02 May 2023: Original Paper
The Incidence of Brain-Dead Donors Based on Screening and Management Led by Intensivists
Hyo Jin LeeDOI: 10.12659/AOT.939521
Ann Transplant 2023; 28:e939521
Abstract
BACKGROUND: This study aimed to compare the incidence of brain-dead (BD) donors and potential brain-dead (PBD) donors before vs after the introduction of intensivists.
MATERIAL AND METHODS: This longitudinal retrospective study was performed between January 2012 and December 2020 at Seoul Metropolitan Government-Seoul National University Boramae Medical Center. Four dedicated intensivists were introduced in January 2016. The periods before and after introduction of the intensivists were defined as the pre-introduction period (2012-2015) and post-introduction period (2016-2020), respectively.
RESULTS: During the study period, there were 2872 discharges in the Intensive Care Unit, of which there were a total of 113 PBD (3.93%) and 36 BD (1.25%) donors. The number of PBD and BD donors increased in the post-introduction period compared in the pre-introduction period (PBD, 47.84 vs 27.14 per 1000 discharges; BD, 13.59 vs 11.03 per 1000 discharges). Poisson regression analysis showed the annual incidence rate of PBD donors significantly increased post-introduction (PBD, 27.53% vs 48.11%, P=0.044), while those of BD donors were similar between the 2 groups (BD, 11.41% vs 13.9%; P=0.743). The annual incidence rate of the total number of organ donations, multi-organ donations (>3 organs), and donation of organs (heart, lung, and kidney) increased in the post-introduction period compared to that in the pre-introduction period.
CONCLUSIONS: Our findings suggest a beneficial role of a dedicated intensivist, not only in improving actual organ donation and discovering PBD donors, but also in affecting the yield of the heart and lung transplantation in actual organ donation compared to donors without a dedicated intensivist.
Keywords: Transplantation, Brain Death, Intensive Care, Organ Transplantation, Humans, Incidence, Retrospective Studies, Tissue Donors, Tissue and Organ Procurement, Brain
Background
Organ transplantation is the ultimate treatment option for patients with end-stage organ failure [1]. The number of people awaiting transplantation has increased steadily over the years. According to the Korea Network for Organ Sharing (KONOS), although 22 695 people awaited transplant surgery in 2016, only 4685 transplants were performed, of which approximately 573 were from deceased donors [2,3]. However, in Korea, the number of brain-dead (BD) donors has steadily decreased from 573 in 2016 to 478 in 2020 [2,3]. Considering the significant disparity between organ donation and demand, this decline is a serious problem. Therefore, diverse attempts have been made to reverse the downward trend by introducing in-house transplant coordinator programs [4], achieving goal-directed donor management protocols [5], and acquiring organs from marginal donors by extending donation criteria [6].
The initial step of organ donation usually occurs in the Intensive Care Unit (ICU) [7]. Intensivists may play an important role in the donation process, including identification of potential organ donors, communication between medical staff, and providing options for organ donations to family members [8]. Additionally, dedicated intensivists usually have sufficient experience in the management of hemodynamically unstable patients such as BD donors to perform the required management for organ donation [9]. There is increasing evidence that controlling these pathophysiological changes through active management in the Intensive Care Unit maintains organ function, improving the number and functional quality of transplantable organs [9,10]. Despite these important roles, there is a lack of research on the impact of dedicated intensivists on potential brain-dead (PBD) donors.
We suggest that dedicated intensivists provide a beneficial role in the donation process, including identification of PBD donors and increasing actual organ donation. In this study, we aimed to compare the incidence of PBD and BD donors before and after the introduction of a dedicated intensivists.
Material and Methods
STUDY DESIGN AND PARTICIPANTS:
This longitudinal retrospective study assessed all PBD and BD donors and collected data on the total number of patients discharged from the Medical ICU (MICU) and Surgical ICU (SICU) between January 2012 and December 2020 from the Seoul Metropolitan Government-Seoul National University (SMG-SNU) Boramae Medical Center (BMC). The period before and after the introduction of the dedicated intensivist were defined as the pre-introduction period (2012–2015) and post-introduction period (2016–2020), respectively.
Before introduction of dedicated intensivists in SMG-SNU BMC, management of critically ill patients and PBD donors or screening of PBD donors was performed only by attending physicians of admitting departments without any specialists from the critical care department or an organ transplant department. Therefore, screening for PBD donors could be overlooked and organ preservation management of BD donors was performed ineffectively. After a dedicated intensivist acquired a new position in the critical care department in January 2016, SMG-SNU BMC started BD donor management with the organ transplant department. A total of 4 dedicated intensivists, 2 each in the MICU and SICU, have been at the forefront of treating critically ill patients and PBD donors. PBD donors were screened by a dedicated intensivist who was an originally an attending physician, trainee physicians in the ICU, and specialist nurses in the organ transplant department. After brain death was confirmed, the donor was referred and assigned to another dedicated intensivist in charge of the primary care with an organ transplant coordinator until organ transplantation was performed. To improve organ donation for PBD donors, organ transplant coordinators provided organ donation pamphlets, educational materials, and professional counseling on brain death donation to families of PBD donors. In addition, these pamphlets and educational materials are always kept in the ICU and are provided to the attending physician and intensivists.
Definitions of the terms utilized are as follows: 1) BD donors are patients with irreversible loss of all functions of the brain or brainstem, who undergone formal brain death determination including apnea testing or ancillary study, and who have actually undergone transplant surgery as donors. 2) PBD donors are patients who meet the criteria of Glasgow Coma Scale score ≥4 due to irreversible brain injury, absence of brainstem reflex, or the possibility of progression to brain death [3]. PBD donors consist of both BD donors and patients whose donations were withdrawn for multiple reasons, although presumed to have brain death while in the ICU (eg, donation refusal, withdrawal of donation, ineligible for donation, suspended contact with medical staff, death during process).
VARIABLES:
Details pertaining to demographic information, including age, body mass index (BMI), history of smoking, marriage, religion, level of education, blood type, presence of organ donation wish registration, documented physician orders for life-sustaining treatment, and severity illness scores, were obtained. Severity of illness was evaluated according to the Acute Physiology and Chronic Health Evaluation II (APACHE II), Simplified Acute Physiology Score II, and Sequential Organ Failure Assessment score. Data on the main causes of brain death, including cerebrovascular ischemia, intracranial tumor, cerebral hemorrhage, hypoxic brain injury caused by hanging, drug intoxication, or cardiac arrest, were collected. During admission to the ICU, we recorded the department of attending dedicated intensivists and admitted patients, admission route, use of inotropes, vasopressors, desmopressin, steroids (including methylprednisolone, prednisolone, hydrocortisone, or dexamethasone), application of continuous renal replacement therapy (CRRT), and amount of fluid administered intravenously before or on the day of donation in BD donors or death in PBD donors. We also assessed 6 organ types (heart, lung, liver, kidney, small intestine, pancreas, and cornea), the total number of donated organs, and the characteristics of brain death judgement date in BD donors.
OUTCOMES:
Our primary outcome was to compare the annual incidence rate (patients/1000 discharges/year) of PBD donors and BD donors before and after introduction of a dedicated intensivist. The secondary outcome was to compare the annual incidence rate ratio (incidence rate of patients in current year/incidence rate of patients in the previous year) of PBD and BD donors, and the annual incidence rate of actual donation organs (number of donated organ/10 donor/year) between pre- and post-introduction of a dedicated intensivist. In addition, the annual incidence rate of donated organs according to organ types was analyzed before and after the introduction of a dedicated intensivist.
DATA AND STATISTICAL ANALYSIS:
The data on total number of PBD donors and BD donors between January 2012 and December 2020 was obtained from KONOS. Data are presented as means with standard deviations or medians with standard errors for continuous variables and numbers with percentages for categorical variables. The
ETHICS:
This study was conducted in accordance with the principles of the Declaration of Helsinki. The Institutional Review Board of SMG-SNU Boramae Medical Center approved this study and waived the requirement for informed consent (IRB No.20-2021-40).
Results
BASELINE CHARACTERISTICS:
The baseline characteristics of the included patients are presented in Table 1. A total of 79 patients were included before (n=20) and after (n=59) the introduction of a dedicated intensivist. The mean age was 52 years and the proportion of men was 67%. There was a comparable distribution in BMI, smoking history, comorbidities, and blood types between pre -and post-introduction groups. Personal information, including marital status, religion, and level of education, was significantly different between the groups. In terms of marital status, the proportion of married people (47%) was higher after introduction of a dedicated intensivist, while the number of people who were unmarried (35%) was higher before introduction of a dedicated intensivist. With respect to religion, atheists (38%) were the most common, followed by Christians (21.5%).
CLINICAL FEATURES:
Table 2 shows the clinical features of the patients in the pre -and post-introduction groups. As seen from the table, 63% of the BD donors were PBD donors after the introduction of dedicated intensivists. The most common reason for rejection of donation among PBD donors was refusal by their legally authorized representative (63.6%), followed by death (13.6%) (Supplementary Table 1). Due to lack of data before 2014, the analysis was undertaken only for the period from 2014 to 2020. Almost all patients were admitted to the ICU through the emergency department, rather than the general ward or coronary care unit. More than twice the number of patients admitted to the MICU were admitted to the SICU, and neurosurgery was the most common department. Cerebral hemorrhage (61.5%) was the most common cause of brain death, followed by cardiac arrest-related hypoxic brain injuries (26.6%). The causes of brain death were well-distributed between the 2 groups. There were no significant differences in the severity of illness, average volume of fluid administrated on the day before (1st day) or on next day (2nd day) of operated organ donation, use of vasopressors, steroids, and desmopressin, and application of CRRT between the 2 groups.
MAIN OUTCOMES:
The main findings are listed in Table 3. A total of 113 patients were included before (n=32) and after (n=81) the introduction of a dedicated intensivist. During the 9 years of the study period (2012–2020), there were 2872 discharges in the ICU; there were 36 BD (1.25%) and 113 PBD donors (3.93%). The number of BD donors increased from 13 (11.03/1,000 discharges) during the pre-introduction period (2012–2015) to 23 (13.59/1000 discharges) during the post-introduction period (2016–2020). Additionally, the number of PBD donors increased from 32 (27.14/1000 discharges) in the pre-introduction period to 81 (47.84/1000 discharges) in the post-introduction period. The cumulative incidence of BD donors and PBD donors from 2012 to 2020 is shown in Figure 2.
