10 August 2021: Original Paper
The Low Utilization Rate of Donor Lungs in China: A Single-Center Experience
Jin Zhao1ABCEF, Dong Liu1AB, Jian Huang1B, Hua-chi Jiang1B, Yuan Chen1B, Hui-xing Li1B, Xiao-shan Li2CD, Jing-yu Chen1AG*DOI: 10.12659/AOT.931409
Ann Transplant 2021; 26:e931409
Abstract
BACKGROUND: Despite the increasing number of organ donations, the utilization rate of donor lungs in China is much lower than that in many other countries.
MATERIAL AND METHODS: The donor lungs were evaluated before departure (stage 1), after on-site management (stage 2), and after harvesting (stage 3). Variables of donor lungs from medical institutions with lung transplant qualification (group A) and those without qualification (group B) were compared. The outcome measurements for lung recipients were early survival and primary graft dysfunction.
RESULTS: Among the 277 donor lungs, 140 (51%) were suitable for transplantation and 101 were sent to our institution for 62 single-lung transplantations and 50 double-lung transplantations. The acceptability rates at stage 1, stage 2, and stage 3 were 78%, 56%, and 51%, respectively. In addition, 69 (50.4%) donor lungs were abandoned for poor quality related to management, 24 (17.5%) for no adequate recipients, 15 (10.9%) for family refusal, 14 (10.2%) for organ procurement organization-related reasons, and 15 (10.9%) for other reasons. Donors in group A were ventilated longer and had longer ischemic time than those in group B. However, bronchoscopy, imaging, and oxygenation in group A achieved better results than in group B. No between-group difference in 30-day mortality or rate of grade 3 primary graft dysfunction was observed.
CONCLUSIONS: Problems at supply and demand ends contribute to the low utilization rate of donor lungs in China. The poor management of donor lungs and the short waiting list for lung transplantation are major reasons.
Keywords: Lung Transplantation, Tissue and Organ Procurement, Utilization Review, Lung, Primary Graft Dysfunction, Tissue Donors
Background
Lung transplantation has benefited thousands of patients with end-stage lung disease [1]. However, many patients still die each year while waiting for lung transplants [2]. Previously, inadequate organ donation constrained the availability of transplantation. However, many countries have reported robust organ donation, as people’s awareness of donation has increased in recent years [3].
In China, since January 1, 2015, the community-based organ donation system has become the only legitimate source of transplantable organs [4], and the annual growth rate of deceased organ donation has shown an upward trend. In 2018, a total of 6302 donors of deceased donation were recorded in the mainland of China, which occupied second place worldwide in terms of quantity [5], ushering in a period of rapid development of organ transplantation [6].
From 2015 to 2018, the China Lung Transplantation Registry reported 1024 cases of lung transplantation, including 118 cases in 2015, 204 cases in 2016, 299 cases in 2017, and 403 cases in 2018 [7]. However, considering China’s huge population, the number of lung transplants per year is still small, and the lung conversion rate was only 6.4% in 2018, which was significantly lower than that of many other countries [3] (Table 1). What currently limits lung transplantation in China is the poor conversion from donor lungs to transplantable lungs [8].
We performed this retrospective study on 277 donor lungs offered by the China Lung Transplantation Registry to the Wuxi Lung Transplant Center between June 1, 2018, and April 30, 2019, to analyze the low utilization rate of donor lungs by examining the causes of donor unsuitability at 3 stages of the donor lung assessment (before departure, after on-site management, and after harvesting), donor lung acceptance rates in different donor hospitals, postoperative complications, and survival rates of recipients.
Material and Methods
ETHICS APPROVAL:
This study was approved by the Medical Ethics Committee of Nanjing Medical University, Nanjing, Jiangsu, China. Written informed consent was waived because of the retrospective nature of the study and the anonymity of patients.
DONATION AND ALLOCATION PROCESS:
All lungs were from volunteer donation after death, and the next of kin provided written informed consent exercising their free will. No lungs were from executed prisoners. The Institutional Ethics Committee of the Organ Procurement Organization (OPO) approved the donation procedures. Donor lungs were allocated through the China Organ Transplant Response System (https://www.cot.org.cn/), following national policies, which were in compliance with internationally recognized principles. In allocation, the following priorities were comprehensively considered: regional geography, disease severity, blood type and histocompatibility match, children, immediate family of the donors, patients with rare opportunity, and waiting time [7]. After receiving notification of organ allocation, the transplant hospital logged on to the organ allocation system for the relevant medical information of the donor within 30 min and decided whether to accept or reject the donated human organ, based on medical judgment and the wishes of the waiting recipient, within 60 min [9].
STUDY POPULATION:
The 277 donor lungs offered to our center, Wuxi Lung Transplant Center, from June 1, 2018, to April 30, 2019, were assessed for inclusion in the analysis. Among the 140 donor lungs that were finally used, 101 (100 double lungs and 1 left lung) were sent to our center. A total of 112 recipients (50 double transplants, and 62 single transplants) were reviewed in our center.
STUDY DESIGN:
The donor lungs were assessed at 3 stages: before departure, after on-site management, and after harvesting. In stage 1, the preliminary information (including age, sex, weight, height, cause of death, ABO group, chest X-ray and computed tomography (CT) findings, PaO2/FiO2 ratio, serological status, and comorbidities), the availability of an appropriate recipient, and the feasibility of transportation before departure were evaluated. In stage 2, the suitability of the donor (such as PaO2/FiO2 ratio, chest X-ray and CT findings, and bronchoscopy findings) was assessed after on-site management. In stage 3, the transplantability of the donor lung (including donor lung inspection and palpation) after harvesting was finally confirmed.
To compare the difference in donor quality and utilization rate, the donors were categorized into group A and group B according to whether the donor hospital had the lung transplant qualification granted by the National Health Commission of China. By the end of 2018, a total of 32 medical institutions in China had obtained qualifications for lung transplantation [7]. The lung transplant doctors in these institutions are certified by the lung transplant training bases and have been trained in donor management, surgical techniques, and perioperative treatment.
DONOR-LUNG ASSESSMENT AND MANAGEMENT:
Considering the short history of lung transplantation and the varied quality of the hospitals in China, in 2018, our center took the lead in establishing the Chinese Lung Transplant Alliance (CLTA), aiming to share recipient information and offer help in donor assessment, management, and procurement. An intensive lung donor management protocol [10], including sputum suction by bronchoscope, recruitment maneuvers, ventilator parameter adjustment, restrictive fluid balance, and administration of antibiotics and hormones, is recognized and practiced in the CLTA.
In the whole procedure, all donor information was shared and discussed in the WeChat (a social networking application) group, which included surgeons, Intensive Care Unit (ICU) doctors, transplant doctors, and other members of the transplant team. After the donor lung was harvested in the operating room, a video showing the general condition of the lung was shared in the WeChat group, and the assessment results were presented promptly to the implant surgeon for final decision making.
DONOR SELECTION CRITERIA:
All donor lungs were selected based on donor lung selection criteria of the CLTA [10] (Table 2). It should be emphasized that donor lung assessment was a comprehensive procedure. Therefore, the oxygenation index served only as an important reference indicator rather than as a decisive indicator. Bronchoscopy findings such as aspiration or a large amount of viscous yellow sputum could have also excluded the lung from being selected.
LUNG PROCUREMENT, PRESERVATION, AND TRANSPORT:
The donor lung was procured using the standard technique of combined cardiopulmonary extraction [10], perfused with and preserved in low-potassium dextran solution. The procured donor lungs were transported by aircraft, high-speed train, automobile, or in-hospital transfer.
TRANSPLANTATION PROCEDURE:
An extracorporeal membrane oxygenation (ECMO) system (by femoral venous/arterial cannula) was used for life support in patients with severe hypoxemia or right-heart insufficiency requiring cardiopulmonary bypass, based on preoperative evaluation. In most recipients, either single- or double-lung transplantation was performed through an anterolateral thoracotomy without sternal division [11]. A clamshell incision was performed in 3 double-lung transplant recipients. Surgery was successfully completed in all recipients. Primary graft dysfunction (PGD), an early postoperative complication, was defined according to the International Society for Heart and Lung Transplantation [12].
STATISTICAL ANALYSIS:
SPSS version 22.0 was used for statistical analysis. The chi-squared test and Fisher’s exact test were used to compare categorical variables. For continuous variables, the
Results
DONOR POPULATION AND TRANSPORT:
From June 1, 2018, to April 30, 2019, a total of 277 donor lungs (donor age range, 6–59 years; mean age, 37.2±11.6 years) were recorded. The median tracheal intubation time was 5.5 days (IQR 4–8 days). The causes of death included trauma (146), intracranial bleeding (112), brain tumor (6), and other causes (13). A total of 140 donor lungs were finally used, with a utilization rate of 51%. Among them, 39 donor lungs were sent to other medical institutions of the CLTA, 100 donor lungs were sent to our institution, and 1 donor’s left lung and right lung were respectively sent to our center and another medical institution.
The green channel mechanism for organ transportation issued in 2016 in China ensured the smooth transfer of donated organs [5], reduced the transit and ischemia time, and therefore expanded the scope of acquisition. The 101 donor lungs sent to our center came from 16 cities across China (13 from Jiangsu Province, and 88 from other provinces, Figure 1), of which 85 cases (84%) were transported by airplane or airplane combined with high-speed train. The average transfer distance was 1008.3±267.4 km, the average transfer time was 5.1±0.9 h, and the transfer speed was 206.0±70.8 km/h (Table 3).
STAGED DONOR ANALYSIS:
A total of 137 donor lungs were excluded during the assessment of the 3 stages (Figures 2, 3). In stage 1, a total of 60 donor lungs were excluded for the following reasons: 24 for lack of recipients, 13 for insufficient management time, 10 for excessively poor quality, 8 for family refusal, 2 for presumed long ischemic time, and 3 for other reasons. Fifty donor lungs were abandoned in stage 2 for poor quality, 7 for family refusal, 2 for severe asthma,1 for hepatitis B virus infection, 1 for dust inhalation, and 1 for scheduling conflict. In stage 3, among the 155 donor lungs harvested and assessed, 15 were considered unsuitable for transplantation owing to quality problems that were not discovered in the preoperative examination and 1 was abandoned owing to surgical technique errors.
COMPARISONS BETWEEN QUALIFIED AND UNQUALIFIED MEDICAL INSTITUTIONS:
In stage 2, there were 123 cases in group A and 94 cases in group B (Table 4). Donors in group A were ventilated longer than those in group B. Chest X-ray/CT assessment demonstrated that group A donors had lower incidences of edema and pulmonary infiltrates/contusion than did group B donors. Group A also exhibited better PaO2/FiO2 and bronchoscopy results than did group B. The intervals between online notification and donation operation and between the first on-site assessment and donation operation in group A were both longer than those in group B (P<0.05).
