04 November 2022: Original Paper
Revisiting the “Weekend Effect” on Adult and Pediatric Liver and Kidney Offer Acceptance
Takayuki Yamamoto1ABCDEF*, Anushi Shah1E, Mike Fruscione1E, Shoko Kimura1E, Nahel Elias1E, Heidi Yeh1E, Tatsuo Kawai1E, James F. Markmann1ADEGDOI: 10.12659/AOT.937825
Ann Transplant 2022; 27:e937825
Abstract
BACKGROUND: Weekends can impose resource and manpower constraints on hospitals. Studies using data from prior allocation schemas showed increased adult organ discards on weekends. We examined the impact of day of the week on adult and pediatric organ acceptance using contemporary data.
MATERIAL AND METHODS: Retrospective analysis of UNOS-PTR match-run data of all offers for potential kidney and liver transplant from 1/1/2016 to 7/1/2021 were examined to study the rate at which initial offers were declined depending on day of the week. Risk factors for decline were also evaluated.
RESULTS: Of the total initial adult/pediatric liver and kidney offers, the fewest offers occurred on Mondays and Sundays. The decline rate for adult/pediatric kidneys was highest on Saturdays and lowest on Tuesdays. The decline rate for adult livers was highest on Saturday and lowest on Wednesday. In contrast, the decline rate for pediatric livers was highest on Tuesdays and lowest on Wednesdays. Independent risk factors from multivariate analysis of the adult/pediatric kidney and liver decline rate were analyzed. The weekend offer remains an independent risk factor for adult kidney and liver offer declines, but for pediatric offers, these were not significant independent risk factors.
CONCLUSIONS: Although allocation systems have changed, and the availability of kidneys and livers have increased in the USA over the past 5 years, the weekend effect remains significant for adult liver and kidney offers for declines. Interestingly, the weekend effect was not seen for pediatric liver and kidney offers.
Keywords: Liver Transplantation, Kidney Transplantation, Tissue and Organ Procurement, Adult, Child, Humans, Liver, Risk Factors, Kidney
Background
A significant increase in the discard of deceased-donor kidneys [1,2] or livers [3] during the weekend has been a source of concern in the United States. However, these studies were performed based on data prior to implementation of the new kidney allocation system (KAS) in December 2014. In addition, the discard of deceased-donor kidneys or livers often occurs following organ procurement and, as a result, additional information is available that may have affected acceptance, including organ damage, adequate organ flush, biopsy findings, extracranial malignancy, and abnormal anatomy, all of which are generally difficult to discover in the United Network for Organ Sharing (UNOS) data.
The decision to decline or accept at the time of the initial offer can affect the final acceptance. The “weekend effect” refers to the increased rate of kidney and liver declines over the weekend. King et al examined initial offer data of adult deceased-donor kidneys from 2008 to 2015 to evaluate the weekend effect [4]. However, no new studies of the weekend effect have been conducted since the new KAS was implemented, nor has the pediatric population been examined. Furthermore, there are no reports that evaluated what risk factors of declined livers related to initial offer, including pediatric deceased donors.
The aims of this study were to compare (i) the decline rate to initial offer of kidneys and livers from adult/pediatric deceased donors by day of the week using the most recently available data, (ii) the sequence number for accepted offers to the initial offer (ie, the number of offers made to matched candidates before a given organ was ultimately accepted for transplantation, with a smaller acceptance sequence number indicating fewer declined offers before acceptance, as previously described [4]) of each group by day of the week, and (iii) the decline (not transplanted, including not procured and discarded organs) rate to final offer of each groups. These analyses may yield insight into the current trend of deceased-donor kidney and liver offer acceptance rates and may identify approaches to promote increased utilization of marginal donor livers and kidneys.
Material and Methods
DATA SOURCE AND STUDY DESIGN:
This was a retrospective cohort study using UNOS Potential Transplant Recipient (PTR) data to evaluate match-run data of all offers for kidney and liver transplant from deceased donors from January 1, 2016 (Friday) to July 1, 2021 (Thursday) to examine: (i) the decline rate (“yes” or “provisional yes” at the initial offer as defined as accepted and “no” at the initial offer as defined declined) of kidneys and livers from adult (≥18 years old [y.o.]) deceased donors (Group A) or pediatric (<18 y.o.) deceased donors (Group B) on the basis of the day of the week of the initial offer, and (ii) the sequence number among accepted offers for potential deceased kidney or liver transplantation from Group A or Group B on the basis of the day of the initial offer. The potential deceased-donor characteristics were identified using UNOS Standard Transplant Analysis and Research (STAR) files based on the National Organ Procurement and Transplantation Network (OPTN) database as of July 2, 2021.
In this study, 117 074 potential deceased-donor kidneys and 69 214 potential deceased-donor livers for the most recent 5.5-year period were enrolled. We evaluated organ quality of a kidney by calculating the KDPI. Therefore, we excluded 7680 kidney donors with missing KDPI data or other key data. For the liver donors, no single factor was defined in the PTR-STAR files that reflected organ quality, such as KDPI for a kidney. Feng et al created a donor risk index based on donor and graft characteristics (age, DCD, split/partial status, donor race, height, and cause of brain death) that are significantly and independently associated with increased failure of deceased-donor liver transplants [5]. Furthermore, DCD donor livers differ vastly from brain-dead donors in terms of risk, and many DCD liver donor candidates were not transplanted by the liver recovery because the donor did not die in a timely manner. Therefore, we excluded DCD liver donors (n=11 482) and 8256 liver donors missing potential data – age, gender, race, cause of death, h/o hypertension and diabetes, h/o alcohol use, terminal ALT/AST/T-bilirubin (T-bil), BMI, HBc-Abs and HCV-Abs status – to evaluate the organ quality of a liver in the study, as previously published [3]. Ultimately, we enrolled 109 394 kidneys (Figure 1) and 49 476 livers (Figure 2) from deceased donors in this study. To assess the weekend effect, we defined the weekend as Saturday and Sunday offers, whereas offers from Monday to Friday were counted as weekday offers, as previously described [6,7]. All data were de-identified; therefore, no Institutional Review Board approval was required.
STATISTICAL ANALYSIS:
Continuous variables were expressed as mean±standard deviation (SD). Comparisons between 2 groups were performed using a Mann-Whitney test for nonparametric values or a
Results
Deceased Donor Characteristics
:
In Group A, kidneys from older people (especially ≥60 y.o.), women, African Americans (AA), stroke as the cause of death, history of hypertension and diabetes, fewer heavy alcohol use donors, more tobacco-using donors, higher hematocrit (Hct), lower pH, less serum Na ≥160, serum BUN and creatinine, especially serum creatinine >2.5, proteinuria, obese (BMI ≥30), shorter height, longer cardiac arrest period, clinical systemic infection, KDPI (especially ≥85%), HBV/HCV-positive and weekend (Saturday/Sunday) offers were significant factors associated with organ decline at the initial offer. In Group B, kidneys from younger people (especially less than 6 y.o.), anoxia as the cause of death, serum BUN and creatinine (especially serum creatinine >2.5), thin (lower BMI), shorter height, KDPI (especially over 85%), and DCD donors were significant factors associated with decline at the initial offer.
:
In Group A, donor age ≥60 y.o., women, less AA and more Hispanic race, stroke as the cause of death, h/o hypertension and diabetes, more alcohol use, more tobacco use, higher Hct, lower pH, less high serum sodium (Na ≥160), high transaminase (especially ALT >500 and total bilirubin [T-bil] >10), obese (especially BMI ≥30), shorter height, HBV/HCV-positive and weekend offer were significant factors associated with offer decline at the initial offer. In Group B, donor age <6 y.o., anoxia as the cause of death, lower pH, high transaminase (especially ALT >500 and T-bil >10), lower BMI, shorter height, and HBV-positive donors were significantly associated with decline at the initial offer.