The Poisson regression results are presented in Table 4. The annual incidence rate of PBD donors was significantly higher post-introduction compared to pre-introduction of a dedicated intensivist, while those of BD donors were similar between the 2 groups (27.53 vs 48.11, P=0.044; 11.41 vs 13.9, P=0.743; Figure 3). There was also a significant increase in the annual incidence rate ratio of BD donors in the post-introduction period but a decrease in those of BD donors in the pre-introduction period (1.532, [95% CI=1.112–2.111] vs 0.546, [95% CI=0.311–0.959]). In terms of PBD donors, while no significant change in annual incidence rate ratio was observed pre-introduction, there was a significantly higher annual incidence rate ratio post-introduction (0.964 [95% CI=0.702–1.324] vs 1.179 [95% CI=1.007–1.380]).
The subgroup analysis of the annual incidence rate according to donated organ type is presented in Table 5 and Supplementary Table 2. The annual incidence rate of total number and over 3 organs from 1 BD donor increased in the post-introduction period compared in the pre-introduction period (21.54 vs 23.91; 3.08 vs 6.52). Moreover, the annual incidence rates of donated hearts, lungs, and kidneys were higher in the post-introduction period compared to the pre-introduction period (2.31 vs 3.48; 1.54 vs 4.78; 7.69 vs 8.26, respectively).
Discussion
This retrospective study compared the annual incidence rate and the annual incidence rate ratio of BD and PBD donors before and after the introduction of a dedicated intensivist. It was noted that there was an increase in the annual incidence rate of PBD donors after the introduction of the intensivist. In addition, both BD and PBD donors significantly increased yearly after the introduction of the intensivist, while there was a yearly decrease in BD or stagnation in PBD donors before the introduction of the intensivist. Moreover, the incidence rate of more than 3 organ donations from 1 BD donor numerically increased after introduction of an intensivist. More donations of hearts and lungs were also observed in the presence of a dedicated intensivist compared to the absence. There was better kidney function at the date of donation and annual incidence rate of kidney donation (incidence per 10 donors/year) after introduction of the dedicated intensivist compared to before; however, the severity of illness was comparable between the pre- and post-intensivist periods.
In Korea, the total number of BD donors significantly increased between 2012 to 2015 and then decreased from 2016 to 2020 [2]. Additionally, the total number of donated organs or more than 3 donated organs from 1 BD donor had decreased from 2016 to 2020 [2]. However, in our study, there was a notable increase in the incidence of BD donors and in the total number of donated organs or more than 3 organs donated from 1 BD donor after the introduction of a dedicated intensivist (2016–2020) compared to before (2012–2015). In general, the number of organ transplantations performed in a medical center can vary due to several factors, such as the number of potential donors, the availability of specialized medical staff, the current prevalence of end-stage organ failure in the population, and advancements in medical technology [11]. Furthermore, when we investigated other possible factors affecting the incidence of PBD or BD donors, there was no remarkable change in factors such as the number of trainees and residents of ICU, the number of beds in the MICU or SICU, reporting system after discovery of PBD or BD donors by the organ transplant team established since 2009, or their day/night work hours during the study periods except for the introduction of intensivists. Additionally, in our study, the number of heart and lung organ donations increased, particularly in 2020 compared to 2019, while the Korean Organ Donation Agency’s 2020 annual report indicated a decrease in the heart and lung organ donations in Korea during the same period [12]. Despite investigating various factors during the study period, we found no remarkable changes, as discussed above. However, it is worth noting that the coronavirus disease (COVID-19) pandemic may have had an impact on lung transplantation in Korea and globally, as the virus can cause severe respiratory complications that could potentially increase the need for lung transplantation [13]. In conclusion, although the demand for lung transplantation may have increased due to COVID-19 infection, the overall number of the heart and lung organ donations decreased in Korea, and it can be inferred that the effect of donor management by dedicated intensivists contributed to the increase in the heart and lung organ donation. Therefore, our study suggests that a dedicated intensivist may contribute not only to the identification of both PBD and BD donors, but also improvement in the yield of total organs, including the heart and lung, in BD donors.
Several efforts have been made to improve identification of PBD donors and the acceleration of actual organ donation in the ICU. In a single-center study, dedicated intensivists in critical care management contributed to many organ donors [14]. Moreover, several single-center studies have documented that a dedicated intensivist could improve the quality of organ condition and increase the number of obtained organs, including the heart and lung, from a BD donor [14,15]. It is widely perceived that achieving donor management goals by institutionalized dedicated intensivists results in increased organ transplants per donor in the critical care unit [16]. Our findings also suggest the beneficial role of a dedicated intensivist, and is thus concordant with previous studies.
In the present study, the annual incidence rate of BD donors was relatively low compared to that of PBD donors after dedicated intensivist introduction. The following reasons are speculated to have contributed: There were no PBD donors who registered a wish for organ donation in advance, and over 63% of PBD donors’ family decided to refuse organ donation in our study. This could imply that the patient’s family might feel burdened in making decisions without the patient’s prior declaration of intention. The role of the dedicated intensivist is to improve organ donations and to contribution to the development of empathy with the patient’s family members who make the decision on organ donation. Most BD donors are in the Intensive Care Unit [7]; therefore, the attending physician feels the responsibility of explaining the possibility of organ donation first, even if there is an organ procurement team acting as a professional counselor [17]. In our hospital, dedicated intensivists participate and act as intermediaries between these trainees and the professional organ procurement team. In a single-center study, well-trained and educated physicians contributed to the increased acceptance of organ donation by patients’ families [18]. It is speculated that the explanation and participation of the organ donation procedure by a dedicated intensivist, who is more empathetic than the third expert, will contribute to an increase in the organ donation rate.
This study had several limitations. First, it was a retrospective single-center study and had relatively small numbers of PBD or BD donors before and after introduction of an intensivist. Second, the analysis involved a relatively short follow-up period with a dedicated intensivist compared with that without a dedicated intensivist. Therefore, to generalize the potential benefits of a dedicated intensivist, more studies with larger numbers of patients are needed. Third, we did not quantitatively or qualitatively assess the role of the intensivist, including brain death identification, declaration and certification, and organ donation-detailed counseling along with patient’s family or transplant coordinator. Additionally, as our study lacks post-transplant outcomes and survival data, it is necessary to analyze the impact of introducing a dedicated intensivist on the survival rate and post-transplant outcomes of organ recipients through future data collection. Fourth, it is still questionable whether a dedicated intensivist has a better role in increasing the number of the heart and lung organs, including the heart or lung, than before the introduction of the intensivist. In Korea, the number of the heart and lung organ donations has steadily increased to 156 for hearts, 89 for lungs in 2016, 173 for hearts, and 150 for lungs in 2020 [2]. Instead, our study suggests an increased total number of donated organs or more than 3 organs donated from 1 BD donor, although these decreased in Korea during 2016–2020 [2]. Moreover, it is also worth noting that the COVID-19 pandemic may have had an impact on lung transplantation in Korea and globally, as the virus can cause severe respiratory complications that could potentially increase the need for lung transplantation [13]. This is thought to be a contributing factor to the increase in lung transplant donors, especially in 2020, in addition to the effect of a dedicated intensivist [13]. Therefore, we cautiously suggest that a dedicated intensivist improved the yield of donated organs from 1 BD donor.
Conclusions
Our findings suggest introduction of dedicated intensivists may affect not only in PBD donors, but also can improve actual organ donation and affect the yield of heart and lung transplantation in actual organ donation. It is speculated that participation in the organ donation procedure by the dedicated intensivist may contribute to an increase in the incidence of organ donation.
Figures
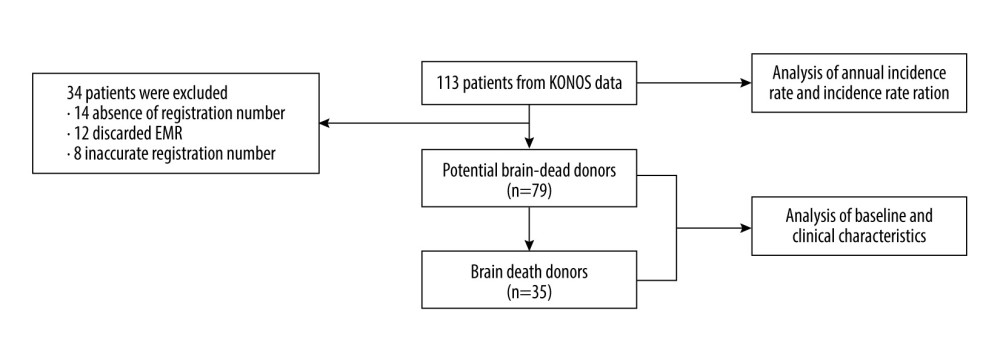 Figure 1. Flow chart depicting the study designEMR – electronic medical record; KONOS – Korea Network for Organ Sharing.
Figure 1. Flow chart depicting the study designEMR – electronic medical record; KONOS – Korea Network for Organ Sharing. 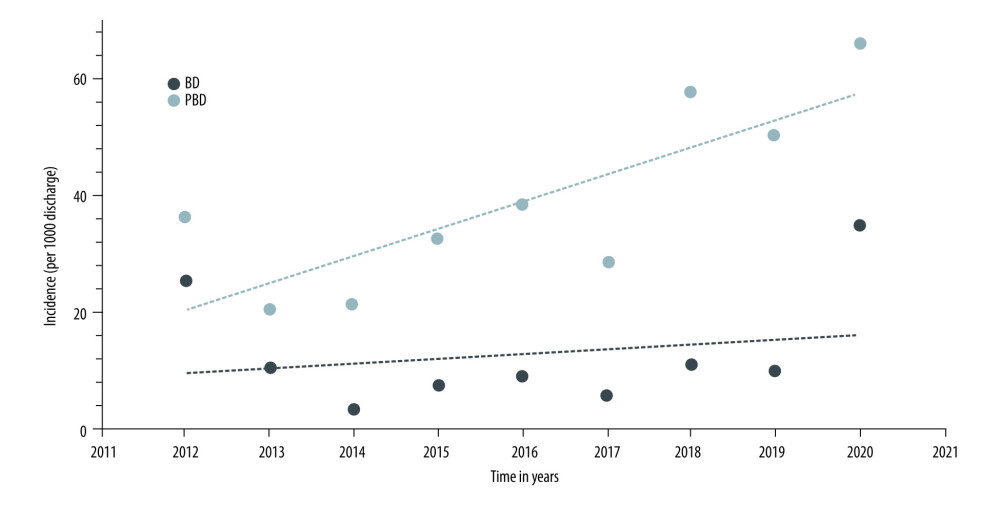 Figure 2. Cumulative incidence of brain-dead (BD) donor and potential brain-dead (PBD) donorIncidence presented as patients per 1000 discharges/year. BD – brain-dead; PBD – potential brain-dead.