The validity rates of donor lungs in group A were significantly higher than those in group B in all 3 stages, with an overall validity rate of 67.7% in group A and 34.7% in group B (
RECIPIENT OUTCOMES:
A total of 101 donor lungs were sent to our center, and 112 lung transplants (62 single and 50 double) were performed in 95 (85%) men and 17 (15%) women (age range, 23–75 years; mean age, 55.8±11.0 years). The indications for transplantation were idiopathic pulmonary fibrosis (48), emphysema (22), pneumonoconiosis (17), bronchiectasis (4), repeat transplant (3), pulmonary hypertension (2), pulmonary lymphangiomyomatosis (1), and other indications (15). Six (15.5%) patients were under mechanical ventilation or ECMO at the time of transplantation. During the procedure, 75 (67%) patients required ECMO. In total, the 30-day mortality rate was 18.8% (21 patients). The causes of death were pulmonary infection (13), PGD (4), cardiac failure (3), and airway bleeding (1). Grade 3 PGD was found in 17 (15.2%) recipients.
No significant difference was observed in the recipients’ general preoperative information between group A and group B (Table 5). The first graft ischemic time in group A was longer than that of group B, but the second graft ischemic time was the same in both groups. Grade 3 PGD developed in 13.9% (11/79) of recipients in group A and in 18.2% (6/33) of recipients in group B (P=0.567). The 30-day mortality rate was 17.7% (14/79) in group A and 21.2% (7/33) in group B (P=0.666).
Discussion
To the best of our knowledge, no previous analysis of the low utilization rate of donor lungs in China has been published. The abandonment of donor lungs is influenced by the specific economic, cultural, and medical factors in China.
Owing to the scarcity of donor lungs and the high requirements for surgical techniques and multidisciplinary teamwork, few medical institutions are qualified for lung transplantation and fewer lung transplant operations are performed annually in China than are liver and kidney transplants (Figure 4). Our center, the largest lung transplant center and the statistics center for lung transplantation in China, has had the leading role in lung transplantation in China since 2002 [13]. Therefore, the data used in this study could roughly reflect the status quo of donor lung utilization in China.
Unlike those countries with long waiting lists of lung transplant recipients [2,14,15], finding adequate lung transplantation candidates is a major problem in China. According to our study, owing to the lack of suitable recipients in the CLTA, 24 donor lungs, accounting for 40% of abandoned cases in stage 1 and 17.5% of all stages, had to be given up. The low awareness and the deviations in the indications of lung transplantation result in the scarcity of lung transplantation candidates. In our study, 42% of recipients were over 60 years of age, and their mean age (55.8±11.0 years) was higher than that reported by lung transplantation centers in other countries [2,16]. Many patients did not seek lung transplantation until they were critically ill, making it extremely dangerous for them to wait for the donor lungs and receive lung transplantation. This partly explains the higher perioperative mortality rate in our center than in the other lung transplantation centers. It is also worth noting that lung transplantation has not been covered by medical insurance in most parts of China, so the high cost has discouraged many patients.
In stages 1 and 2, family refusal led to 17 donor lungs being abandoned. In 8 cases, the family members withdrew their decision to donate, and in the other 9 cases, the family members were willing to donate only the liver and kidney but not the heart and lungs. Rejection of donation by family members can happen all over the world [17]. However, in China, organ donation is also influenced by Confucianism [18]. In Chinese traditional culture, the heart and lungs are the source of the conscience; thus, losing the heart and lungs is not acceptable for family members with traditional beliefs. Hence, it is necessary for the organ donation coordinator to confirm the family’s willingness to donate in order to save invalid travel and avoid the waste of time and human resources. Owing to family hesitancy, the complicated process of brain death diagnosis, and time spent on gathering an organ procurement team by the OPO, the median time of tracheal intubation in this study was 5.5 days (IQR 4–8 days), which was significantly longer than what was reported by centers in other countries (usually 1–3 days) [16,19,20]. Long-term intubation is more likely to cause infection and hypoxemia [21], posing difficulties in management.
Of the 137 abandoned cases in the 3 stages, 69 (50.4%) were due to the lack of or improper management of the donor lung in the early stage, which resulted in intractable hypoxemia, infection, and edema (Figure 3). Hence, ICU physicians need to conduct early interventions such as anti-infection, hormone therapy, airway management, and liquid control [20]. For ICU physicians, once a patient is identified as a potential donor, the treatment strategy must be promptly changed from saving the patient’s life to maintaining the function and the overall stability of the donor organs to maximize the transplantability of the organs [22].
However, the donation process and management protocol vary significantly between medical institutions with lung transplantation qualification and those without. In this study, compared to that in group B, the validity rate of stage 2 in group A was significantly higher, despite the longer intubation time. This could be attributed to the professional training and systematic mode in donor lung management in the medical institutions of group A.
The involvement of an experienced intensivist is associated with a greater number of transplantable organs [23]. By contrast, an intensivist with limited experience in donor lung management is related to a lower suitability rate. In our study, some medical institutions of group B with only 1 or 2 donor cases in a year lacked the experience in donor lung management and had insufficient basic equipment (such as bronchoscopes and hemofilters), which evidently led to the low utilization rate of donor lungs. According to our experience, common errors in donor lung management include (1) sputum specimens are not collected or collected late, resulting in the absence of sputum culture results when harvesting organs; (2) low-level antibiotics are used and timely adjustment based on sputum culture is lacking; (3) bronchoscopy is not performed routinely or bronchoscope is not prepared; (4) excessive fluid rehydration causes obvious pulmonary edema; (5) alveolar injury caused by excessive tidal volume [24]; and (6) the ventilator is disconnected during sputum suction, and lung recruitment is not applied in cases of atelectasis.
Among these errors, the liquid management of donors is extremely challenging and troublesome. Since kidney transplantation started earlier and is developing better than lung transplantation in China, some ICU physicians are more skillful in kidney management, and therefore tend to focus on retaining sufficient fluid in the kidneys while neglecting the maintenance of the lungs. Hence, in some cases, the donor is often refilled with a lot of fluid, the airway is moist, and a large amount of edema fluid can be sucked out by bronchoscopy, which are typical manifestations of pulmonary edema. In the present study, 14 cases in stage 2 and 4 cases in stage 3 were forced to be abandoned because of severe edema. Based on this, we hereby suggest a more restrictive, central venous pressure-guided (CVP <6 mmHg) fluid balance in multiorgan donors that supports adequate perfusion to vital organ systems [25]. This could prevent volume overload and lung neurogenic edema and increase the availability rate of lung grafts for transplantation, without impacting either kidney graft survival or development [26].
Because China has a vast territory with unevenly distributed medical and donor organ sources (Figure 1), organ procurement teams have to respond to demands swiftly and make a precise traveling and working schedule for organ procurement [13], which requires help from the OPO. Unlike the OPO in the United States and the Organization National De Transplantz in Spain, the OPO in China is not an independent legal entity from an administrative perspective [7], and most OPO staff members do not have the capacity to access and procure donor hearts and lungs independently. Hence, they need to contact the procurement teams from transplantation hospitals to negotiate the operation time and assess the organs, which can cause long-term intubation and uncertainty of organ procurement. Therefore, the OPO needs to ensure sufficient preoperative time for management and assessment, which to a certain extent determines the availability of donor lungs. In the present study, 14 cases (10.2%) were forced to be abandoned because of OPO-related issues, among which 13 were abandoned for insufficient management time. The interval between online notification and operation in group A (20.5 h [18.0–26.5 h]) was longer than that of group B (13.5 h [9.2–19.5]), indicating that the determination of donation time and notification of the procurement team were made earlier in group A than in group B. Therefore, in group A, more time was saved in the communication between the ICU physicians and the transplant physicians and for the assessment and management by procurement teams (the interval between first on-site assessment and donation operation).
As a retrospective analysis in a single center, this study has some weaknesses, which mainly resulted from incomplete data and the subjectivity in some evaluation items. The present study collected donor information of 277 cases over 11 months, which was less than the total number of donors in China during the same period. Many donor lungs were not reported in the online distribution system because of obviously poor quality or because the local medical institutions were not qualified for lung transplantation, which means that the actual donor lung utilization rate should be even lower (Figure 4).
Based on these results, we present some strategies that could be implemented in the current setting to elevate the utilization rate of donor lungs in China. First, some restrictions on lung transplant qualifications should be lifted so that lung transplantation training and lung transplantation programs can be conducted in more hospitals. Then, OPO staff and ICU physicians, especially those from community hospitals, should receive regular training courses on donor lung management. Second, cooperation and coordination should be established among the transplantation teams of different organs to increase the utilization rate of organs from the same donor. Third, ex vivo lung perfusion (EVLP) has been demonstrated to be valid in preserving and repairing marginal donor lungs. However, the high cost of EVLP precludes its wide application in China. At present, our center is using the modified EVLP method by adding the dialyzer to reduce the high cost caused by exchanging perfusion fluid hourly [27,28]. We hope this modified method could be successfully applied in other centers. Last, to expand the waiting list, increasing the public’s awareness and acceptance of lung transplantation is not enough. More efforts should be made to cover lung transplantation by medical insurance, which seems more practical [13].
Conclusions
Our study found that problems existing at both supply and demand ends contribute to the low utilization rate of donor lungs in China. On the supply side, long-term intubation coupled with the poor management of donors in some hospitals and OPO-related delays caused the low quality of donor lungs. On the demand side, low public awareness and high cost for transplantation are related to the short waiting list for lung transplantation and the waste of donor lungs. The above problems regarding organ donation and transplantation may exist in most developing countries. Improving the management of donor lungs and promoting publicity on lung transplantation in local communities are needed to increase the utilization rate of donor lungs.