KIDNEYS FROM DECEASED DONORS: In Group A, Monday offers were the least frequent (13.3%), followed by Sunday (13.5%). Wednesday (15.0%) offers were the most frequent, followed closely by Thursdays (14.9%) and Tuesdays (14.8%) (Figure 3, Supplementary Table 1).
This trend was similar to that observed by Mohan et al using data from 2000-2013 [1].
In Group B, the initial offers from deceased pediatric kidney donors were similar to that of adults, with the fewest offers on Mondays (13.5%). Fridays had the most offers (15.0%), followed by Wednesdays (14.8%) and Thursdays (14.6%) (Figure 3, Supplementary Table 1).
LIVERS FROM DECEASED DONORS: In Group A, Sundays had the fewest offers (13.3%), followed by Mondays (13.4%), similar to that for kidneys. Wednesdays (15.2%) had the greatest number of initial offers, followed by Tuesdays (15.0%) and Thursdays (14.8%), with a pattern similar to that seen for kidneys (Figure 3, Supplementary Table 2).
The trend of initial offers from potential pediatric livers was similar to those from adult livers (Figure 3, Supplementary Table 2).
KIDNEYS FROM DECEASED DONORS: In Group A, the initial offers on Saturdays (12.5%) and Sundays (12.2%) were declined more frequently than for other days. The declined rate of initial offer on Fridays (11.5%) was similar to Mondays (11.6%) and Thursdays (11.4%). Tuesdays (10.7%) had the lowest declined rate of the week (Figure 4, Supplementary Table 1). Mean sequence numbers among the accepted group for the initial offers on Saturdays (mean: 430.7) and Sundays (460.3) were also higher than for other days (Table 3). The declined rate of final offer on Saturdays (17.1%) and Sundays (17.1%) was also higher than that of other days (Figure 4, Supplementary Table 1).
In Group B, Saturdays (8.4%) and Sundays (8.4%) had the highest decline rates of the week, similar to Group A. Tuesdays (6.8%) had the lowest decline rate of the week, similar to Group A (Figure 4, Supplementary Table 1). Mean sequence numbers among accepted initial offers on Saturdays (327.3) and Sundays (314.2) were also more than for other days, similar to adult kidneys (Table 3). The declined rate of final offer on Saturdays (12.4%) and Sundays (12.8%) was also more than for other days (Supplementary Table 1).
In summary, the decline rate of initial offers of adult kidneys was significantly higher during the weekend (12.4%) compared to weekdays (11.2%) (P<0.001) (Table 3). The mean sequence number of accepted kidneys on weekends (445.2) was also significantly higher than that on weekdays (397.0) (P=0.001), indicating that on the weekend it was harder to place a kidney compared to on weekdays. Our results also demonstrated the final decline rate on weekends (18.8%) was also significantly higher than for weekdays (15.1%) (P<0.001) (Table 3). In contrast, the decline rate of initial offers of pediatric kidneys was not significantly different on weekends (8.4%) than on weekdays (7.5%) (Table 3). However, the mean sequence number of accepted kidneys in weekends (320.9) was also significantly higher than for weekdays (226.2) (P=0.004). In addition, the final decline rate in weekend (14.2%) was also significantly higher than on weekdays (10.3%) (P<0.001) (Table 3).
LIVERS FROM DECEASED DONORS: In Group A, the initial offer on Wednesdays was declined less than other days, whereas decline rates on other days were similar (Figure 4, Supplementary Table 2). Mean sequence number among accepted initial offers on Sundays was lower compared to other days (Supplementary Table 2). Final offers on Fridays [16.2%] and Saturdays [16.5%] were declined more often than on other days (Figure 4, Supplementary Table 2).
In Group B, the initial offer occurring on Wednesdays (5.3%) and Thursdays (5.6%) was declined less than on other days (Figure 4, Supplementary Table 2). The mean sequence number among the accepted group for initial offers varied depending on day of the week (Supplementary Table 2). Final offer on Fridays [18.5%] was declined more than other days (Figure 4, Supplementary Table 2).
In summary, the decline rate of initial offers of adult livers was significantly higher on weekends (7.7%) compared with weekdays (7.0%) (P=0.012) (Table 3). However, the mean sequence number of accepted livers on the weekend (79.7) was not significantly different from the weekdays (87.0). The final decline rate on the weekend (17.5%) was significantly higher than on weekdays (15.2%) (P<0.001) (Table 3). On the other hand, the decline rate of initial offers of pediatric livers was not significantly different on weekends (6.5%) from weekdays (6.4%) (Table 3). The mean sequence number of accepted livers on the weekend (72.9) was also not significantly different from that of weekdays (68.6). As a result, the final decline rate on weekends (16.5%) was also not significantly different from weekdays (15.7%) (Table 3).
ADULT DONORS VERSUS PEDIATRIC DONORS:
The decline rates of both initial and final offer of pediatric kidneys were significantly lower than for adult kidneys (odds ratio [OR]: 0.65 at the initial offer, 0.66 at the final offer, P<0.001) (Supplementary Table 3). However, the decline rates of both initial and final offer of pediatric livers were not significantly different from that for adult livers (Supplementary Table 3).
ADULT DECEASED KIDNEY DONORS: Multivariable analysis indicated that age ≥60 y.o. (OR: 1.92), h/o hypertension (OR: 1.50), h/o diabetes (OR: 1.90), tobacco use (OR: 1.18), terminal pH <7.4 (OR: 1.09), terminal serum Cre >2.5 (OR: 2.18), proteinuria (OR: 1.13), KDPI ≥85% (OR: 2.43), HBVc-Abs-positive (OR: 1.31), HCV-Abs-positive (OR: 2.21), and weekend offer (OR: 1.11) of adult deceased kidney donors were independent risk factors for decline for the initial offers (Table 4). Conversely, terminal Na ≥160 mg/dL of the donors was independently associated with reduced rates of decline for the initial offer (Table 4).
PEDIATRIC DECEASED KIDNEY DONORS: In the multivariable analysis, independent risk factors for an initial offer being declined were height <100 cm (OR: 3.17), terminal serum Cre >2.5 (OR: 2.57), and KDPI ≥85% (OR: 2.59) (Table 5).
ADULT DECEASED LIVER DONORS: In the multivariable analysis, independent risk factors associated with initial offer decline of adult deceased liver donors were age ≥60 y.o. (OR: 1.47), stroke as the cause of death (OR: 1.18), h/o hypertension (OR: 1.17), h/o diabetes (OR: 1.33), heavy alcohol use (OR: 1.67), terminal pH <7.4 (OR: 1.10), terminal ALT >500 (OR: 2.88), terminal T-bil >10 (OR: 5.89), BMI ≥30 (OR: 1.51), HBVc-Abs-positive (OR: 1.47), HCV-Abs-positive (OR: 1.55), and weekend offer (OR: 1.11) (Table 6). Conversely, AA race (OR: 0.64) and terminal Na ≥160 mg/dL (OR: 0.84) were independent factors associated with reduced rates of initial offer decline (Table 6).
PEDIATRIC DECEASED LIVER DONORS: Multivariable analysis showed that independent risk factors associated with initial offer decline of pediatric deceased liver donors were age <6 y.o. (OR: 1.86), ALT >500 (OR: 4.45), terminal T-bil >10 (OR: 9.11), and HBVc-Abs-positive (OR: 4.23) (Table 7).
In summary, kidneys and livers from adult donors demonstrated a weekend effect for their initial offer decline. On the other hand, organs from pediatric donors did not reveal a weekend effect for refusal of initial offers.