Figure 2. Cumulative incidence of brain-dead (BD) donor and potential brain-dead (PBD) donorIncidence presented as patients per 1000 discharges/year. BD – brain-dead; PBD – potential brain-dead. 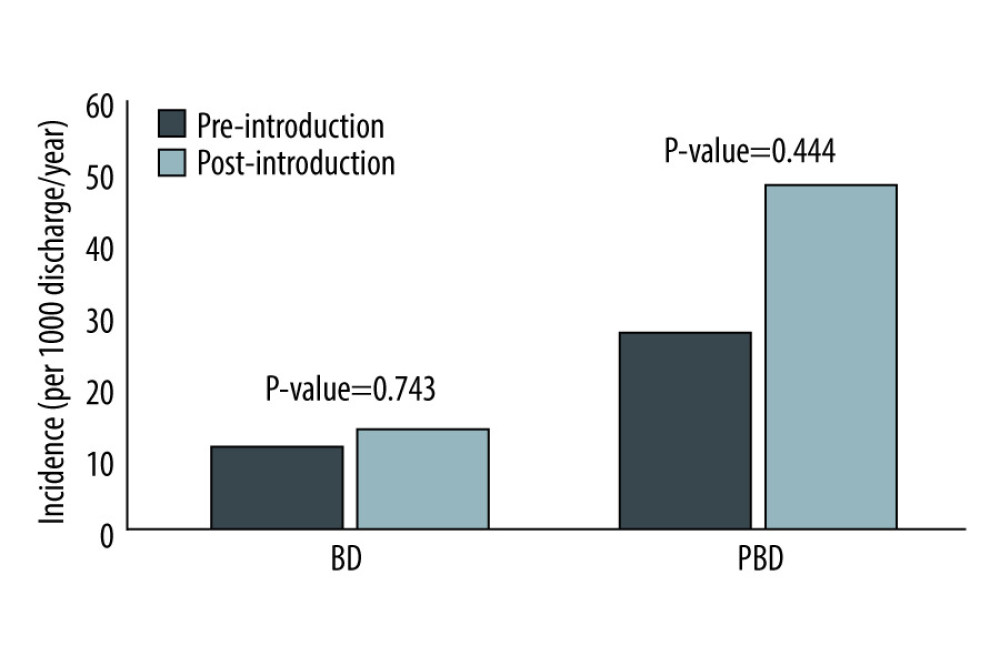 Figure 3. Comparison of incidence rate before and after introduction of dedicated intensivistIncidence presented as patients per 1000 discharges/year. BD – brain-dead; PBD – potential brain-dead
Figure 3. Comparison of incidence rate before and after introduction of dedicated intensivistIncidence presented as patients per 1000 discharges/year. BD – brain-dead; PBD – potential brain-dead Tables
Table 1. Baseline characteristics of pre-introduction and post-introduction groups.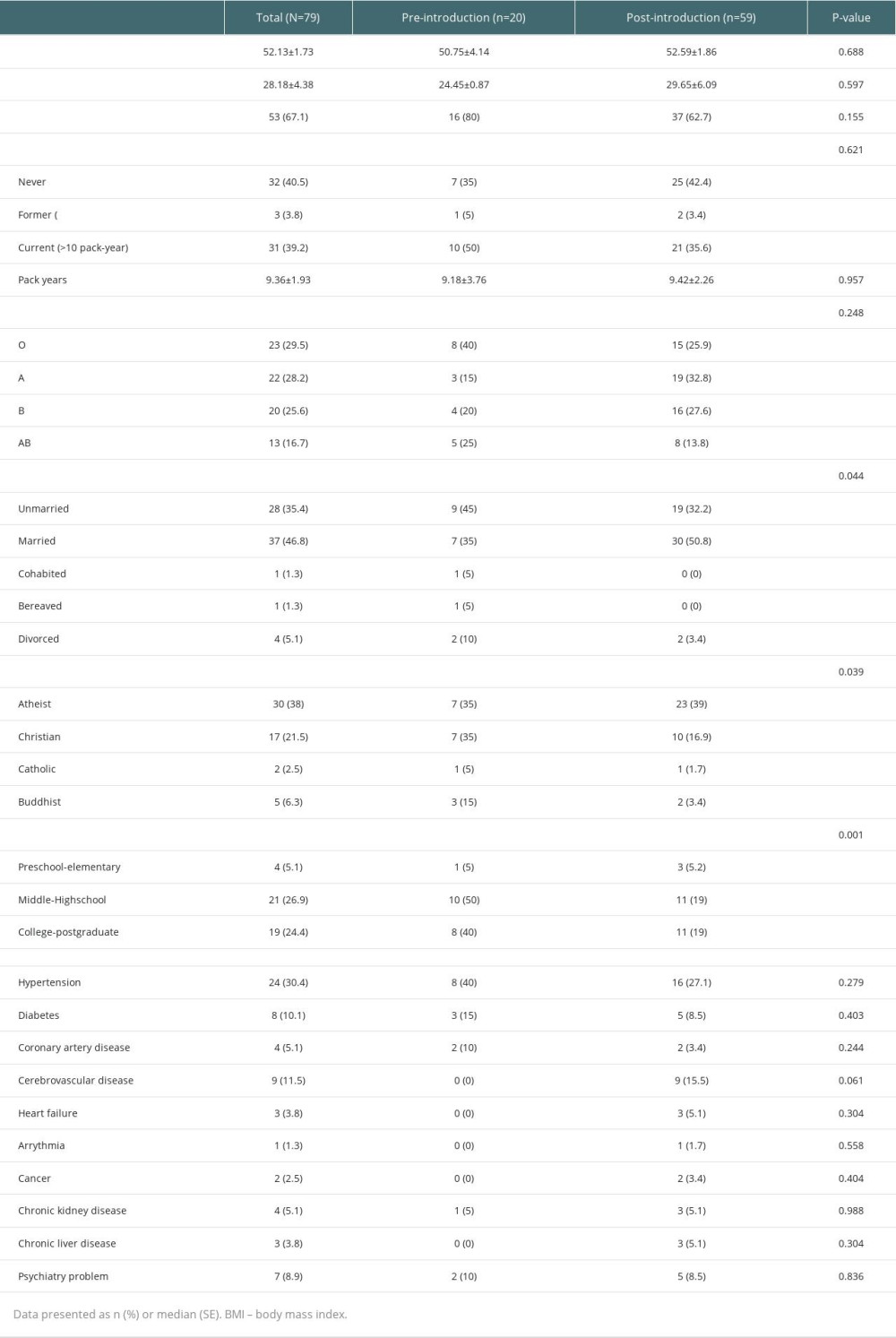 Table 2. Clinical features of pre-introduction and post-introduction groups.
Table 2. Clinical features of pre-introduction and post-introduction groups.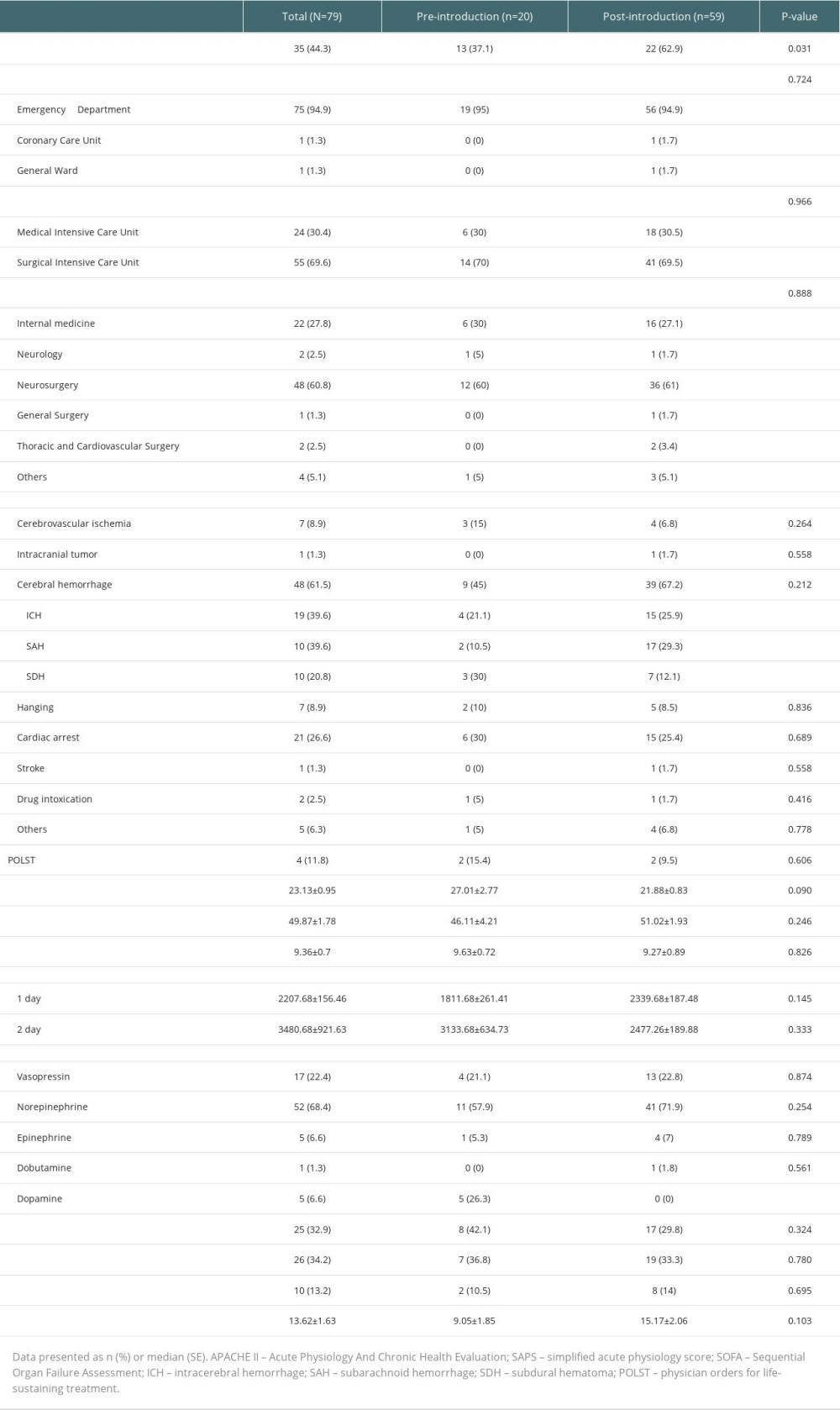 Table 3. Number of brain-dead (BD) donors and potential brain-dead (PBD) donors during the study period.