Figures
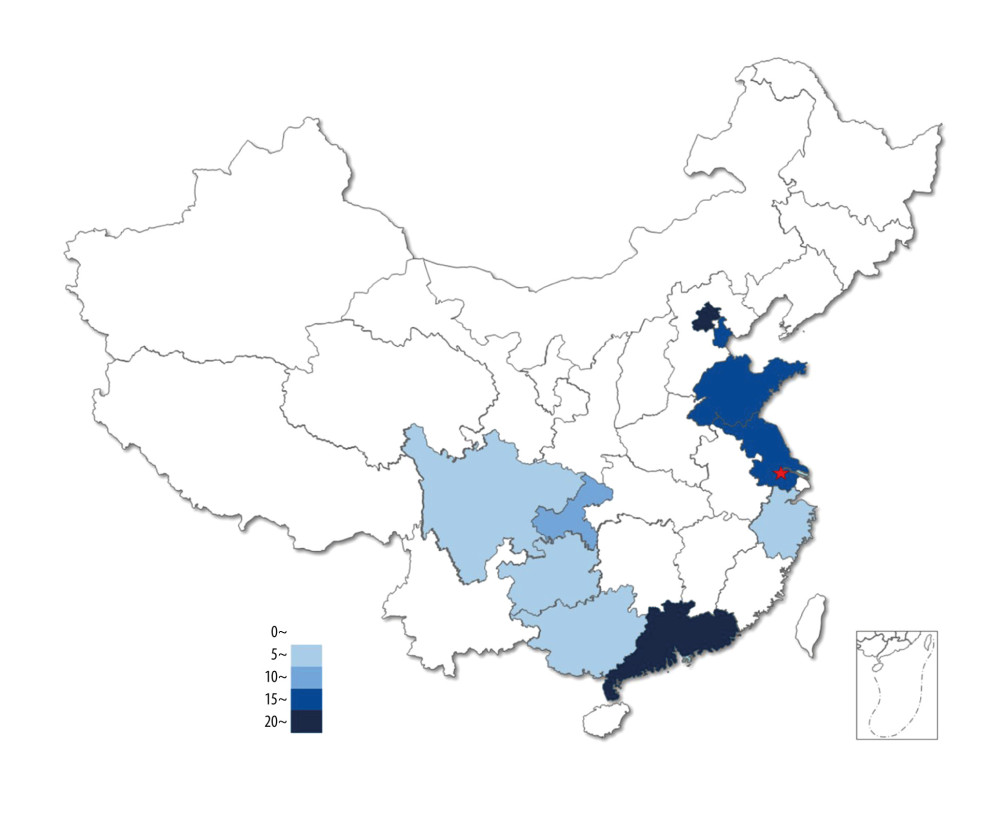 Figure 1. Source distribution of 101 donor lungs. The pentagram indicates the location of our center.
Figure 1. Source distribution of 101 donor lungs. The pentagram indicates the location of our center. 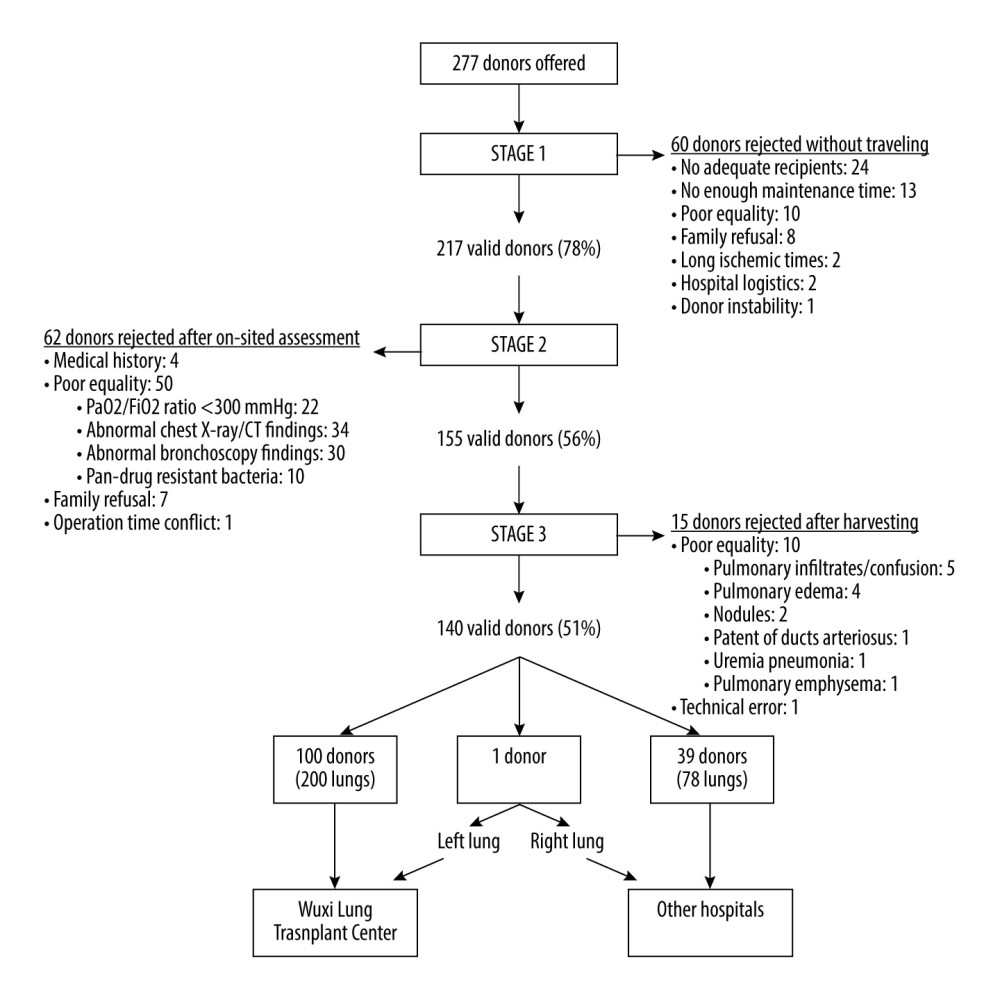 Figure 2. An overview of the study group: acceptability rates and causes of exclusion at each stage.
Figure 2. An overview of the study group: acceptability rates and causes of exclusion at each stage. 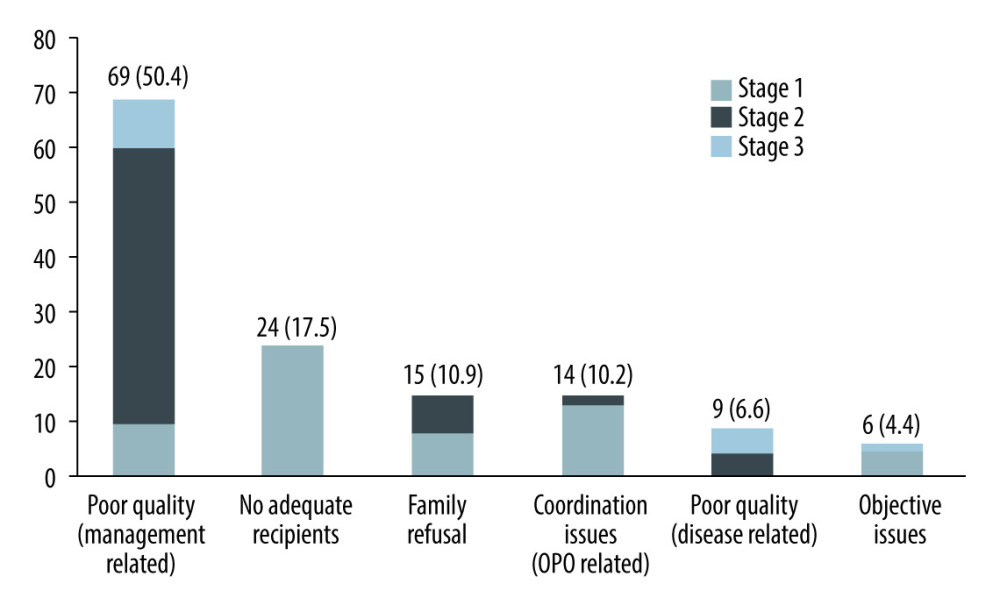 Figure 3. The number and proportion of donor lungs abandoned for different reasons.
Figure 3. The number and proportion of donor lungs abandoned for different reasons. 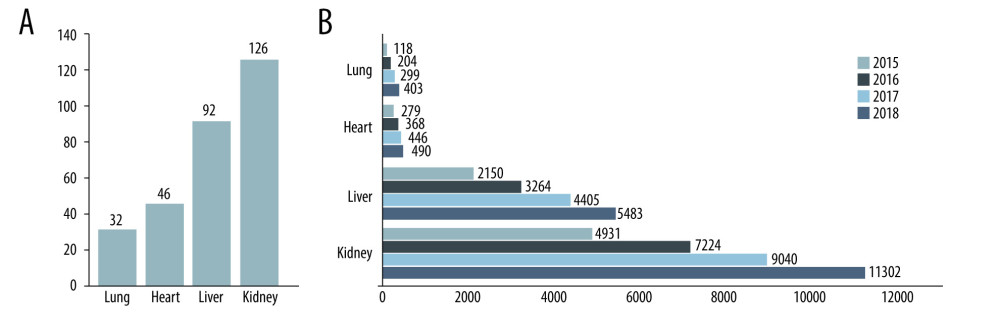 Figure 4. Medical institutions qualified for transplantation and transplant activity in China (except Hong Kong, Macao, and Taiwan). (A) Number of medical institutions qualified for transplantation in China by December 31, 2018. (B) Number of dead donor organ transplant operations in China from 2015 to 2018.
Figure 4. Medical institutions qualified for transplantation and transplant activity in China (except Hong Kong, Macao, and Taiwan). (A) Number of medical institutions qualified for transplantation in China by December 31, 2018. (B) Number of dead donor organ transplant operations in China from 2015 to 2018. Tables
Table 1. Number of donors, number of lung transplants, and donor conversion rate in different countries in 2018.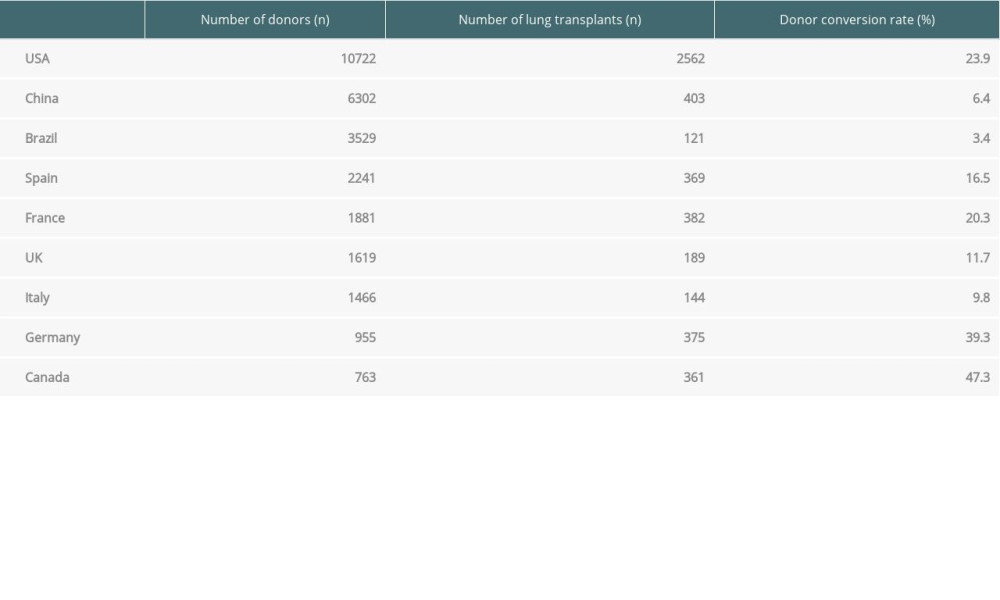 Table 2. Donor lung selection criteria of the Chinese Lung Transplant Alliance.
