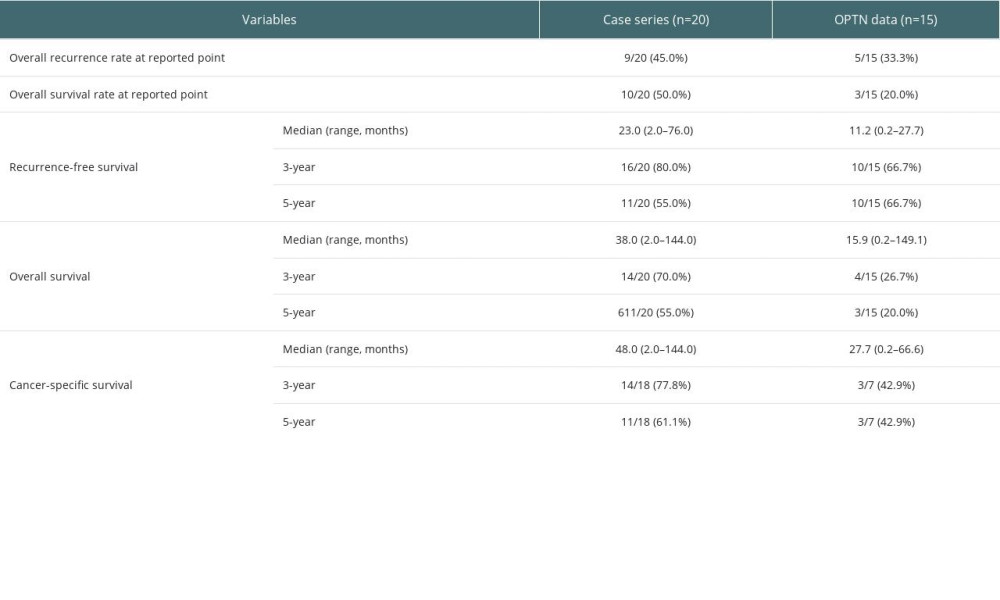 Table 2. Comparison of survivals in patients who received double-lung transplantation for lung cancer between case series and data from Organ Procurement Transplantation Network (OPTN).
Table 2. Comparison of survivals in patients who received double-lung transplantation for lung cancer between case series and data from Organ Procurement Transplantation Network (OPTN).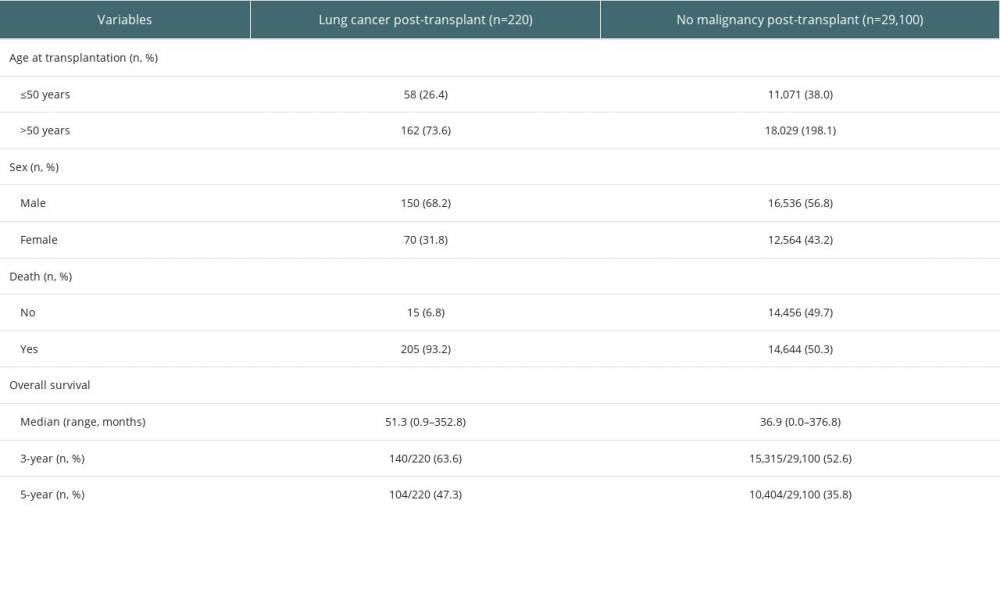 Table 3. Clinical characteristics in patients who received double-lung transplantation (DLT) for non-cancerous disease from Organ Procurement Transplantation Network (OPTN) registry.