Table 3. Number of brain-dead (BD) donors and potential brain-dead (PBD) donors during the study period.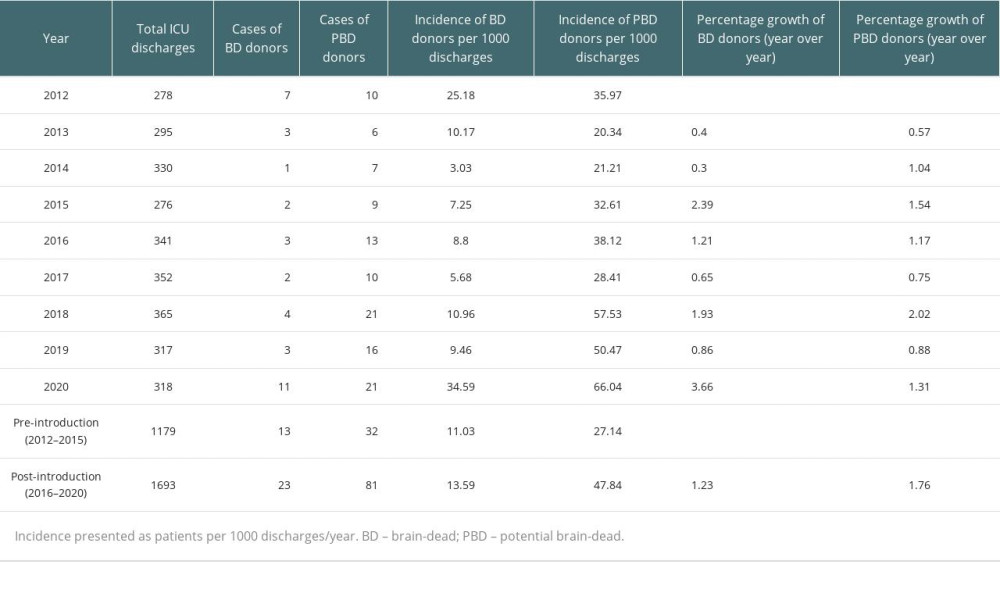 Table 4. Comparison of incidence rate and incidence rate ratio before and after introduction of the intensivist system.
Table 4. Comparison of incidence rate and incidence rate ratio before and after introduction of the intensivist system.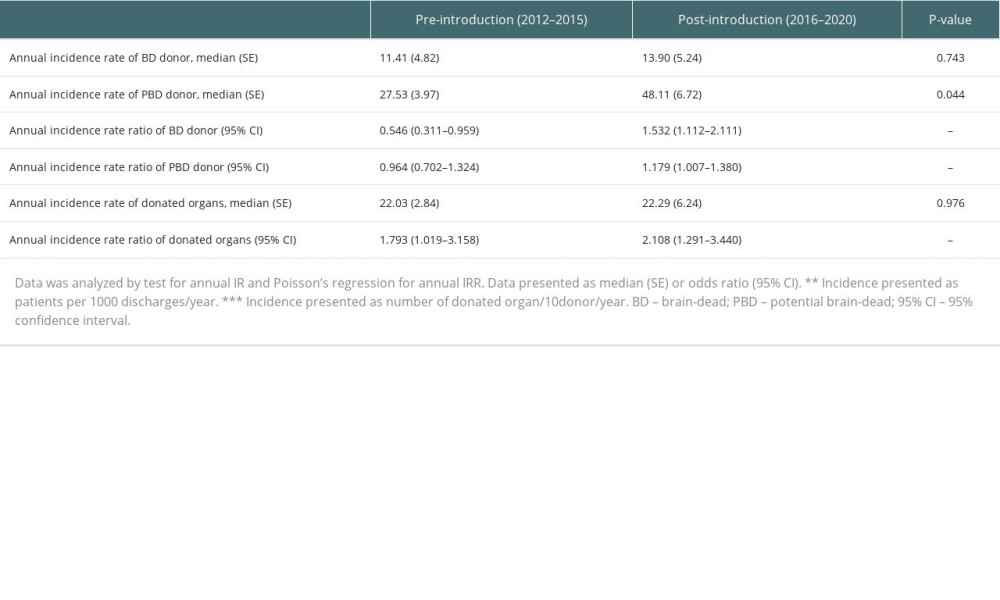 Table 5. Incidence of donated organs during the study period.
Table 5. Incidence of donated organs during the study period.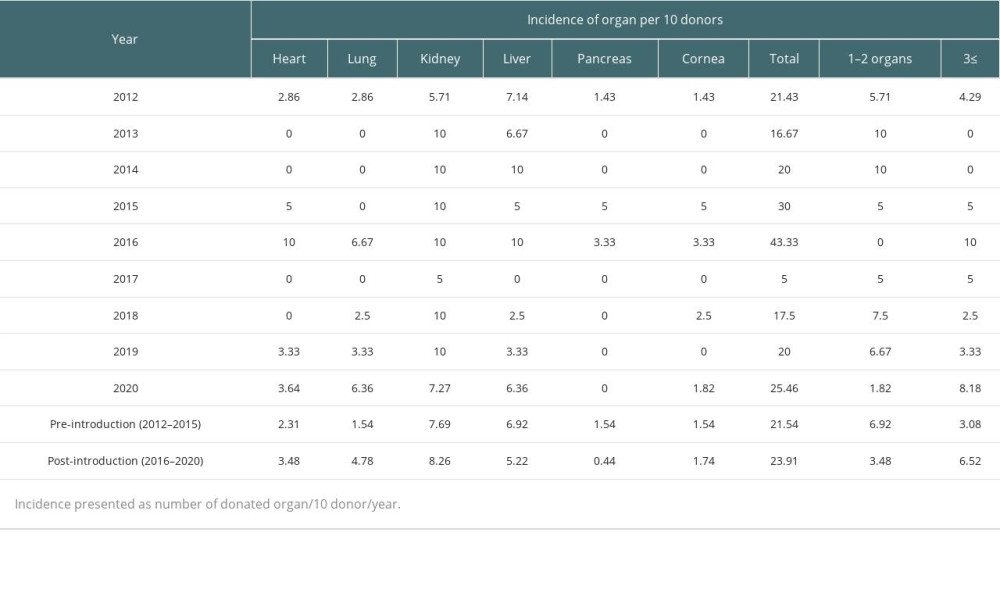 Supplementary Table 1. Reason of donation rejection.
Supplementary Table 1. Reason of donation rejection. Supplementary Table 2. The number of donated organs during the study period.