Table 2. Donor lung selection criteria of the Chinese Lung Transplant Alliance.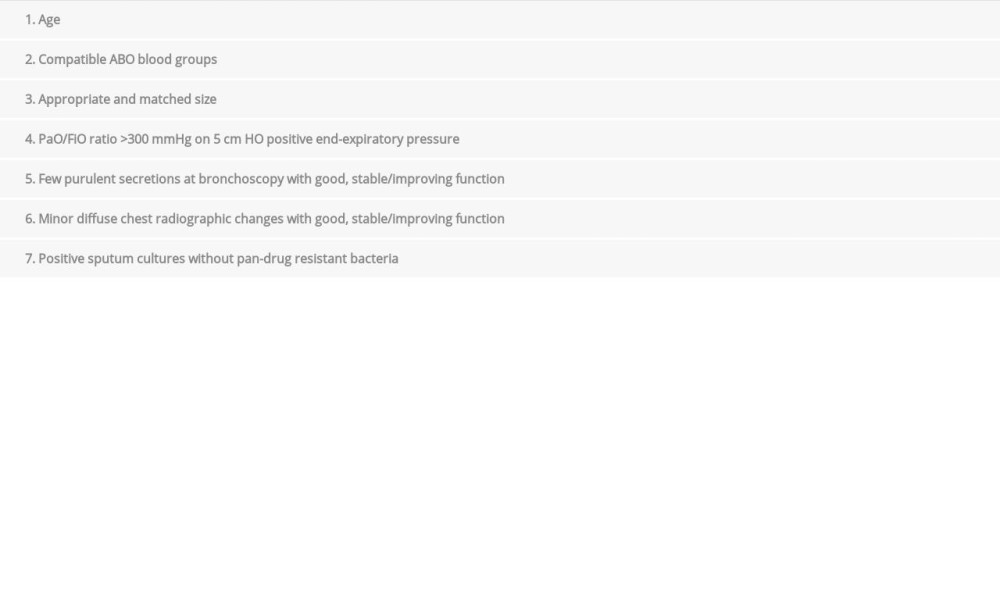 Table 3. Transport mode and time of the donor lungs (n=101).
Table 3. Transport mode and time of the donor lungs (n=101).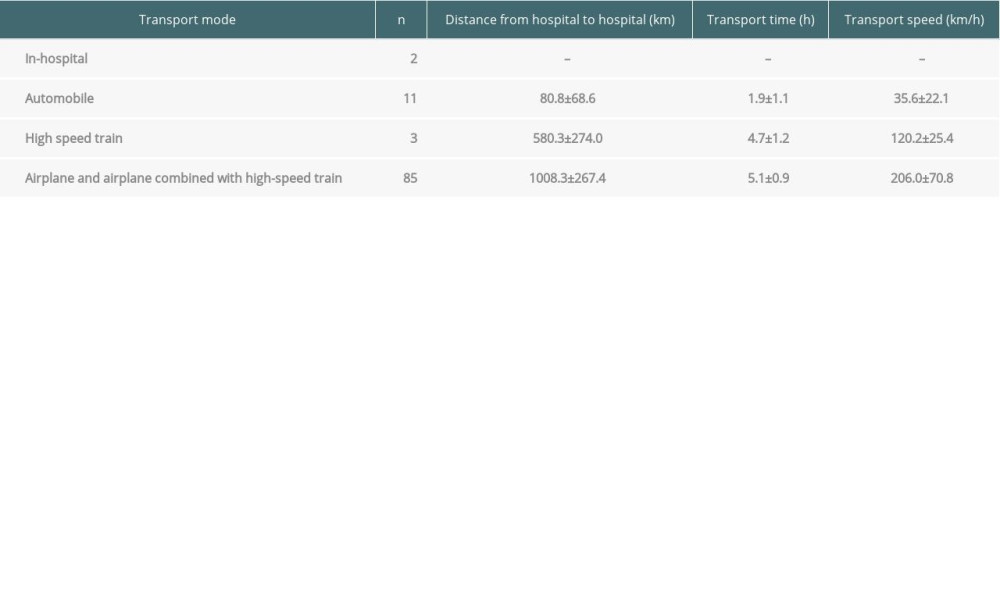 Table 4. Comparison of donor characteristics, assessment findings, and validity rates between the 2 groups in stage 2.
Table 4. Comparison of donor characteristics, assessment findings, and validity rates between the 2 groups in stage 2.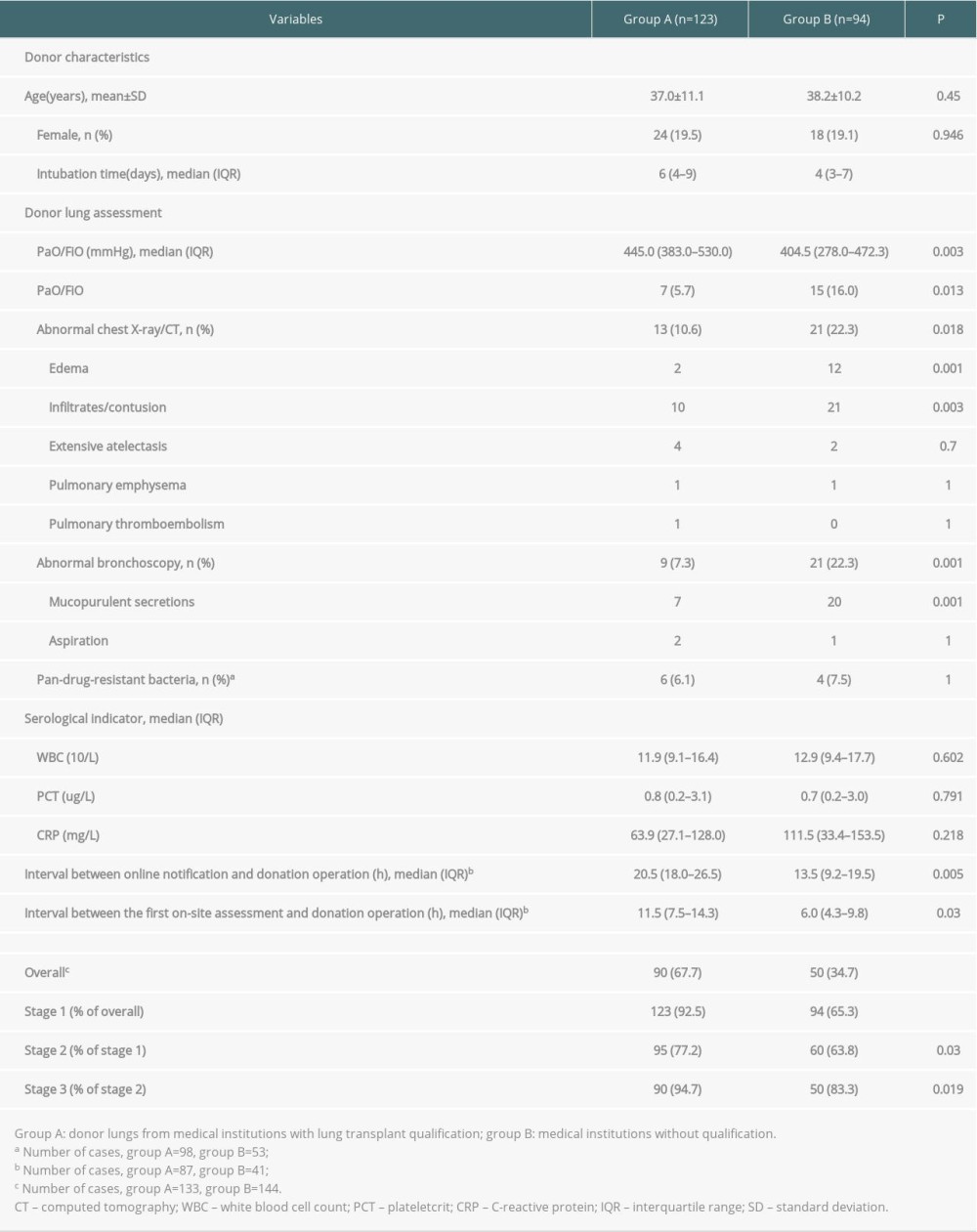 Table 5. Comparison of recipient characteristics, perioperative information, and 30-day mortality rate between the 2 groups.