INDEPENDENT RISK FACTORS FOR DISCARDING KIDNEYS OR LIVERS:
At the time of the final decision to accept an organ for transplant, additional information is available, including kidney and liver biopsy findings, anatomy, and use of pump preservation are available to discern the offered organ’s quality. The initial offer response appears to be strongly correlated with final acceptance. However, to evaluate the relationship of the weekend effect with the final declined rate, the risk factors associated with decline at the time of the final offer (ie, discarding kidneys or livers) were examined.
ADULT DECEASED KIDNEY DONORS: In the multivariable analysis, independent risk factors associated with discarding adult kidneys were declined at the initial offer (OR: 207.0), weekend effect (OR: 1.19), cancer at procurement (OR: 1.93), and number of organs discarded (OR: 5.04) (Table 8). Conversely, perfusion pump use (OR: 0.62) was independently associated with fewer adult kidney discards (Table 8).
PEDIATRIC DECEASED KIDNEY DONORS: In the multivariable analysis, independent risk factors associated with discarding pediatric kidneys were declined at the initial offer (OR: 170.0), weekend effect (OR: 1.34), and number of organs discarded (OR: 3.57) (Table 8). Conversely, pump preservation (OR: 0.42) was an independent predictive factor associated with fewer discarded pediatric kidneys (Table 8).
ADULT DECEASED LIVER DONORS: In the multivariable analysis, independent risk factors associated with discarding adult livers were decline at the initial offer (OR130.0), macrosteatosis >30% (OR: 7.71), fibrosis (OR: 2.08), and numbers of organ discarded (OR: 2.21) (Table 9). Conversely, pump use (OR: 0.28) of the donors was an independent predictor of fewer discarded adult livers (Table 9).
PEDIATRIC DECEASED LIVER DONORS: In the multivariable analysis, independent risk factors associated with discarding pediatric livers were declined of the initial offer (OR143.0), macrosteatosis >30% (OR: 10.7), and number of organs discarded (OR: 2.8) (Table 9).
In summary, discarded kidneys from adult and pediatric donors demonstrated the weekend effect, but discarded livers did not have a weekend effect.
Discussion
ADULT DONOR KIDNEYS:
With respect to initial offers of adult kidney, KDPI ≥85%, HCV-positive and terminal Cre >2.5 donors are highest independent risk factors for declining the initial offer. Numerous studies showed high KDPI kidneys continue to be difficult to allocate [9–11], with a discard rate over 50% [11]. Even though the most recent data was used in this study, KDPI ≥85% kidneys still experienced a 2.43 times greater decline rate for the initial offer compared to KDPI<85% kidneys. Recently, several studies noted that AKI of deceased donor did not affect graft survival [12–14], though this does not necessarily predict the outcome of similar high KDPI kidneys that were discarded. However, the present study revealed that terminal Cre >2.5 donor was still a higher risk factor to decline than the initial offer. In recent years, the proportion of deceased donors who have HCV viremia has increased in the USA, from 3.5% in 2015 to 6.5% in 2019 [15]. The introduction of HCV direct-acting antiviral therapies has provided an opportunity to expand the utilization of kidneys from HCV-viremic donors. Despite this highly effective therapy, HCV viremia status has been reported as an independent risk factor for discard (odds ratio 2.29) [16]. The present data also indicated a similar trend, with HCV-viremic donor’s kidneys 2.21 times more likely to be declined on the initial offer than HCV negative kidneys.
Although as expected, initial offer decline was an independent risk factor to the final decline kidneys for transplant, weekend transplant date (Sat/Sun) remained an independent risk factor to decline adult kidneys for transplant (Table 8). Interestingly, kidney biopsy was not observed to be a risk factor to decline kidneys for transplant. In addition, pump use for kidneys was a negative predictive factor to decline kidneys for transplant (Table 8). The data suggest that greater pump preservation for adult kidneys which are offered on the weekend, and the attempt to delay weekend offers to Monday using pump preservation, may increase utilization rates and the impact of the weekend may decrease.
PEDIATRIC DONOR KIDNEYS:
KDPI ≥85%, height <100cm and terminal Cre >2.5 donors carry the highest independent risk factors leading to decline of the initial offer. Since calculation of KDPI uses height and terminal creatinine, small pediatric donor conferred the greatest risk to decline the initial offer of pediatric kidneys in the present study. This trend parallels a previous report evaluating the risk factors for discarded pediatric donor kidneys [17]. Since small pediatric kidneys have the potential risk for graft thrombosis [18] and urologic complications [19], transplant centers still tend to decline small pediatric kidneys. However, Troppmann et al reported that small pediatric donor AKI did not increase risk for early graft loss or decrease long-term function [20]. To increase the use of small pediatric donor AKI kidneys, a special allocation system may be required. For example, in high-volume transplant centers, the use of a single small pediatric donor kidney for transplantation is as successful as with larger pediatric or adult living donors [18]. If OPTN elects to preferentially allocate these unique kidneys to specialized transplant centers, the discarded rate may be reduced.
Even though the weekend effect was not observed with the initial offer, the weekend effect was an independent risk factor in the ultimate decline of pediatric kidneys for transplant. This phenomenon may be attributable to the limited resources availability on weekends [21].
ADULT DONOR LIVERS:
Donor liver quality (terminal ALT >500, T-bil >10), h/o heavy alcohol use, HCV positivity, and BMI ≥30 are independent risk factors for decline of the initial liver offer. Previous studies showed these factors were also independent discard risk factors: ALT >500 (22), T-bil >10 [22], HCV-positive [3, 22], and BMI ≥30 [3]. In other words, if a donor has those factors, fewer transplant centers are likely to accept the liver based on the initial offer, and the liver will more likely be declined as a result. However, current data indicate final bilirubin and peak ALT of donors were not associated with increased risk of graft failure after liver transplant [23]. Similar to kidney donors, HCV-seropositive livers can now be safely transplanted into HCV-seronegative patients with minimal post-transplant complications due to availability of safe and effective DAA therapies [24,25]. High BMI and h/o heavy alcohol use are risk factors for steatosis [3,22] and these characteristics still tend to promote organ declines (Table 5). Compared to kidney offers, the impact of initial offer on liver acceptance was small (Tables 6, 7). In addition, the weekend effect was not seen as an independent risk factor leading to decline of adult liver offers for transplant because macrosteatosis >30% and fibrosis in the liver were stronger independent risk factors. Like kidneys, perfusion-based preservation use was a factor predictive of reduced liver declines for transplant. Since normothermic machine perfusion pumps were only recently approved by the FDA, it is expected that utilization of currently discarded livers will almost certainly increase in the future.
PEDIATRIC DONOR LIVERS:
Poor donor liver quality (terminal ALT >500, T-bil >10), smaller donors (age <6 years, height <100 cm), and HBVc-Ab-positive donors are independent risk factors correlated with decline of the initial offer. Prior studies demonstrated that the most significant risk factors for discard of pediatric livers were DCD, terminal ALT >500, and T-bil >10 [26]. In addition, HBVc-Ab-positive and donor weight and height were also risk factors for pediatric liver discard [26]. Based on these data, if pediatric donors have those factors, increasing decline of the initial offer leads to discard of livers. In addition to these declines of initial offers, macrosteatosis >30% of pediatric livers was also associated with the final decline of livers for transplant.
Although there are many strengths of this study, we acknowledge several limitations that are inherent in observational studies analyzing registry data. First, we were not able to analyze time of day, which meant we could not define, for example, from Friday at 6 pm to Monday at 6 am as the weekend, even though this way may more accurately reflect the weekend. Second, we were unable to evaluate recipient OPO/center effects or individual recipient factors (eg, patients’ availability, MELD/PELD score). Third, due to the large size of the database, some observed differences may reach statistical significance despite being clinically insignificant.