Supplementary Table 2. The number of donated organs during the study period.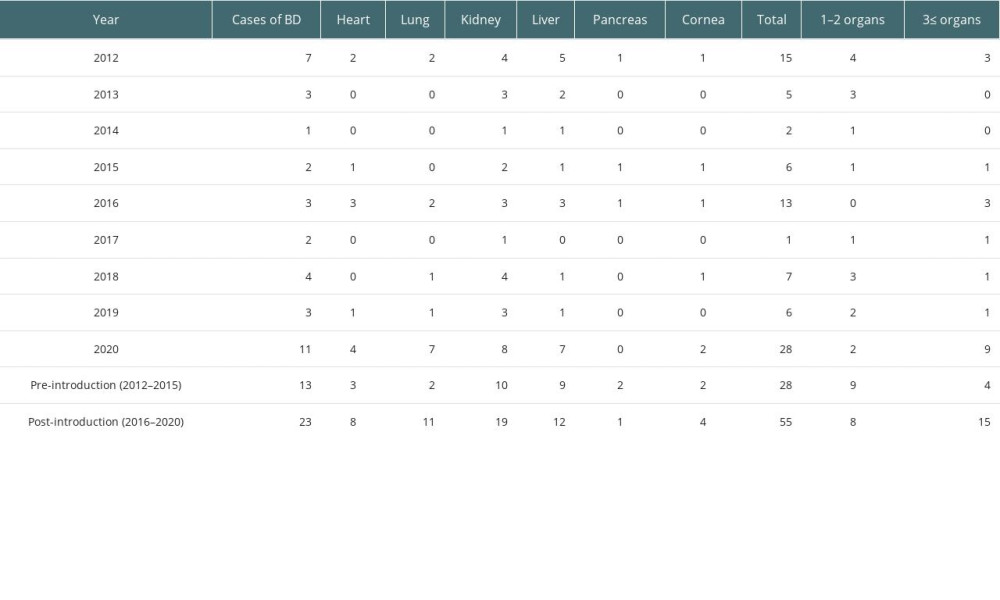
References
1. Abbasi M, Kiani M, Ahmadi M, Salehi B, Knowledge and ethical issues in organ transplantation and organ donation: Perspectives from Iranian health personnel: Ann Transplant, 2018; 23; 292-99
2. : The Korea Network for Organ Sharing
3. Park J, Kim CJ, Recent decrease in organ donation from brain-dead potential organ donors in Korea and possible causes: J Korean Med Sci, 2020; 35(13); e94
4. Salim A, Brown C, Inaba K, Improving consent rates for organ donation: the effect of an inhouse coordinator program: J Trauma, 2007; 62(6); 1411-14 discussion 1414–15
5. Salim A, Martin M, Brown C, Rhee P, The effect of a protocol of aggressive donor management: Implications for the national organ donor shortage: J Trauma, 2006; 61(2); 429-33 discussion 433–35
6. Gridelli B, Remuzzi G, Strategies for making more organs available for transplantation: N Engl J Med, 2000; 343(6); 404-10
7. Duth Transplant Foundation: Annual report 2017 of the Dutch transplant foundation June 25, 2018
8. Jenkins DH, Reilly PM, Schwab CW, Improving the approach to organ donation: A review: World J Surg, 1999; 23(7); 644-49
9. Thet MS, Verzelloni Sef A, Sef D, Can adequate hemodynamic management of brain-dead donors improve donor organ procurement?: World J Transplant, 2022; 12(4); 79-82
10. McKeown DW, Bonser RS, Kellum JA, Management of the heartbeating brain-dead organ donor: Br J Anaesth, 2012; 108(Suppl 1); i96-107
11. Kates OS, Fisher CE, Rakita RM, Use of SARS-CoV-2-infected deceased organ donors: Should we always “just say no?”: Am J Transplant, 2020; 20(7); 1787-94
12. : KODA Annual Report, 2020 https://www.koda1458.kr/newPr/annual.do
13. Kang JM, Kim YJ, Huh K, COVID-19 among solid organ transplant recipients in Korea: surveillance data of the Korean Transplantation Society, January 2020 to March 2022: Korean J Transplant, 2022; 36(2); 159-63
14. Park J, Yang NR, Lee YJ, Hong KS, A single-center experience with an intensivist-led brain-dead donor management program: Ann Transplant, 2018; 23; 828-35
15. Singbartl K, Murugan R, Kaynar AM, Intensivist-led management of brain-dead donors is associated with an increase in organ recovery for transplantation: Am J Transplant, 2011; 11(7); 1517-21
16. Malinoski DJ, Daly MC, Patel MS, Achieving donor management goals before deceased donor procurement is associated with more organs transplanted per donor: J Trauma, 2011; 71(4); 990-95 discussion 996
17. Kim SI, Jeon KO, Son S, Effect of caring for potential brain death organ donors during the organ donation process upon physician attitudes: J Korean Soc Transplant, 2013; 27(3); 92-99
18. Yılmaz Ferhatoglu S, Yapici N, Brain death and organ donation rates in a city hospital: a retrospective study: Cureus, 2019; 11(2); e4006
Figures
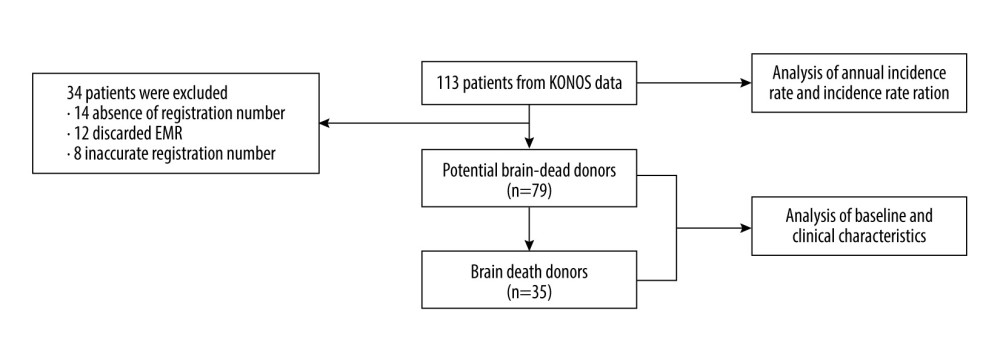 Figure 1. Flow chart depicting the study designEMR – electronic medical record; KONOS – Korea Network for Organ Sharing.
Figure 1. Flow chart depicting the study designEMR – electronic medical record; KONOS – Korea Network for Organ Sharing.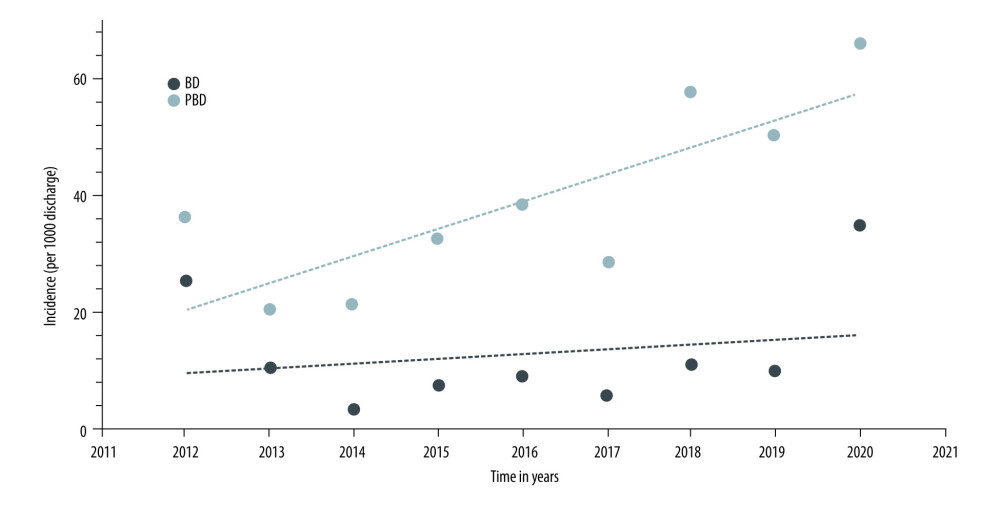 Figure 2. Cumulative incidence of brain-dead (BD) donor and potential brain-dead (PBD) donorIncidence presented as patients per 1000 discharges/year. BD – brain-dead; PBD – potential brain-dead.
Figure 2. Cumulative incidence of brain-dead (BD) donor and potential brain-dead (PBD) donorIncidence presented as patients per 1000 discharges/year. BD – brain-dead; PBD – potential brain-dead.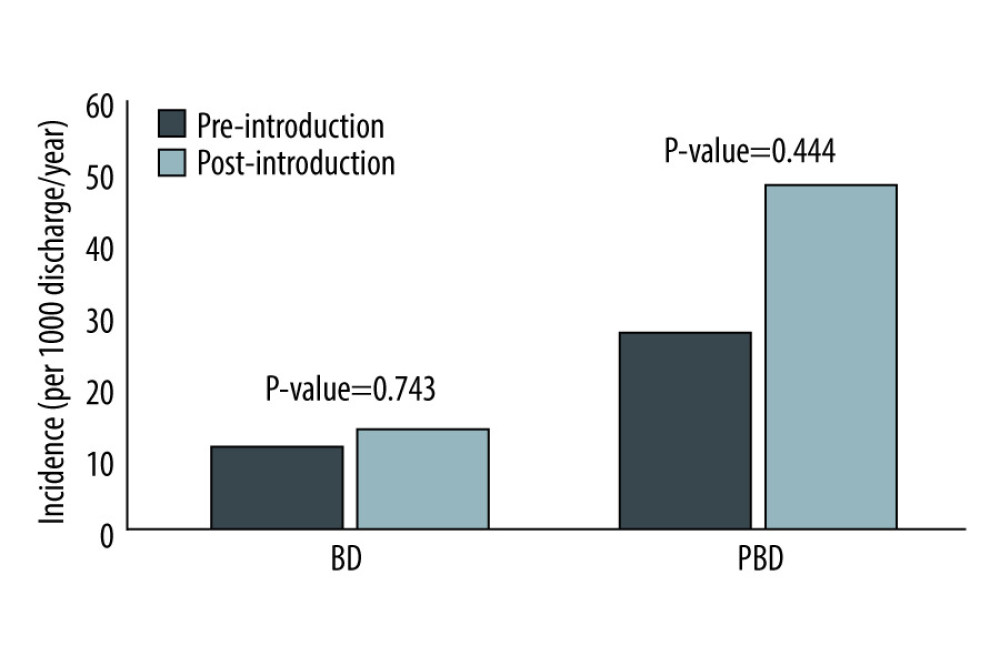 Figure 3. Comparison of incidence rate before and after introduction of dedicated intensivistIncidence presented as patients per 1000 discharges/year. BD – brain-dead; PBD – potential brain-dead
Figure 3. Comparison of incidence rate before and after introduction of dedicated intensivistIncidence presented as patients per 1000 discharges/year. BD – brain-dead; PBD – potential brain-dead Tables
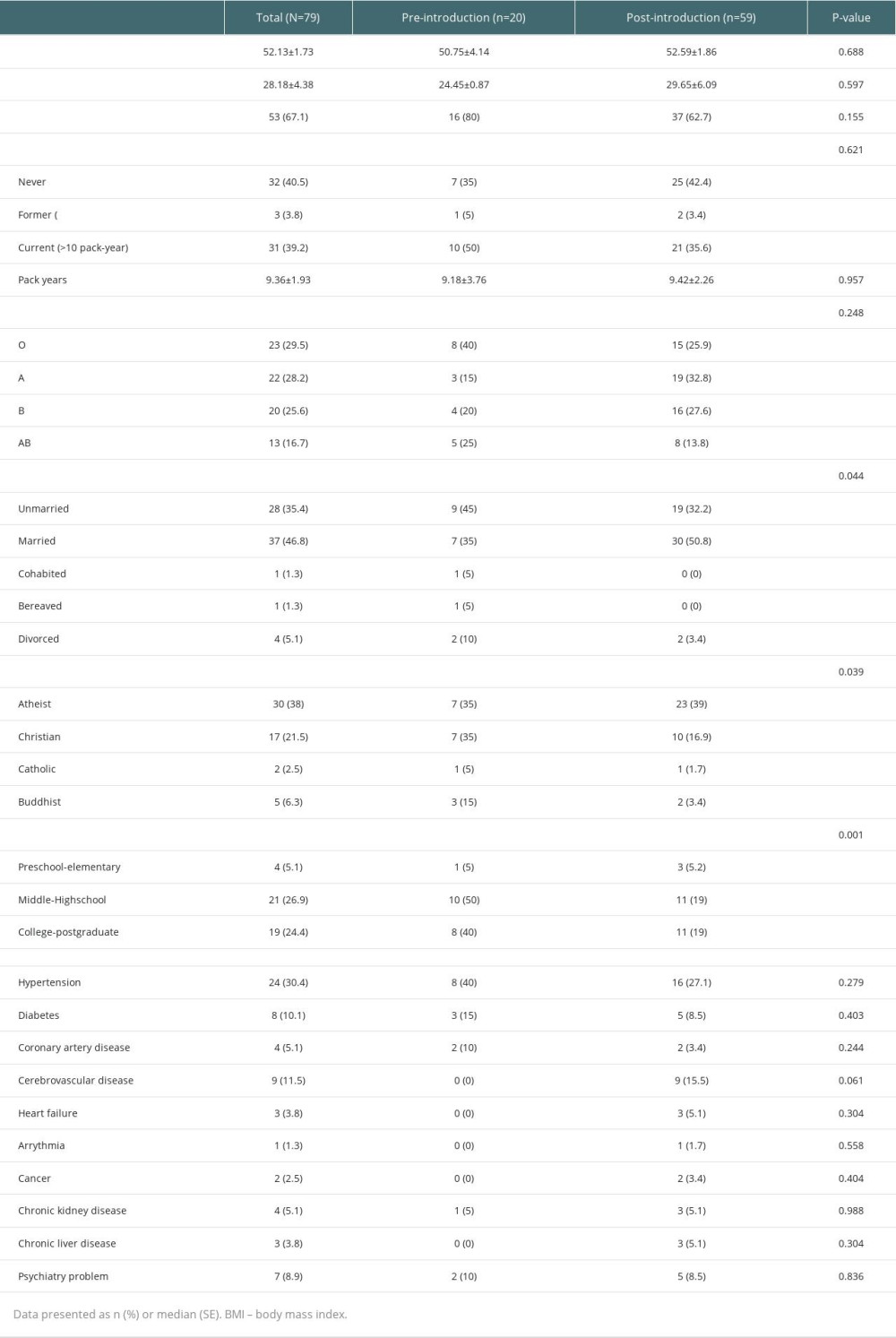 Table 1. Baseline characteristics of pre-introduction and post-introduction groups.