Table 5. Comparison of recipient characteristics, perioperative information, and 30-day mortality rate between the 2 groups.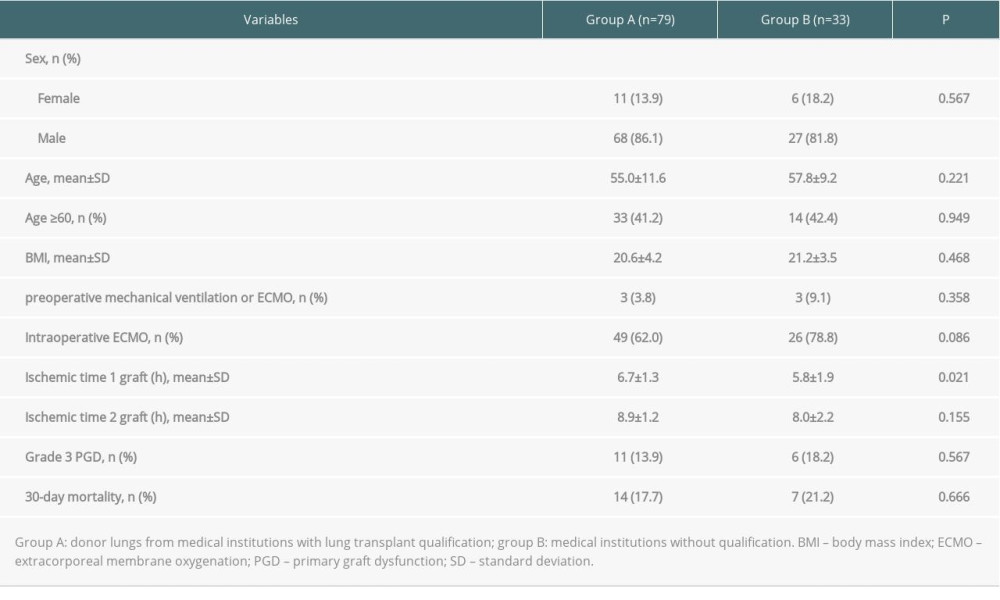
References
1. Chambers DC, Cherikh WS, Harhay MO, The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Thirty-sixth adult lung and heart-lung transplantation Report-2019; Focus theme: Donor and recipient size match: J Heart Lung Transplant, 2019; 38(10); 1042-55
2. Valapour M, Lehr CJ, Skeans MA, OPTN/SRTR 2018 Annual Data Report: Lung: Am J Transplant, 2020; 20(Suppl s1); 427-508
3. , Newsletter Transplant: International figures on donation and transplantation 2018, 2019 http://www.transplant-observatory.org/download/newsletter-transplant-2019/
4. Huang J, Millis JM, Mao Y, Voluntary organ donation system adapted to Chinese cultural values and social reality: Liver Transpl, 2015; 21(4); 419-22
5. Shi BY, Liu ZJ, Yu T, Development of the organ donation and transplantation system in China: Chin Med J (Engl), 2020; 133(7); 760-65
6. Hu CX, Chen WH, He JX, Lung transplantation in China between 2015 and 2018: Chin Med J (Engl), 2019; 132(23); 2783-89
7. Chinese Medical Association: Report On Organ Transplantation Developement in China (2015-2018), 2020 http://en.cma.org.cn/module/download/downfile.jsp?classid=0&filename=1641321f95524992974c11f71da149b9.pdf
8. Riddell P, Egan JJ, International donor conversion rates for lung transplantation need to be standardised: Lancet Respir Med, 2015; 3(12); 909-11
9. NationaI HeaIth Commission of the People’s RepubIic of China: Provisions on the Administration of the Procurement and Allocation of Human Donated Organs, 2019 http://www.gov.cn/gongbao/content/2019/content_5397751.htm
10. Branch of Organ Transplantation of Chinese Medical Association, Guideline on the standard of lung transplantation donors and the acquisition and transshipment in China: Organ Transplant, 2018; 9(5); 325-33 [in Chinese]
11. Meyers BF, Sundaresan RS, Guthrie T, Bilateral sequential lung transplantation without sternal division eliminates posttransplantation sternal complications: J Thorac Cardiovasc Surg, 1999; 117(2); 358-64
12. Christie JD, Carby M, Bag RReport of the ISHLT Working Group on Primary Lung Graft Dysfunction part II: Definition, A consensus statement of the International Society for Heart and Lung Transplantation: J Heart Lung Transplant, 2005; 24(10); 1454-59
13. Wu B, Hu C, Chen W, China lung transplantation developing: Past, present and future: Ann Transl Med, 2020; 8(3); 41
14. Komatsu T, Oshima A, Chen-Yoshikawa TF, Physical activity level significantly affects the survival of patients with end-stage lung disease on a waiting list for lung transplantation: Surg Today, 2017; 47(12); 1526-32
15. Oshima A, Nishimura A, Chen-Yoshikawa TF, Nutrition-related factors associated with waiting list mortality in patients with interstitial lung disease: A retrospective cohort study: Clin Transplant, 2019; 33(6); e13566
16. Alvarez A, Moreno P, Espinosa D, Assessment of lungs for transplantation: A stepwise analysis of 476 donors: Eur J Cardiothorac Surg, 2010; 37(2); 432-39
17. Shaw D, Elger B, Persuading bereaved families to permit organ donation: Intensive Care Med, 2014; 40(1); 96-98
18. Iltis AS, Building norms for organ donation in China: Pitfalls and challenges: J Med Philos, 2019; 44(5); 640-62
19. Cano JR, Algar FJ, Cerezo F, Results of lung transplantation in patients with chronic obstructive pulmonary disease: Transplant Proc, 2008; 40(9); 3073-75
20. Minambres E, Perez-Villares JM, Chico-Fernandez M, Lung donor treatment protocol in brain dead-donors: A multicenter study: J Heart Lung Transplant, 2015; 34(6); 773-80
21. Courtwright A, Cantu E, Evaluation and management of the potential lung donor: Clin Chest Med, 2017; 38(4); 751-59
22. Minambres E, Coll E, Duerto J, Effect of an intensive lung donor-management protocol on lung transplantation outcomes: J Heart Lung Transplant, 2014; 33(2); 178-84
23. Singbartl K, Murugan R, Kaynar AM, Intensivist-led management of brain-dead donors is associated with an increase in organ recovery for transplantation: Am J Transplant, 2011; 11(7); 1517-21
24. Determann RM, Royakkers A, Wolthuis EK, Ventilation with lower tidal volumes as compared with conventional tidal volumes for patients without acute lung injury: A preventive randomized controlled trial: Crit Care, 2010; 14(1); R1
25. Minambres E, Rodrigo E, Ballesteros MA, Impact of restrictive fluid balance focused to increase lung procurement on renal function after kidney transplantation: Nephrol Dial Transplant, 2010; 25(7); 2352-56
26. Ballesteros MA, Duerto Alvarez J, Martin-Penagos L, Influence of specific thoracic donor therapy on kidney donation and long-term kidney graft survival: J Nephrol, 2017; 30(6); 869-75
27. Wei D, Gao F, Yang Z, Ex vivo lung perfusion with perfusate purification for human donor lungs following prolonged cold storage: Ann Transl Med, 2020; 8(3); 38
28. Liu F, Lu Y, Wei D, Effect of ex vivo lung perfusion on storage of isolated lungs: Ann Palliat Med, 2020; 9(2); 359-67
Figures
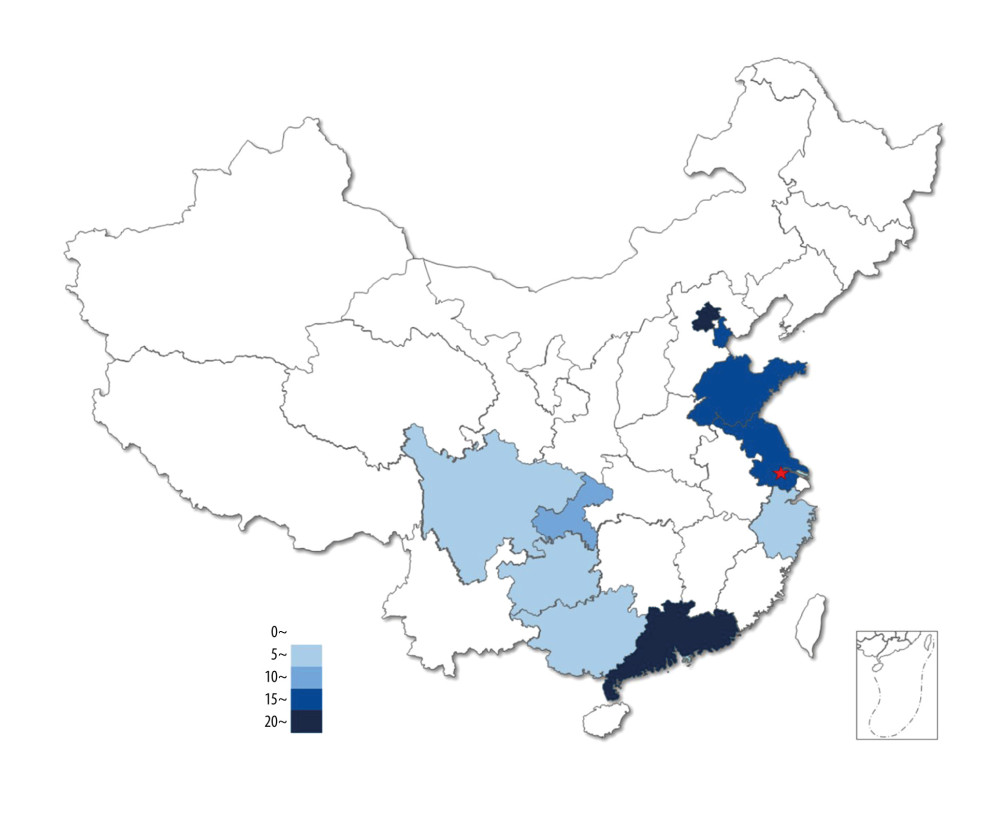 Figure 1. Source distribution of 101 donor lungs. The pentagram indicates the location of our center.
Figure 1. Source distribution of 101 donor lungs. The pentagram indicates the location of our center.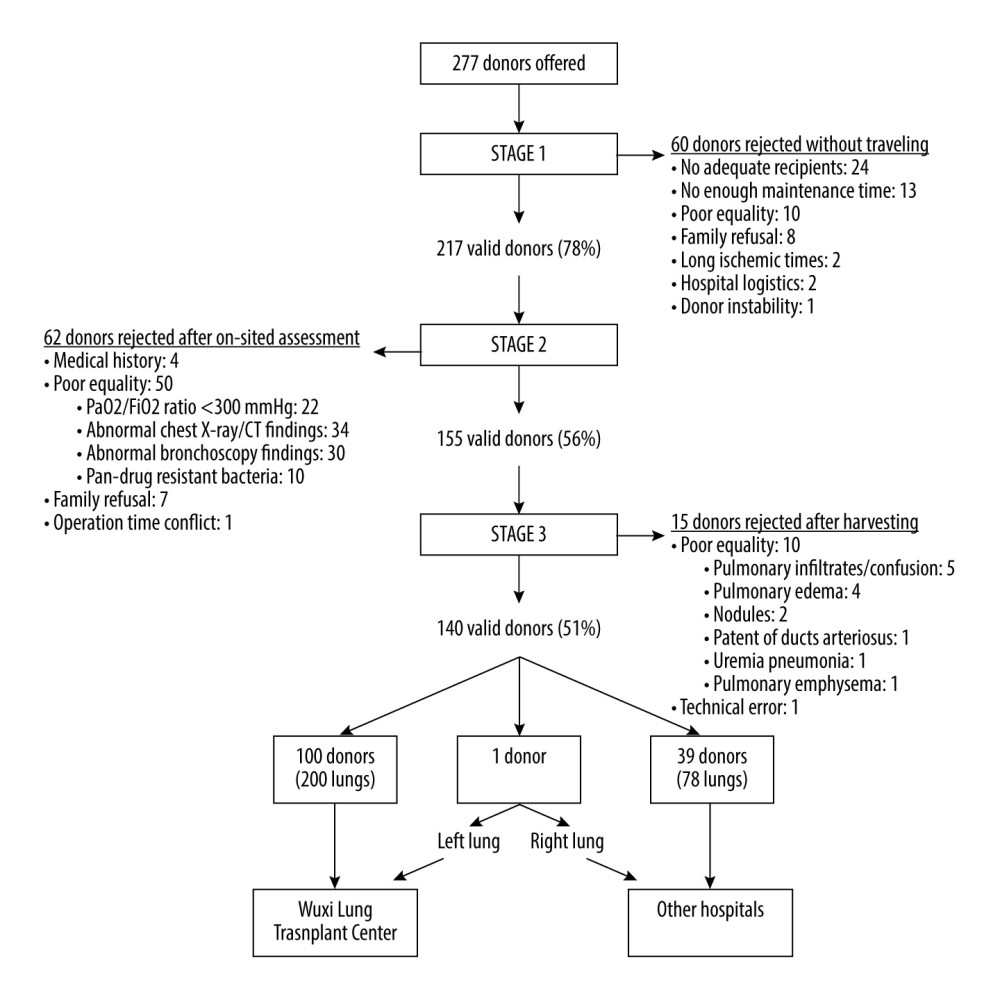 Figure 2. An overview of the study group: acceptability rates and causes of exclusion at each stage.