Conclusions
Even though allocation systems are continually being modified to promote greater organ utilization, and the availability of kidneys and livers have increased significantly in the USA over the past 5 years, the weekend effect has a significant impact on adult liver and kidney offer acceptances. Interestingly, the weekend effect was not evident for pediatric liver and kidney offers; likely a consequence of the different nature of adult and pediatric practice, the higher quality of pediatric organs, and the relative infrequency of offers compared to those for adult recipients. Manpower differences on the weekend may contribute to the offer decline imbalance. A number of solutions have been proposed to address this wastage of potentially life-saving organs, including penalizing centers for low transplant rates or low organ acceptance rates, or by increased funding to centers to address resource shortages. None of these appear practical or very likely to succeed. As noted above, introduction of better assessment tools such as organ perfusion could have a major positive impact. In addition, to address this issue, strategies should be devised to better synchronize manpower and organ availability, avoiding weekend offers in areas of poor utilization on the weekend. In the centers too, organ preservation may be impactful by facilitating delay in transplantation until times when centers are better resourced and staffed to handle more organs.
Figures
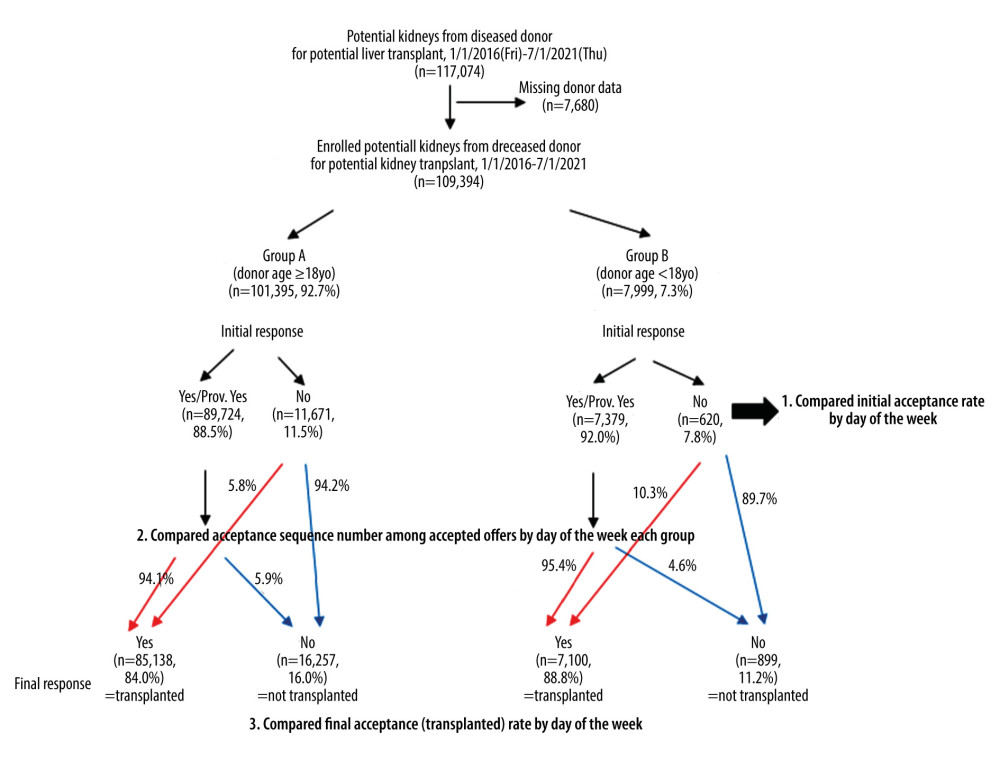 Figure 1. Schematic illustration of our cohort study of potential kidneys from deceased donors from 1/1/2016 to 7/1/2021. In the Group A (adult cases), 94.1% of initial offer acceptances accepted the kidney for transplant but 5.9% did not. On the other hand, 94.2% of initial offer declines declined the kidney for transplant, but 5.8% did not. In the Group B (pediatric cases), 95.4% of initial offer acceptances accepted the kidney for transplant, but 4.6% did not. On the other hand, 89.7% of initial offer declines declined the kidney for transplant, but 10.3% did not. Created using Microsoft® PowerPoint® for Microsoft 365 MSO (Version 2202 Build 16.0.14931.20602) 32-bit.
Figure 1. Schematic illustration of our cohort study of potential kidneys from deceased donors from 1/1/2016 to 7/1/2021. In the Group A (adult cases), 94.1% of initial offer acceptances accepted the kidney for transplant but 5.9% did not. On the other hand, 94.2% of initial offer declines declined the kidney for transplant, but 5.8% did not. In the Group B (pediatric cases), 95.4% of initial offer acceptances accepted the kidney for transplant, but 4.6% did not. On the other hand, 89.7% of initial offer declines declined the kidney for transplant, but 10.3% did not. Created using Microsoft® PowerPoint® for Microsoft 365 MSO (Version 2202 Build 16.0.14931.20602) 32-bit. 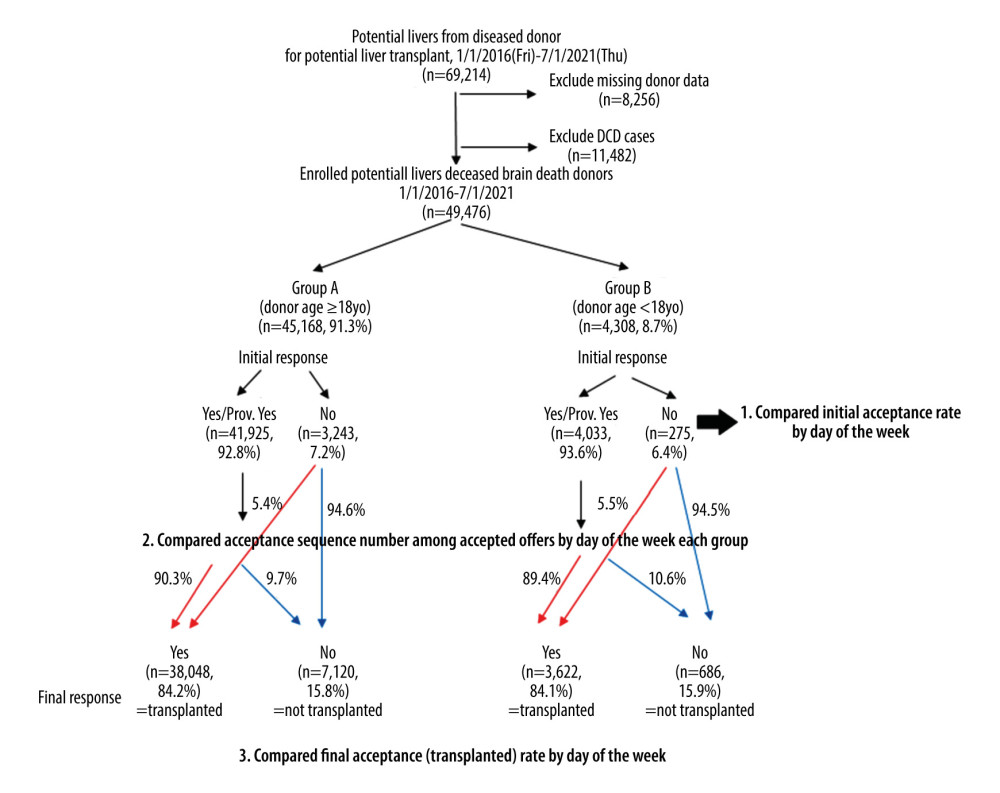 Figure 2. Schematic illustration for our cohort study of potential livers from deceased donors from 1/1/2016 to 7/1/2021. In the Group A (adult cases), 90.3% of initial offer acceptances accepted the liver for transplant but 9.7% did not. On the other hand, 94.6% of initial offer declines declined the liver for transplant, but 5.4% did not. In the Group B (pediatric cases), 89.4% of initial offer acceptances accepted the liver for transplant but 10.6% did not. On the other hand, 94.5% of initial offer declines declined the liver for transplant, but 5.5% did not. Created using Microsoft® PowerPoint® for Microsoft 365 MSO (Version 2202 Build 16.0.14931.20602) 32-bit.