Table 3. Clinical characteristics in patients who received double-lung transplantation (DLT) for non-cancerous disease from Organ Procurement Transplantation Network (OPTN) registry.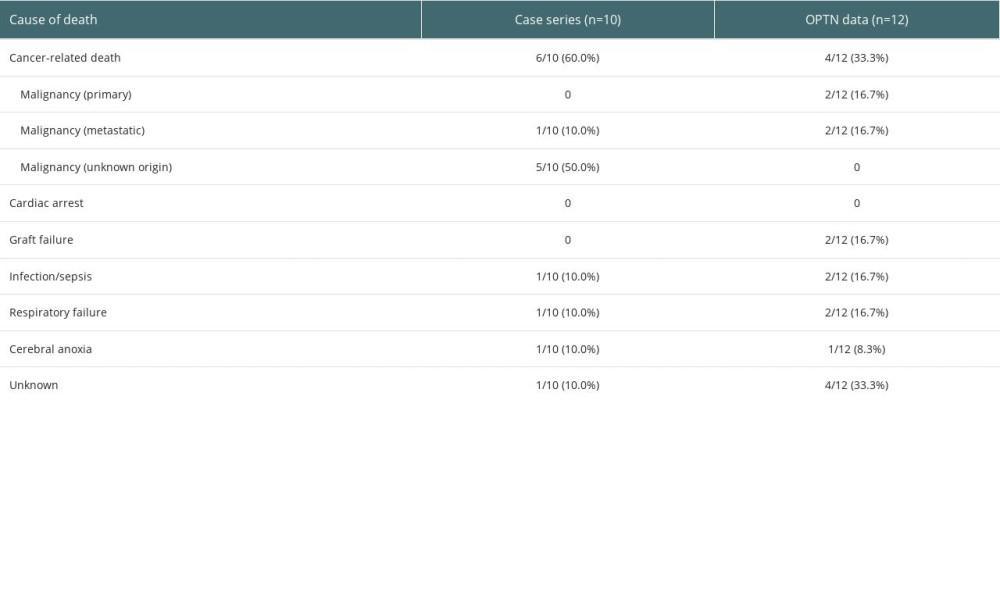 Supplementary Table 1. Cause of death in patients who received double-lung transplantation for lung cancer in pooled analysis and Organ Procurement Transplantation Network (OPTN) registry.
Supplementary Table 1. Cause of death in patients who received double-lung transplantation for lung cancer in pooled analysis and Organ Procurement Transplantation Network (OPTN) registry. In Press
20 Mar 2024 : Original article
Transplant Nephrectomy: A Comparative Study of Timing and Techniques in a Single InstitutionAnn Transplant In Press; DOI: 10.12659/AOT.942252
28 Mar 2024 : Original article
Association Between FEV₁ Decline Rate and Mortality in Long-Term Follow-Up of a 21-Patient Pilot Clinical T...Ann Transplant In Press; DOI: 10.12659/AOT.942823
02 Apr 2024 : Original article
Liver Transplantation from Brain-Dead Donors with Hepatitis B or C in South Korea: A 2014-2020 Korean Organ...Ann Transplant In Press; DOI: 10.12659/AOT.943588
02 Apr 2024 : Original article
Effect of Dexmedetomidine Combined with Remifentanil on Emergence Agitation During Awakening from Sevoflura...Ann Transplant In Press; DOI: 10.12659/AOT.943281
Most Viewed Current Articles
05 Apr 2022 : Original article
Impact of Statins on Hepatocellular Carcinoma Recurrence After Living-Donor Liver TransplantationDOI :10.12659/AOT.935604
Ann Transplant 2022; 27:e935604
12 Jan 2022 : Original article
Risk Factors for Developing BK Virus-Associated Nephropathy: A Single-Center Retrospective Cohort Study of ...DOI :10.12659/AOT.934738
Ann Transplant 2022; 27:e934738
22 Nov 2022 : Original article
Long-Term Effects of Everolimus-Facilitated Tacrolimus Reduction in Living-Donor Liver Transplant Recipient...DOI :10.12659/AOT.937988
Ann Transplant 2022; 27:e937988
15 Mar 2022 : Case report
Combined Liver, Pancreas-Duodenum, and Kidney Transplantation for Patients with Hepatitis B Cirrhosis, Urem...DOI :10.12659/AOT.935860
Ann Transplant 2022; 27:e935860