Figure 2. An overview of the study group: acceptability rates and causes of exclusion at each stage.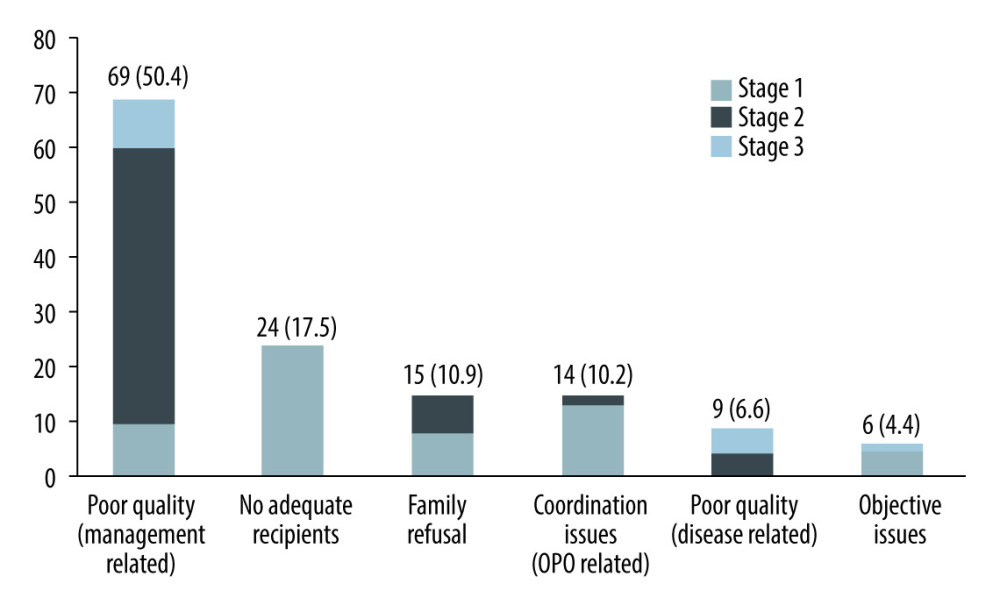 Figure 3. The number and proportion of donor lungs abandoned for different reasons.
Figure 3. The number and proportion of donor lungs abandoned for different reasons.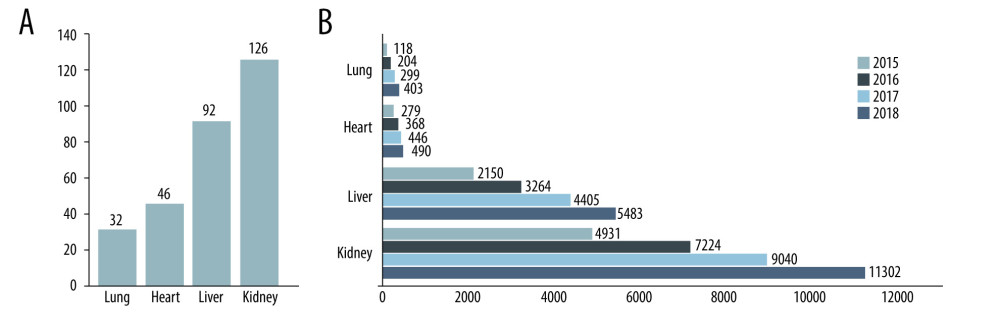 Figure 4. Medical institutions qualified for transplantation and transplant activity in China (except Hong Kong, Macao, and Taiwan). (A) Number of medical institutions qualified for transplantation in China by December 31, 2018. (B) Number of dead donor organ transplant operations in China from 2015 to 2018.
Figure 4. Medical institutions qualified for transplantation and transplant activity in China (except Hong Kong, Macao, and Taiwan). (A) Number of medical institutions qualified for transplantation in China by December 31, 2018. (B) Number of dead donor organ transplant operations in China from 2015 to 2018. Tables
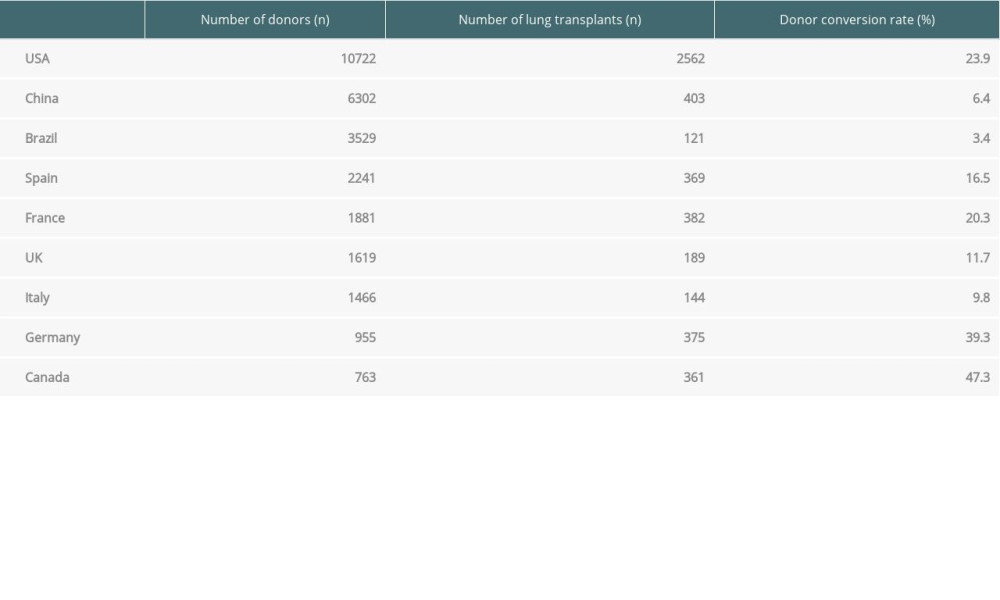 Table 1. Number of donors, number of lung transplants, and donor conversion rate in different countries in 2018.
Table 1. Number of donors, number of lung transplants, and donor conversion rate in different countries in 2018.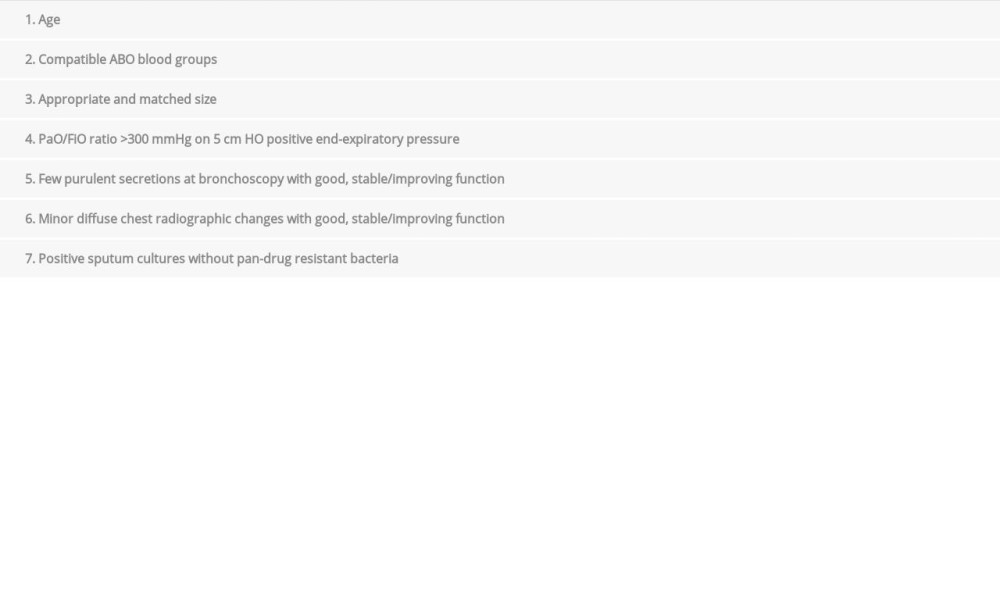 Table 2. Donor lung selection criteria of the Chinese Lung Transplant Alliance.
Table 2. Donor lung selection criteria of the Chinese Lung Transplant Alliance.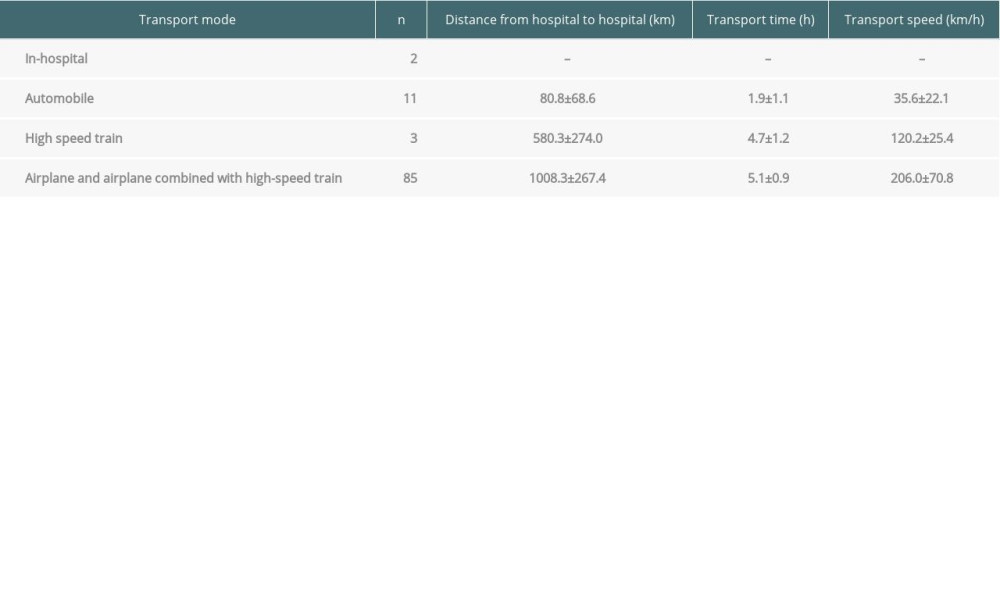 Table 3. Transport mode and time of the donor lungs (n=101).