Figure 2. Schematic illustration for our cohort study of potential livers from deceased donors from 1/1/2016 to 7/1/2021. In the Group A (adult cases), 90.3% of initial offer acceptances accepted the liver for transplant but 9.7% did not. On the other hand, 94.6% of initial offer declines declined the liver for transplant, but 5.4% did not. In the Group B (pediatric cases), 89.4% of initial offer acceptances accepted the liver for transplant but 10.6% did not. On the other hand, 94.5% of initial offer declines declined the liver for transplant, but 5.5% did not. Created using Microsoft® PowerPoint® for Microsoft 365 MSO (Version 2202 Build 16.0.14931.20602) 32-bit. 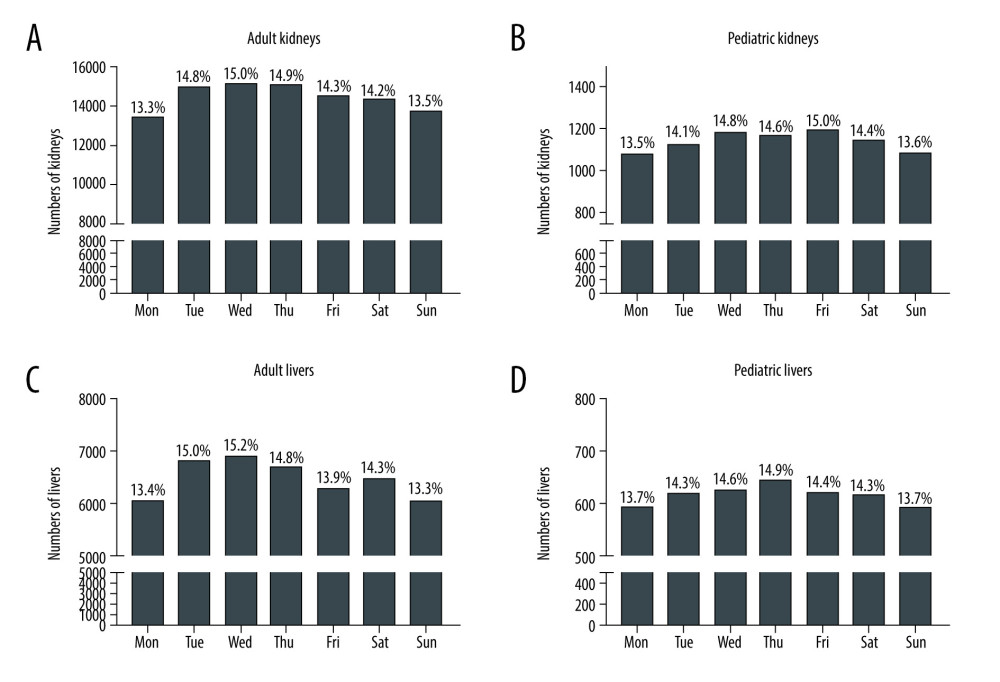 Figure 3. Total number of initial offers of adult kidneys (A), pediatric kidneys (B), adult livers (C), and pediatric livers (D) over the course of the week from 1/1/2016 to 7/1/2021. Each percentage on the day shows the percentage among total cases. Made by Microsoft® PowerPoint® for Microsoft 365 MSO (Version 2202 Build 16.0.14931.20602) 32-bit and social sciences software GraphPad Prism 9 (GraphPad Software, San Diego, CA).
Figure 3. Total number of initial offers of adult kidneys (A), pediatric kidneys (B), adult livers (C), and pediatric livers (D) over the course of the week from 1/1/2016 to 7/1/2021. Each percentage on the day shows the percentage among total cases. Made by Microsoft® PowerPoint® for Microsoft 365 MSO (Version 2202 Build 16.0.14931.20602) 32-bit and social sciences software GraphPad Prism 9 (GraphPad Software, San Diego, CA). 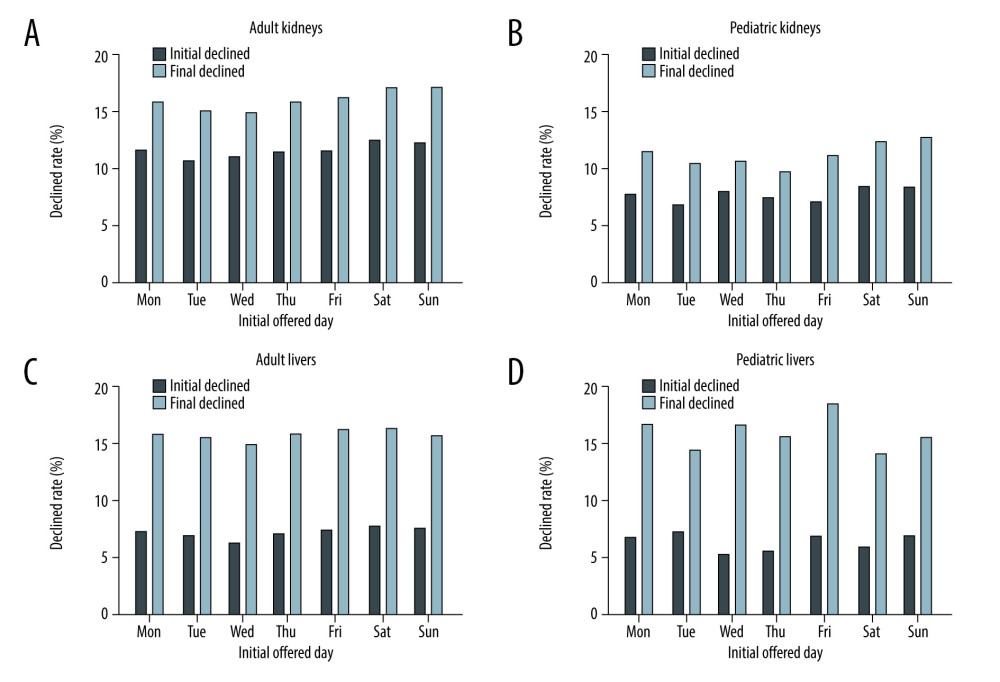 Figure 4. Rate of declined to initial and final offers of adult kidneys (A), pediatric kidneys (B), adult livers (C), and pediatric livers (D) over the course of the week from 1/1/2016 to 7/1/2021. Black bars show each rate of declined to initial offers and light bars show each rate of declined to final offers. Created using Microsoft® PowerPoint® for Microsoft 365 MSO (Version 2202 Build 16.0.14931.20602) 32-bit and social sciences software GraphPad Prism 9 (GraphPad Software, San Diego, CA).