Table 1. Baseline characteristics of pre-introduction and post-introduction groups.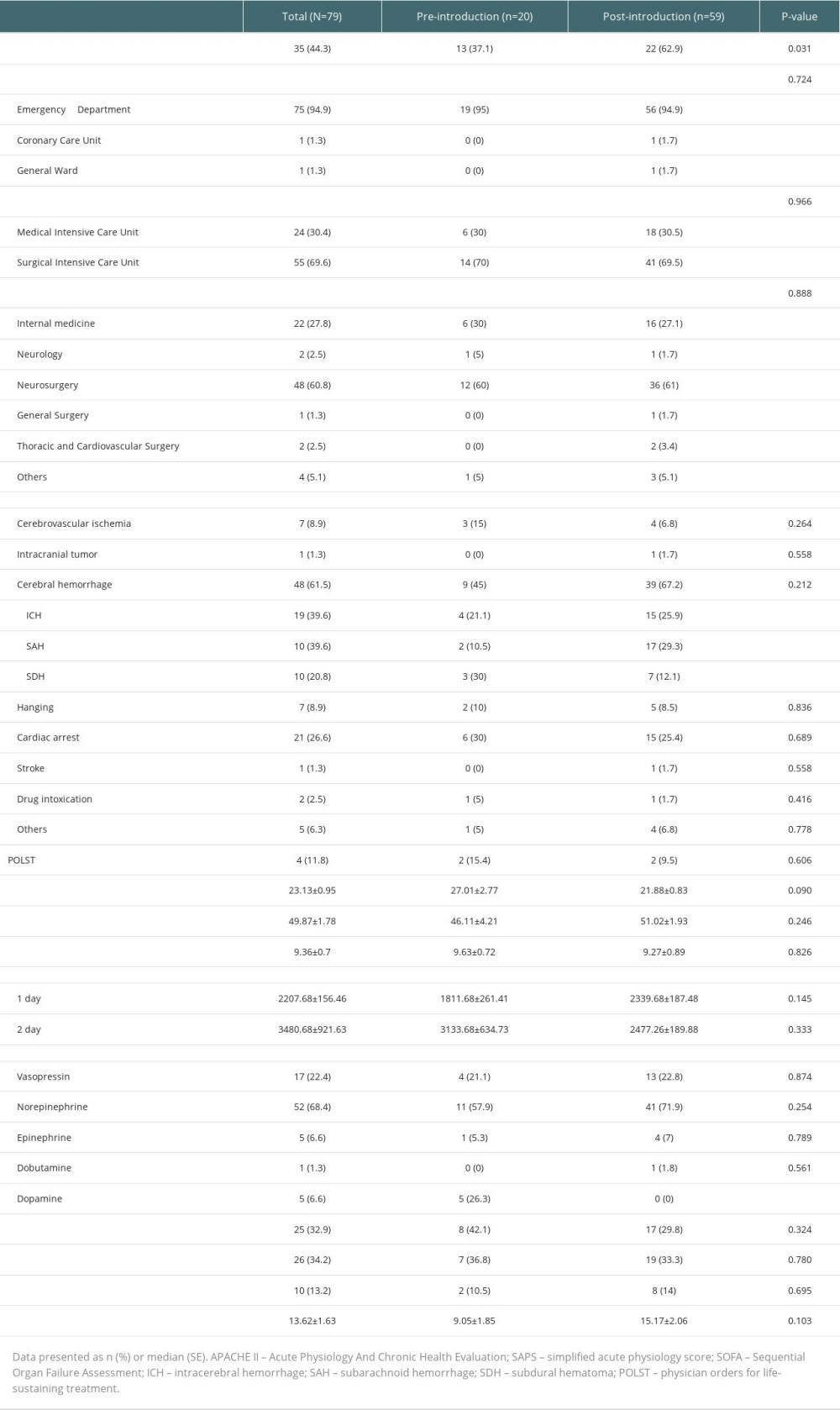 Table 2. Clinical features of pre-introduction and post-introduction groups.
Table 2. Clinical features of pre-introduction and post-introduction groups.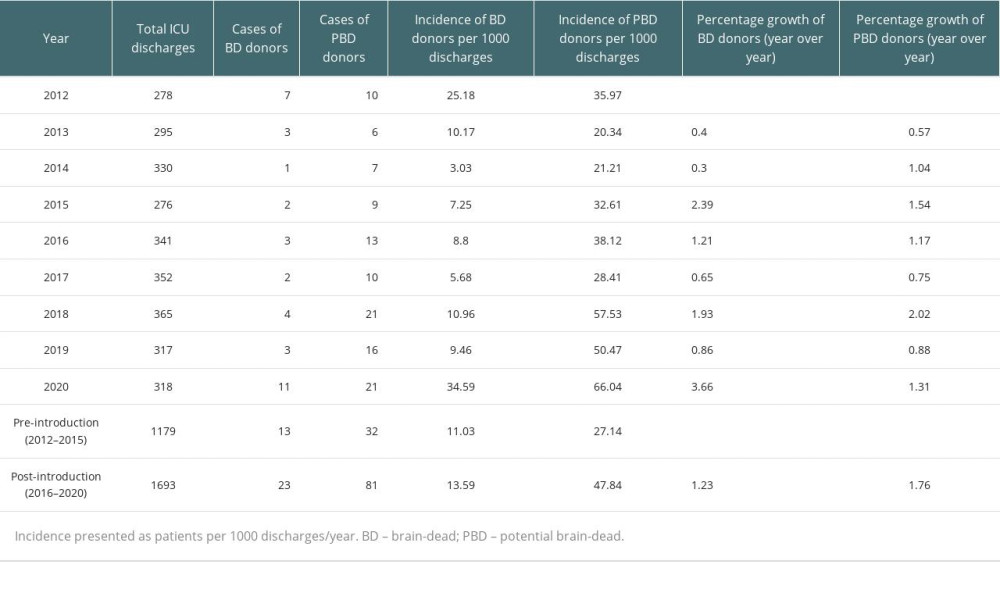 Table 3. Number of brain-dead (BD) donors and potential brain-dead (PBD) donors during the study period.
Table 3. Number of brain-dead (BD) donors and potential brain-dead (PBD) donors during the study period.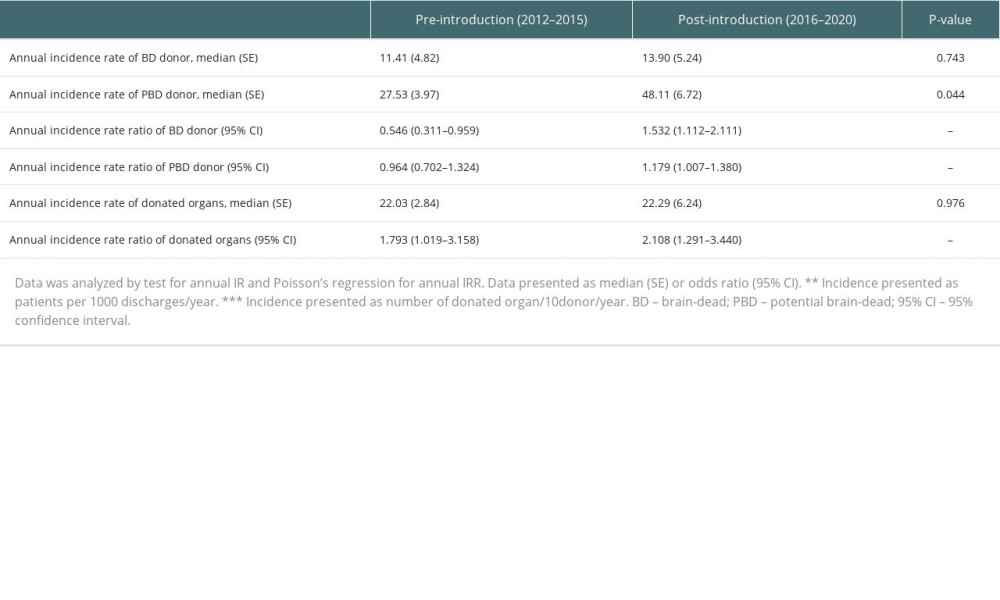 Table 4. Comparison of incidence rate and incidence rate ratio before and after introduction of the intensivist system.