Table 3. Transport mode and time of the donor lungs (n=101).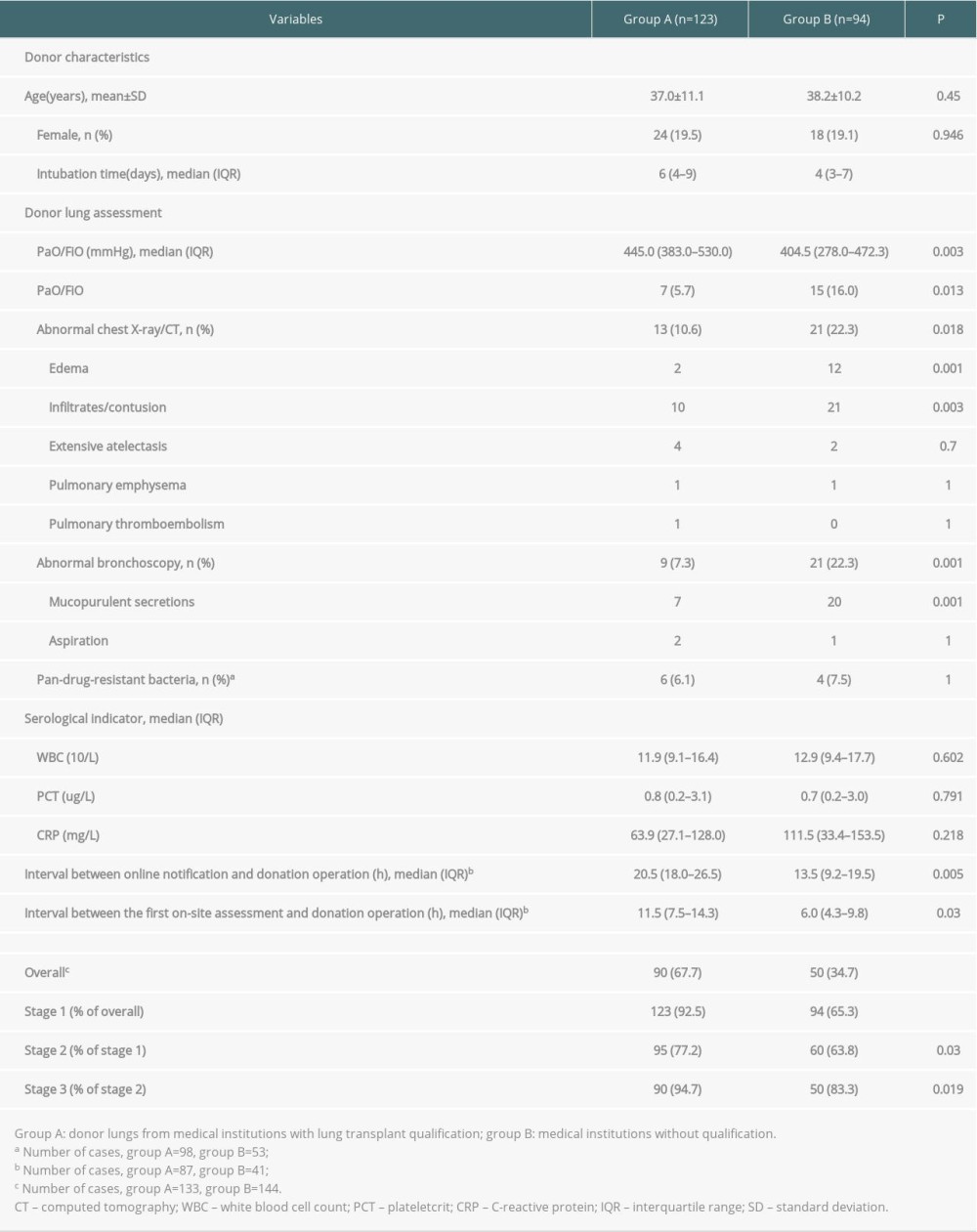 Table 4. Comparison of donor characteristics, assessment findings, and validity rates between the 2 groups in stage 2.
Table 4. Comparison of donor characteristics, assessment findings, and validity rates between the 2 groups in stage 2.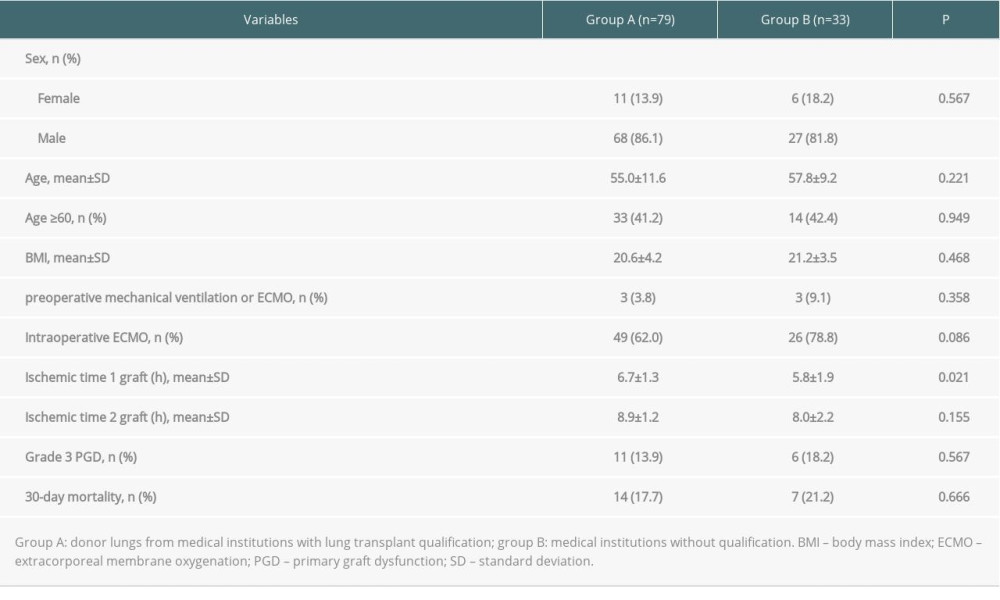 Table 5. Comparison of recipient characteristics, perioperative information, and 30-day mortality rate between the 2 groups.
Table 5. Comparison of recipient characteristics, perioperative information, and 30-day mortality rate between the 2 groups.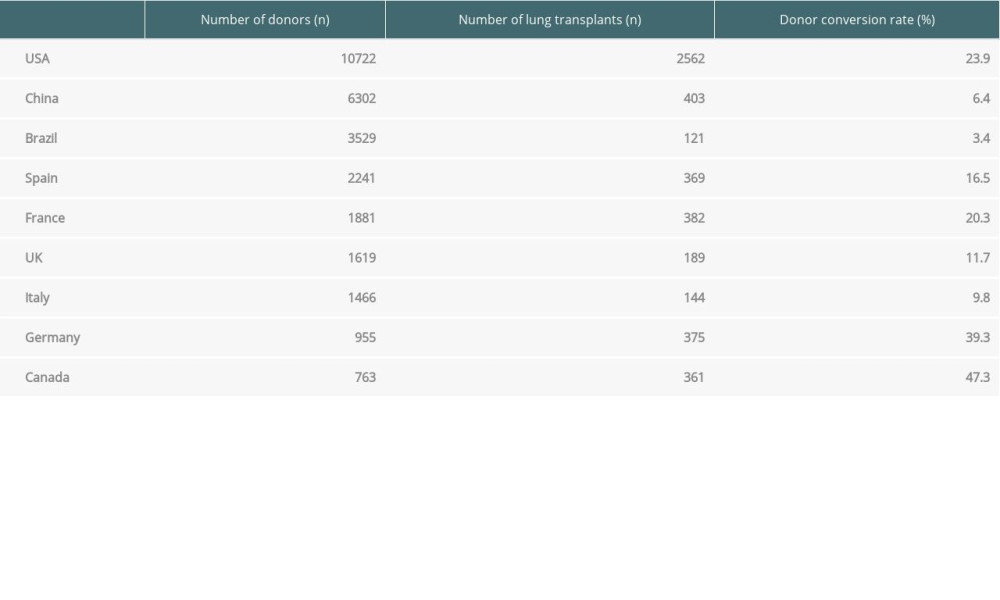 Table 1. Number of donors, number of lung transplants, and donor conversion rate in different countries in 2018.
Table 1. Number of donors, number of lung transplants, and donor conversion rate in different countries in 2018.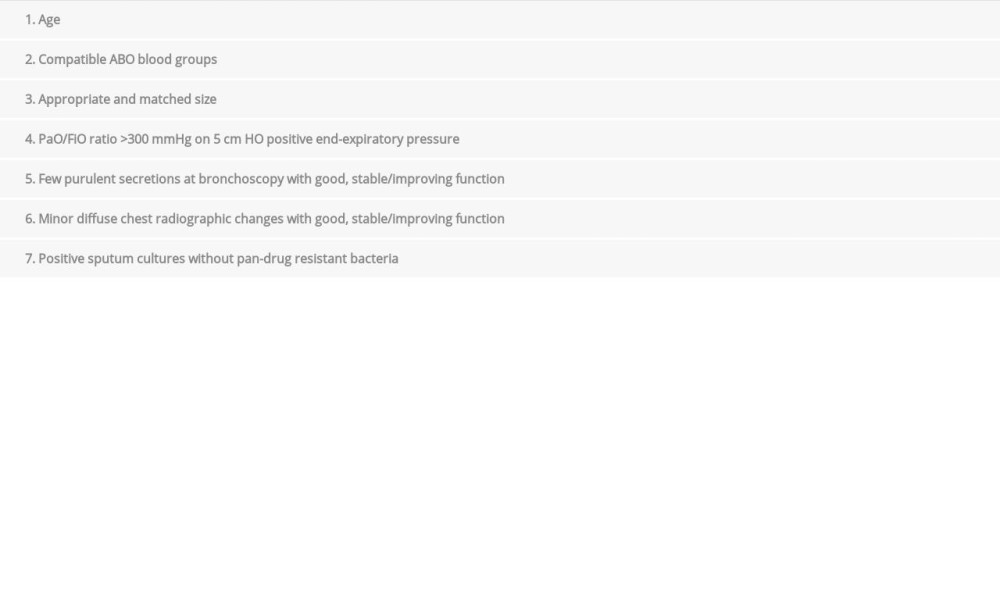 Table 2. Donor lung selection criteria of the Chinese Lung Transplant Alliance.