Figure 4. Rate of declined to initial and final offers of adult kidneys (A), pediatric kidneys (B), adult livers (C), and pediatric livers (D) over the course of the week from 1/1/2016 to 7/1/2021. Black bars show each rate of declined to initial offers and light bars show each rate of declined to final offers. Created using Microsoft® PowerPoint® for Microsoft 365 MSO (Version 2202 Build 16.0.14931.20602) 32-bit and social sciences software GraphPad Prism 9 (GraphPad Software, San Diego, CA). Tables
Table 1. Characteristics of potential deceased kidney donors for the initial offers (accept kidneys vs decline kidneys).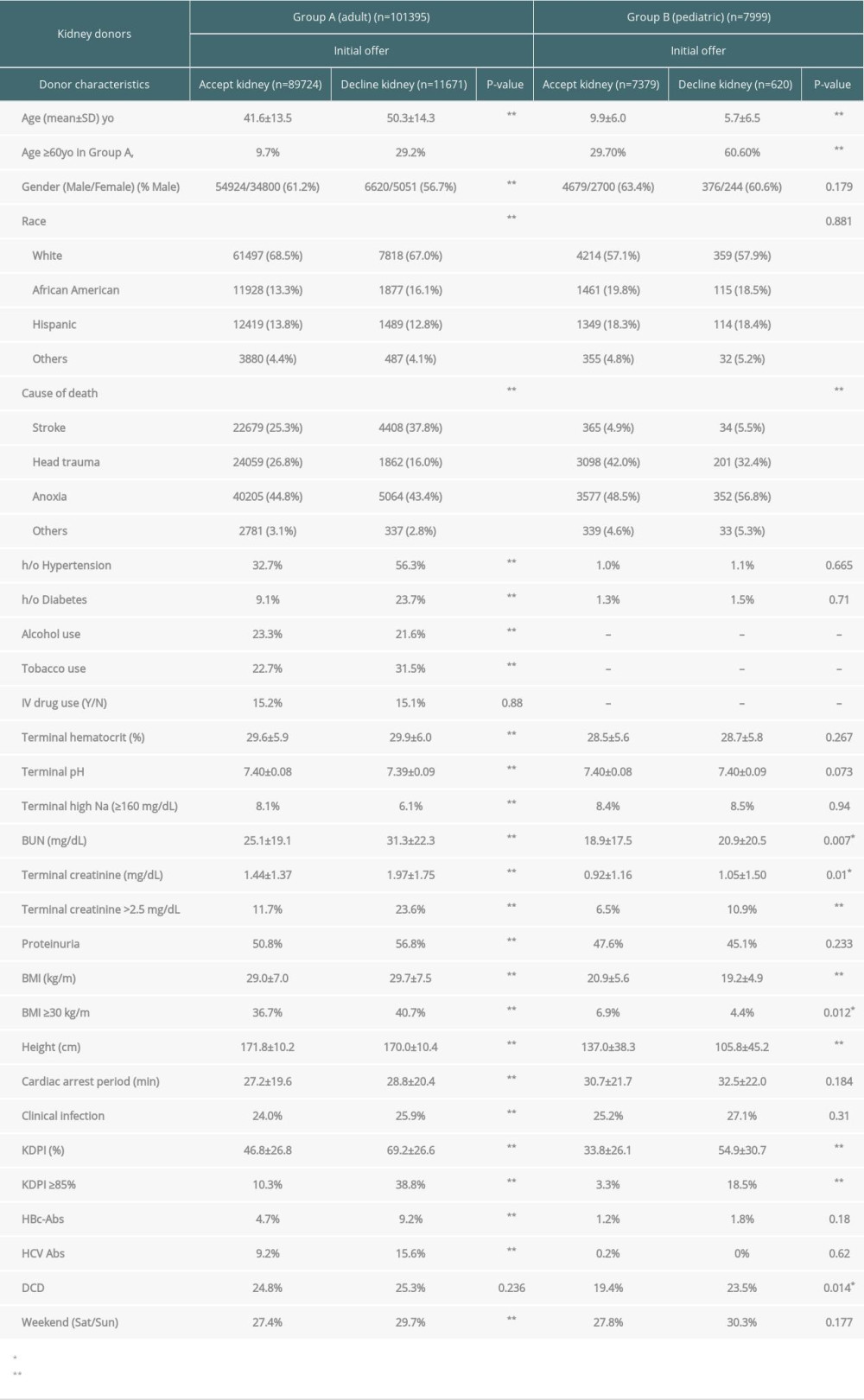 Table 2. Characteristics of potential deceased liver donors for the initial offers (accept liver vs decline liver).
Table 2. Characteristics of potential deceased liver donors for the initial offers (accept liver vs decline liver).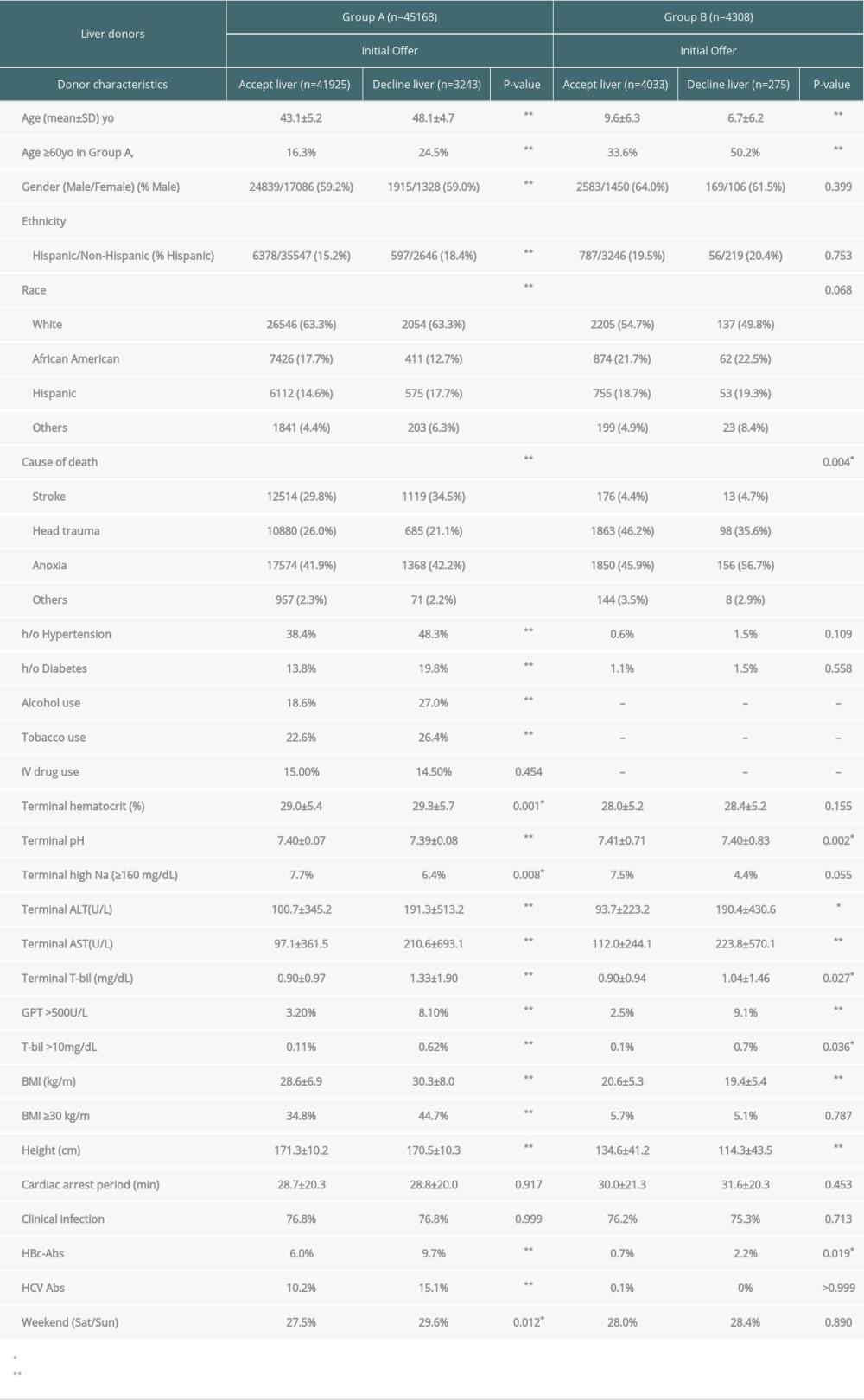 Table 3. Weekday vs weekend of initial declined rate, mean sequence number and final declined rate.