Table 4. Comparison of incidence rate and incidence rate ratio before and after introduction of the intensivist system.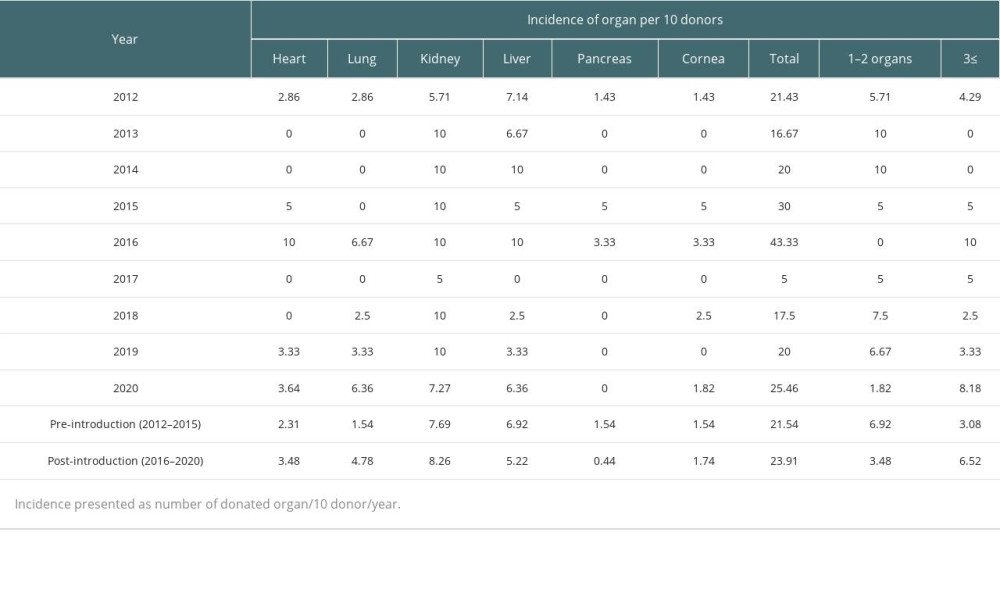 Table 5. Incidence of donated organs during the study period.
Table 5. Incidence of donated organs during the study period.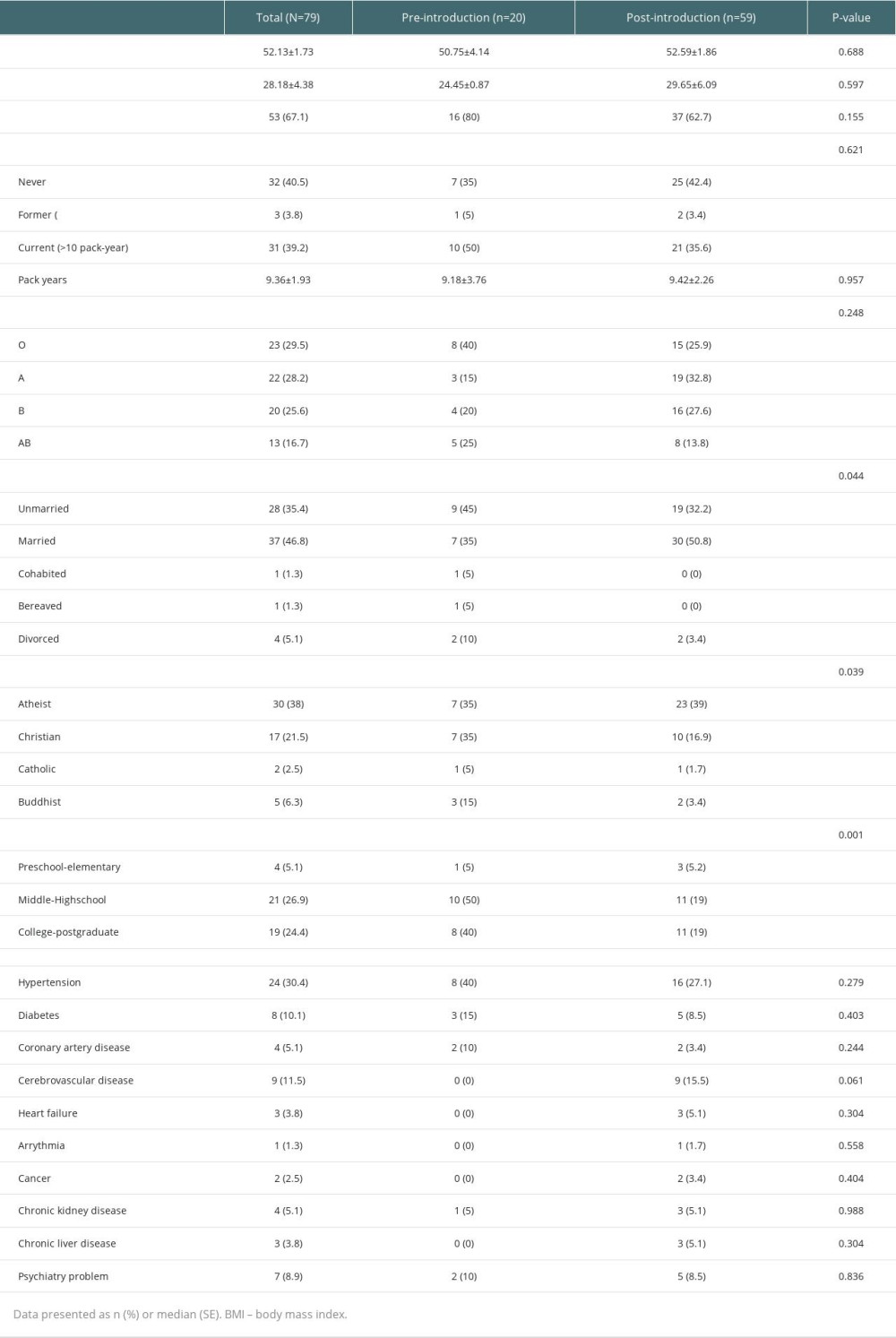 Table 1. Baseline characteristics of pre-introduction and post-introduction groups.
Table 1. Baseline characteristics of pre-introduction and post-introduction groups.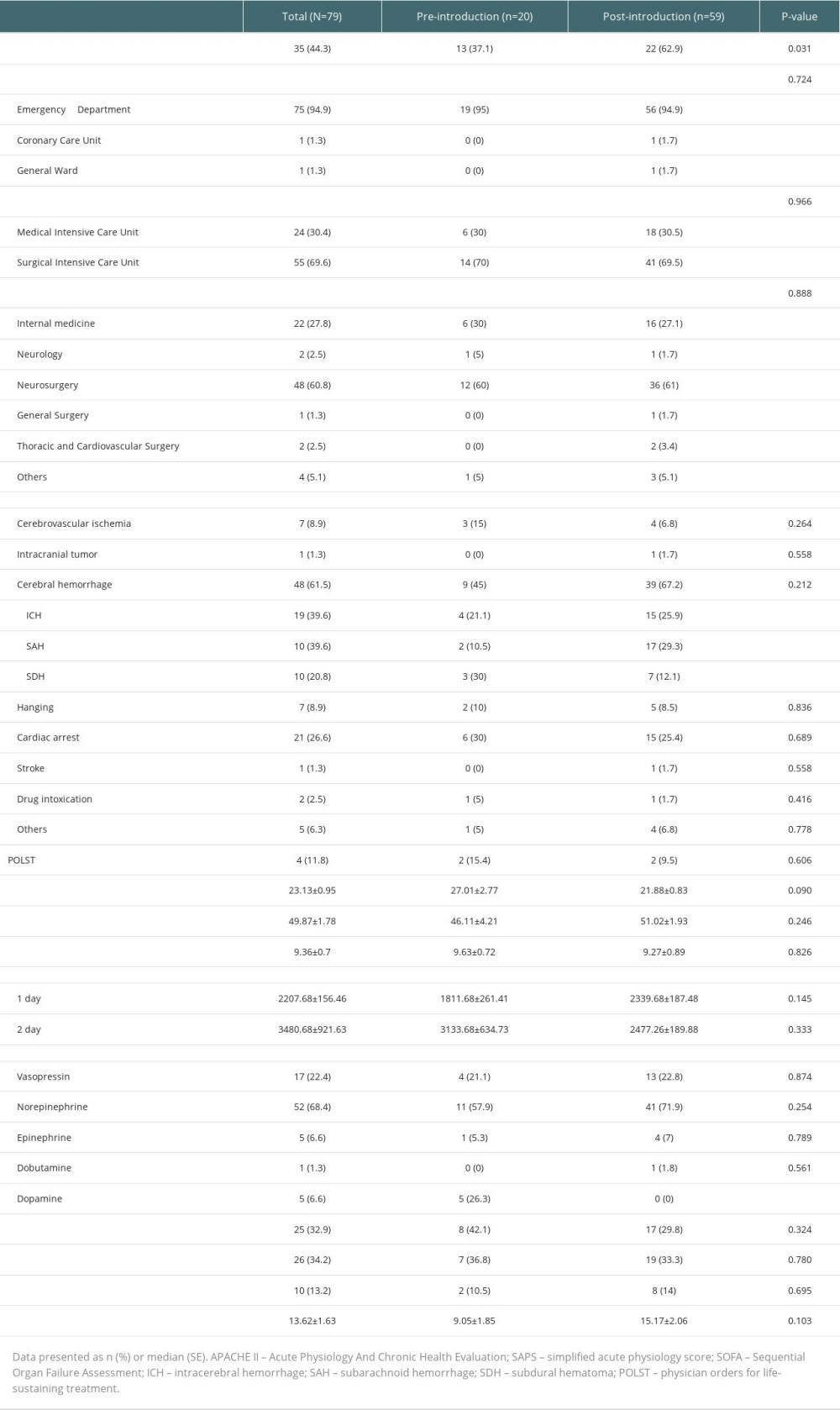 Table 2. Clinical features of pre-introduction and post-introduction groups.