Table 2. Donor lung selection criteria of the Chinese Lung Transplant Alliance.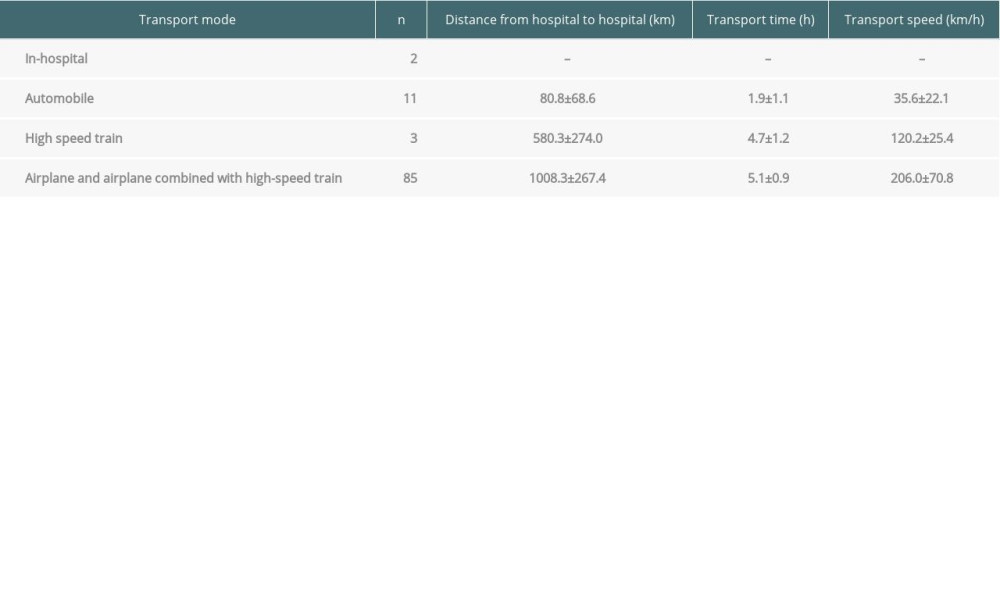 Table 3. Transport mode and time of the donor lungs (n=101).
Table 3. Transport mode and time of the donor lungs (n=101).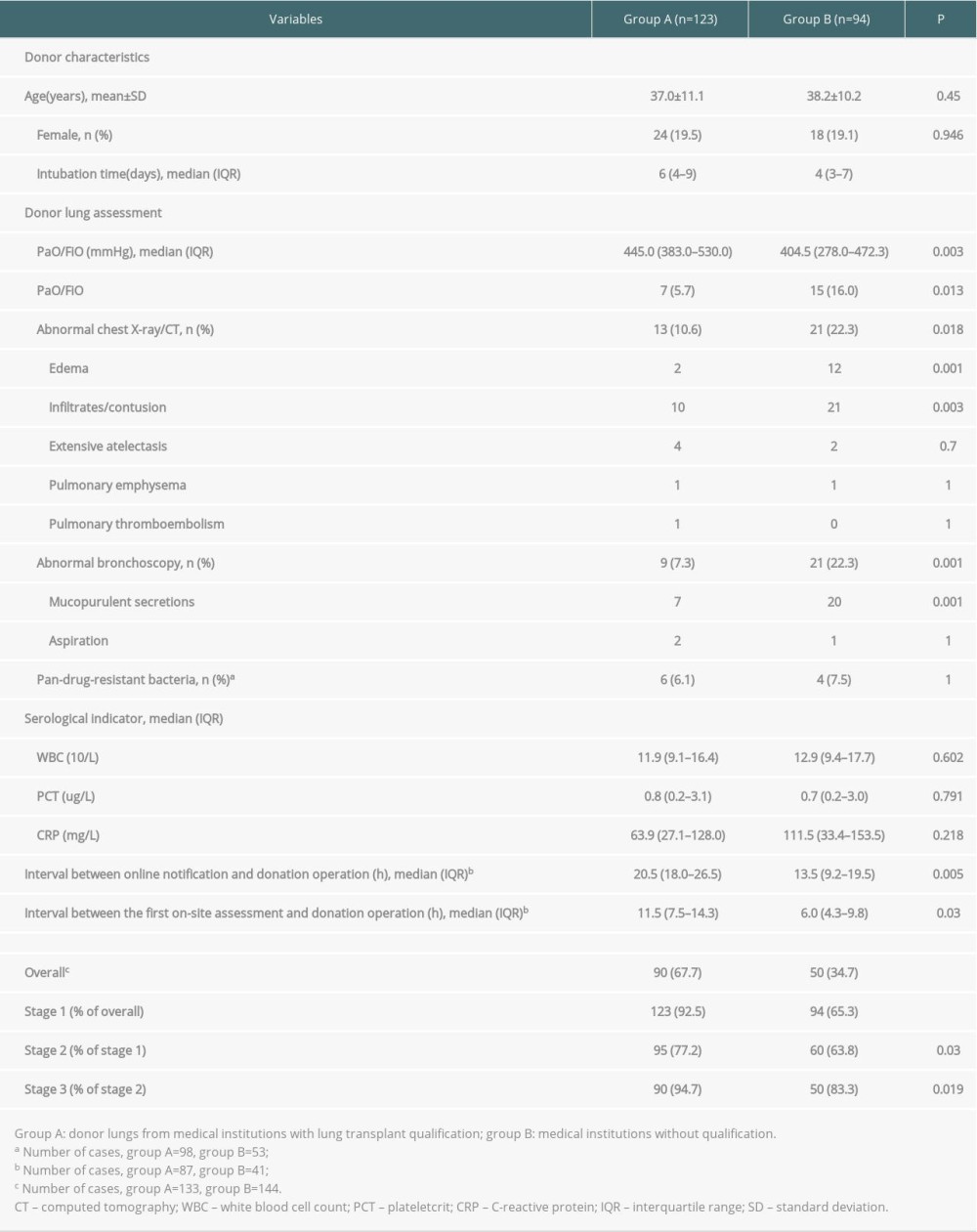 Table 4. Comparison of donor characteristics, assessment findings, and validity rates between the 2 groups in stage 2.
Table 4. Comparison of donor characteristics, assessment findings, and validity rates between the 2 groups in stage 2.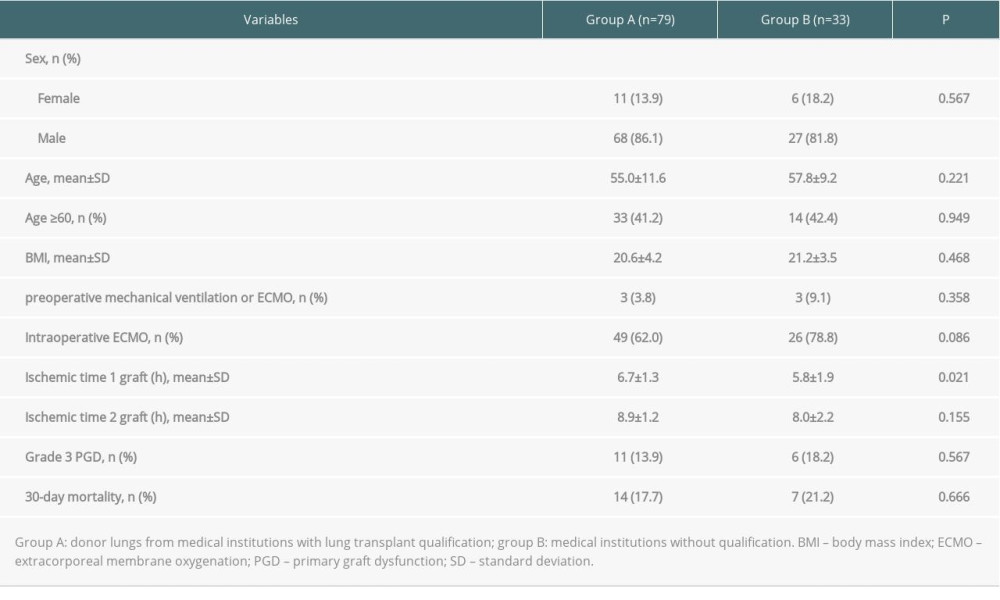 Table 5. Comparison of recipient characteristics, perioperative information, and 30-day mortality rate between the 2 groups.
Table 5. Comparison of recipient characteristics, perioperative information, and 30-day mortality rate between the 2 groups. In Press
18 Mar 2024 : Original article
Does Antibiotic Use Increase the Risk of Post-Transplantation Diabetes Mellitus? A Retrospective Study of R...Ann Transplant In Press; DOI: 10.12659/AOT.943282
20 Mar 2024 : Original article
Transplant Nephrectomy: A Comparative Study of Timing and Techniques in a Single InstitutionAnn Transplant In Press; DOI: 10.12659/AOT.942252
28 Mar 2024 : Original article
Association Between FEV₁ Decline Rate and Mortality in Long-Term Follow-Up of a 21-Patient Pilot Clinical T...Ann Transplant In Press; DOI: 10.12659/AOT.942823
02 Apr 2024 : Original article
Liver Transplantation from Brain-Dead Donors with Hepatitis B or C in South Korea: A 2014-2020 Korean Organ...Ann Transplant In Press; DOI: 10.12659/AOT.943588
Most Viewed Current Articles
05 Apr 2022 : Original article
Impact of Statins on Hepatocellular Carcinoma Recurrence After Living-Donor Liver TransplantationDOI :10.12659/AOT.935604
Ann Transplant 2022; 27:e935604
12 Jan 2022 : Original article
Risk Factors for Developing BK Virus-Associated Nephropathy: A Single-Center Retrospective Cohort Study of ...DOI :10.12659/AOT.934738
Ann Transplant 2022; 27:e934738
22 Nov 2022 : Original article
Long-Term Effects of Everolimus-Facilitated Tacrolimus Reduction in Living-Donor Liver Transplant Recipient...DOI :10.12659/AOT.937988
Ann Transplant 2022; 27:e937988
15 Mar 2022 : Case report
Combined Liver, Pancreas-Duodenum, and Kidney Transplantation for Patients with Hepatitis B Cirrhosis, Urem...DOI :10.12659/AOT.935860
Ann Transplant 2022; 27:e935860