Table 3. Weekday vs weekend of initial declined rate, mean sequence number and final declined rate.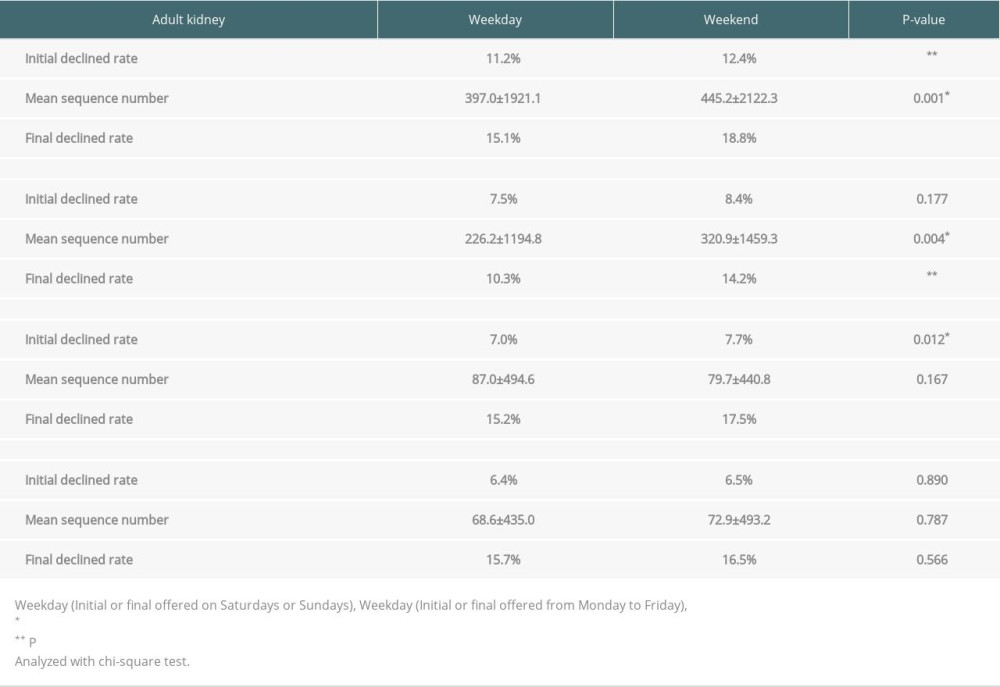 Table 4. Logistic regression for risk factors of declined to the initial offers in adult deceased kidneys.
Table 4. Logistic regression for risk factors of declined to the initial offers in adult deceased kidneys.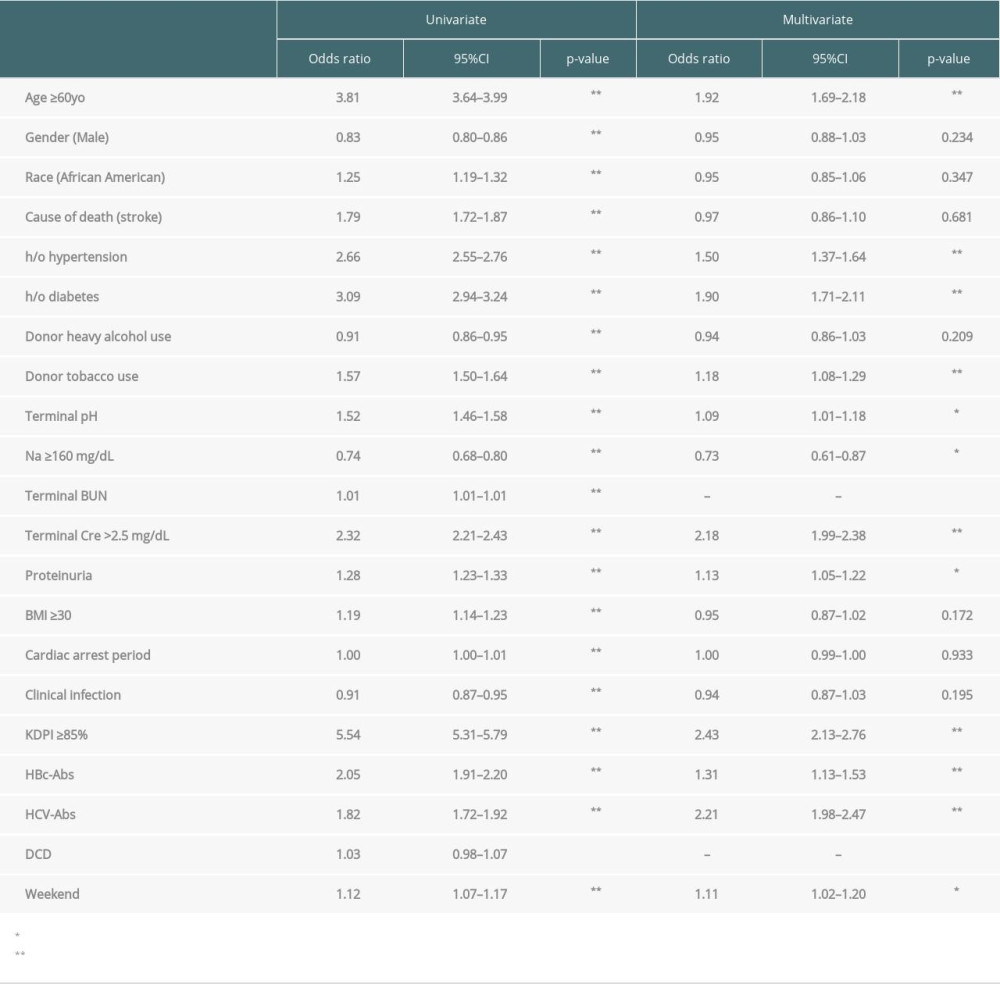 Table 5. Logistic regression for risk factors of declined to the initial offers in pediatric deceased kidneys.