Table 2. Clinical features of pre-introduction and post-introduction groups.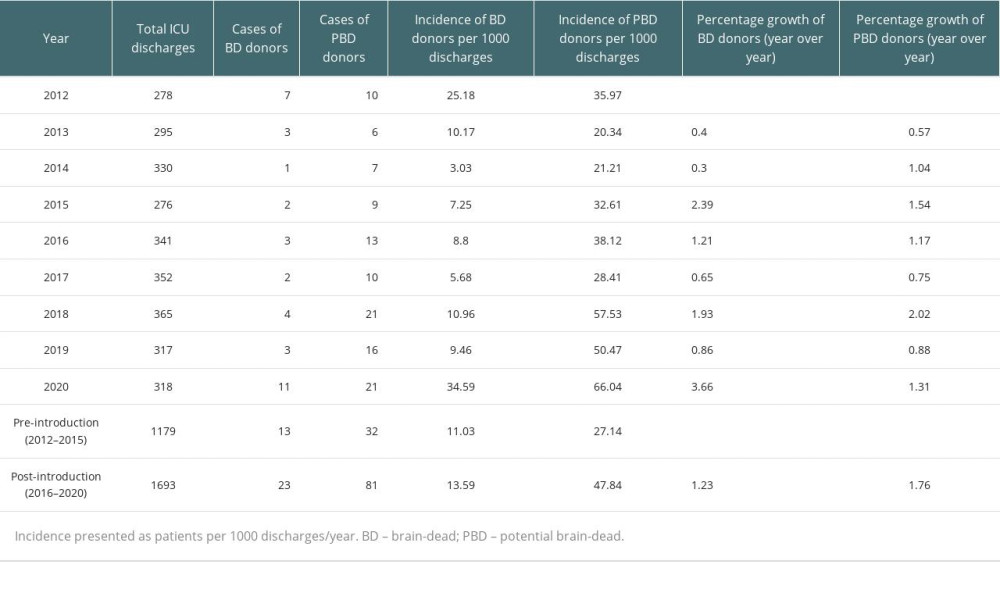 Table 3. Number of brain-dead (BD) donors and potential brain-dead (PBD) donors during the study period.
Table 3. Number of brain-dead (BD) donors and potential brain-dead (PBD) donors during the study period.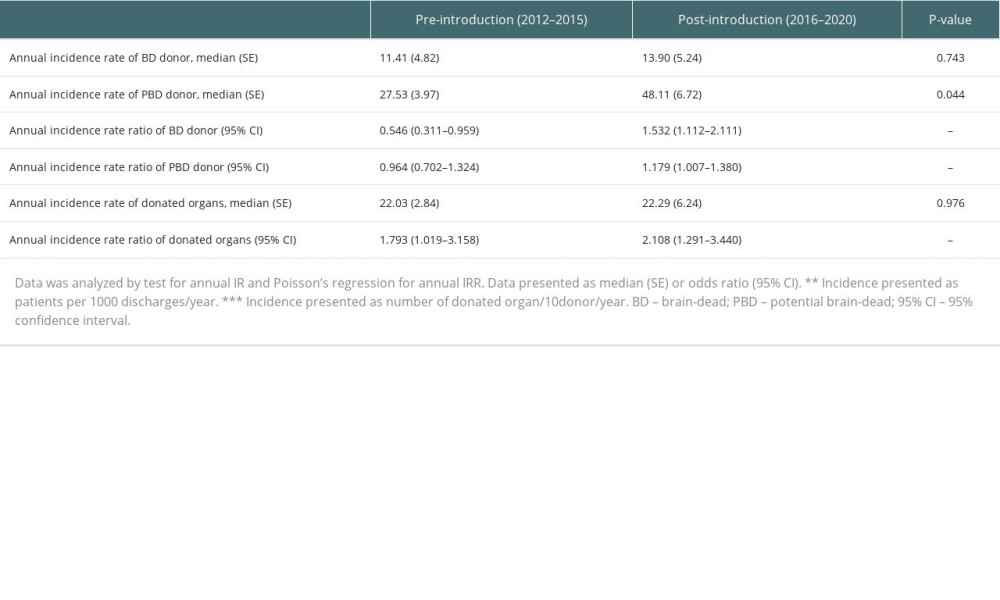 Table 4. Comparison of incidence rate and incidence rate ratio before and after introduction of the intensivist system.
Table 4. Comparison of incidence rate and incidence rate ratio before and after introduction of the intensivist system.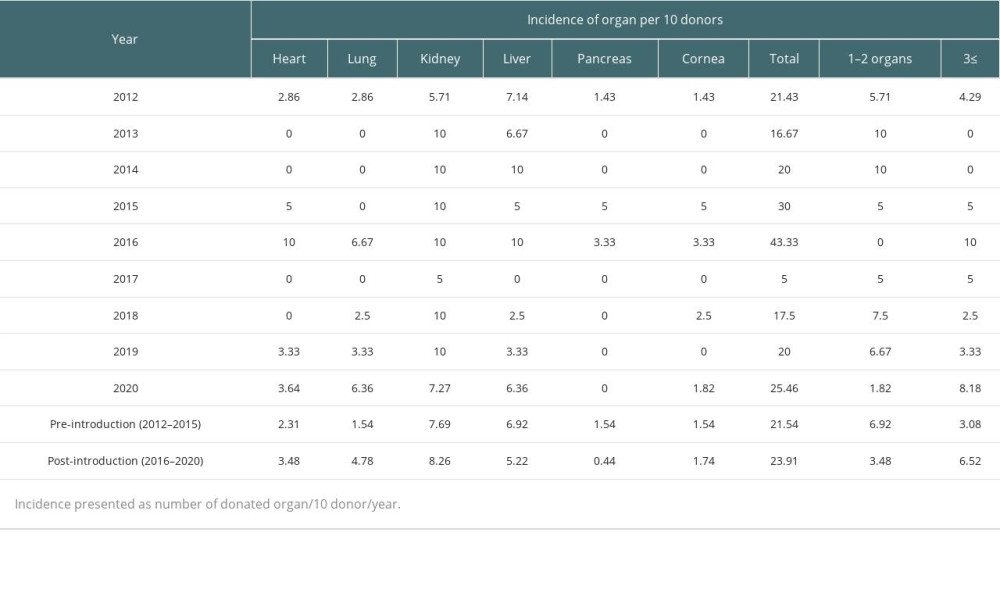 Table 5. Incidence of donated organs during the study period.
Table 5. Incidence of donated organs during the study period. Supplementary Table 1. Reason of donation rejection.
Supplementary Table 1. Reason of donation rejection.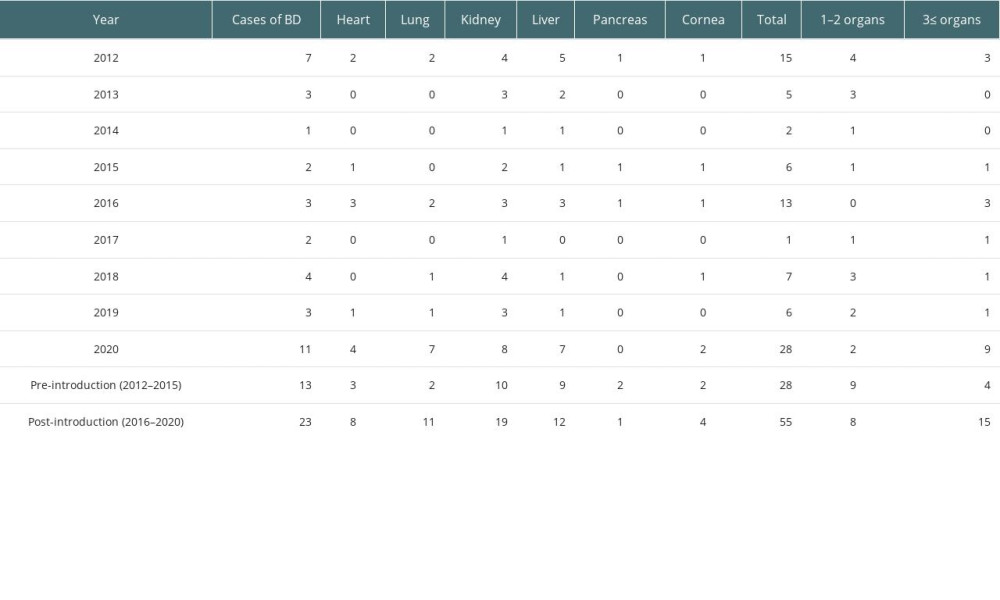 Supplementary Table 2. The number of donated organs during the study period.
Supplementary Table 2. The number of donated organs during the study period. In Press
15 Mar 2024 : Review article
Approaches and Challenges in the Current Management of Cytomegalovirus in Transplant Recipients: Highlighti...Ann Transplant In Press; DOI: 10.12659/AOT.941185
18 Mar 2024 : Original article
Does Antibiotic Use Increase the Risk of Post-Transplantation Diabetes Mellitus? A Retrospective Study of R...Ann Transplant In Press; DOI: 10.12659/AOT.943282
20 Mar 2024 : Original article
Transplant Nephrectomy: A Comparative Study of Timing and Techniques in a Single InstitutionAnn Transplant In Press; DOI: 10.12659/AOT.942252
28 Mar 2024 : Original article
Association Between FEV₁ Decline Rate and Mortality in Long-Term Follow-Up of a 21-Patient Pilot Clinical T...Ann Transplant In Press; DOI: 10.12659/AOT.942823
Most Viewed Current Articles
05 Apr 2022 : Original article
Impact of Statins on Hepatocellular Carcinoma Recurrence After Living-Donor Liver TransplantationDOI :10.12659/AOT.935604
Ann Transplant 2022; 27:e935604
12 Jan 2022 : Original article
Risk Factors for Developing BK Virus-Associated Nephropathy: A Single-Center Retrospective Cohort Study of ...DOI :10.12659/AOT.934738
Ann Transplant 2022; 27:e934738
22 Nov 2022 : Original article
Long-Term Effects of Everolimus-Facilitated Tacrolimus Reduction in Living-Donor Liver Transplant Recipient...DOI :10.12659/AOT.937988
Ann Transplant 2022; 27:e937988
15 Mar 2022 : Case report
Combined Liver, Pancreas-Duodenum, and Kidney Transplantation for Patients with Hepatitis B Cirrhosis, Urem...DOI :10.12659/AOT.935860
Ann Transplant 2022; 27:e935860