Table 5. Logistic regression for risk factors of declined to the initial offers in pediatric deceased kidneys.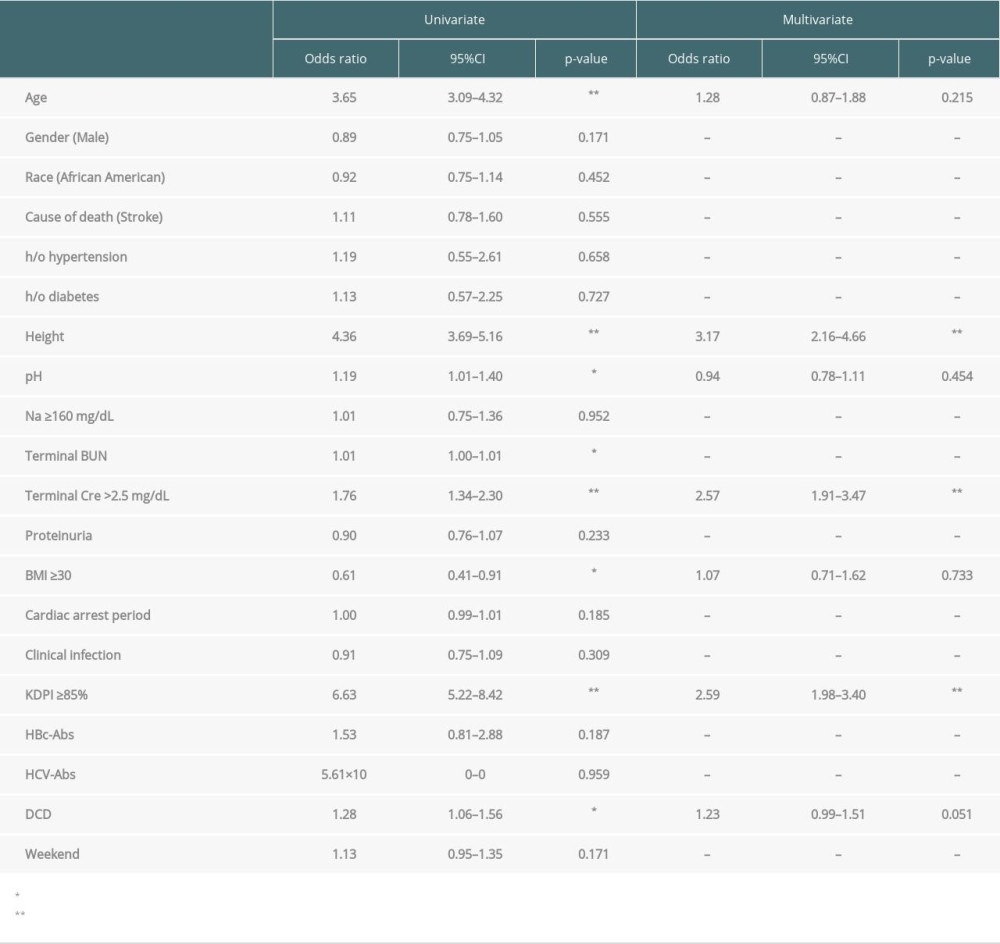 Table 6. Logistic regression for risk factors of declined to the initial offers in adult deceased livers.
Table 6. Logistic regression for risk factors of declined to the initial offers in adult deceased livers. Table 7. Logistic regression for risk factors of declined to the initial offers in pediatric deceased livers.
Table 7. Logistic regression for risk factors of declined to the initial offers in pediatric deceased livers. Table 8. Logistic regression for risk factors of declined to the final offers in (A) adult or (B) pediatric deceased kidneys.
Table 8. Logistic regression for risk factors of declined to the final offers in (A) adult or (B) pediatric deceased kidneys.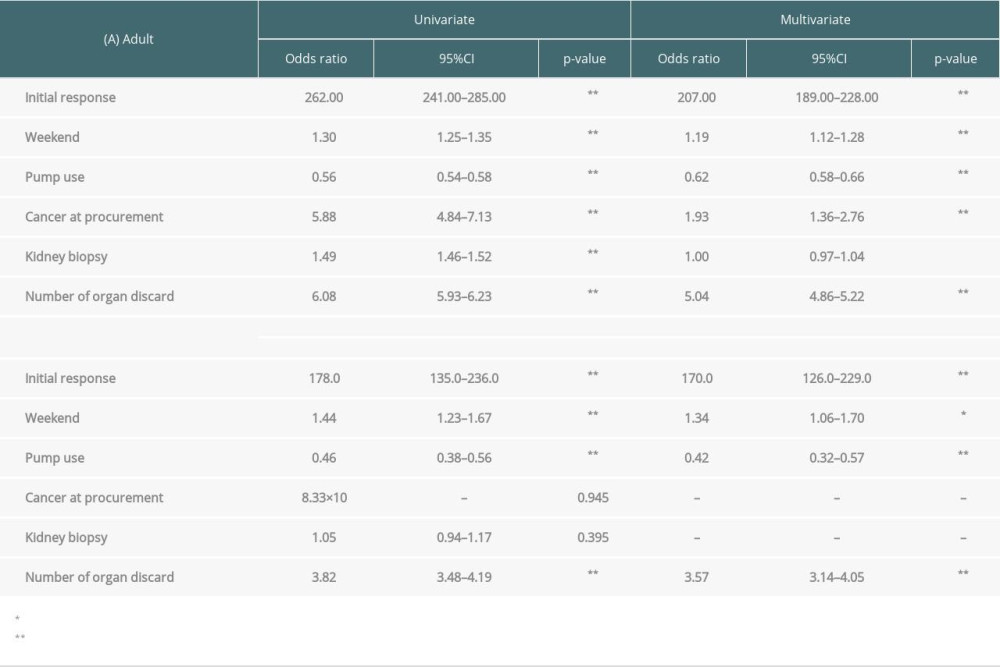 Table 9. Logistic regression for risk factors of declined to the final offers in (A) adult or (B) pediatric deceased livers.
Table 9. Logistic regression for risk factors of declined to the final offers in (A) adult or (B) pediatric deceased livers.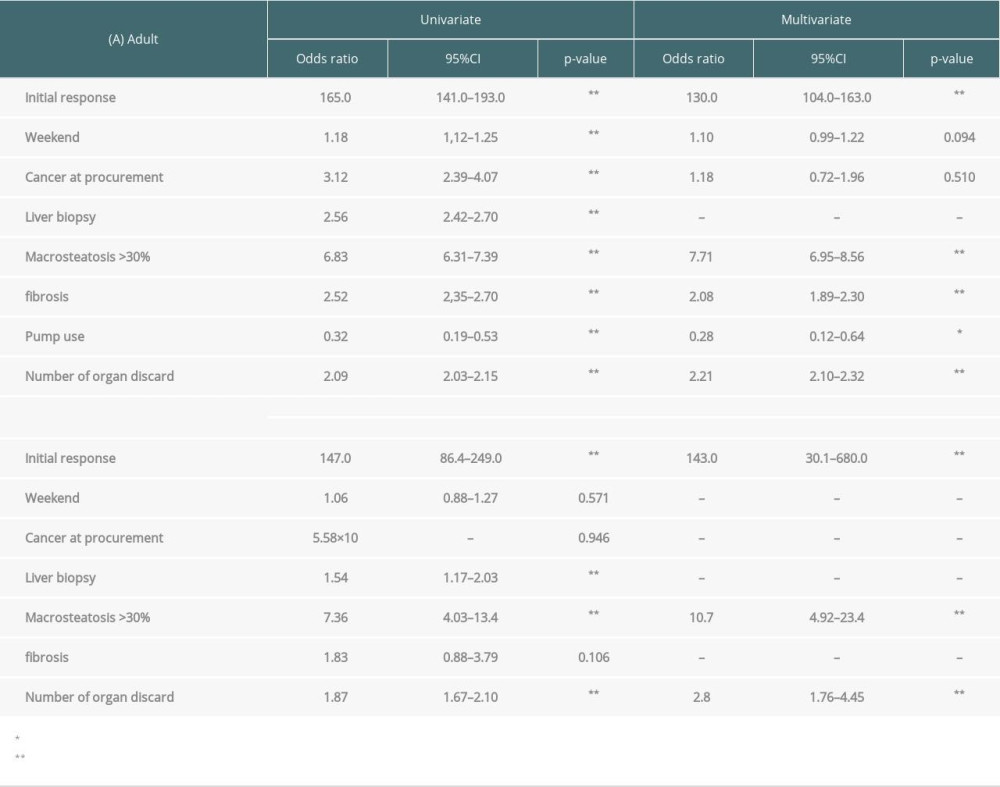 Supplementary Table 1. Total numbers, initial and final offers of potential kidneys from deceased donors by day of week (A. adult donors, B. pediatric donors).
Supplementary Table 1. Total numbers, initial and final offers of potential kidneys from deceased donors by day of week (A. adult donors, B. pediatric donors).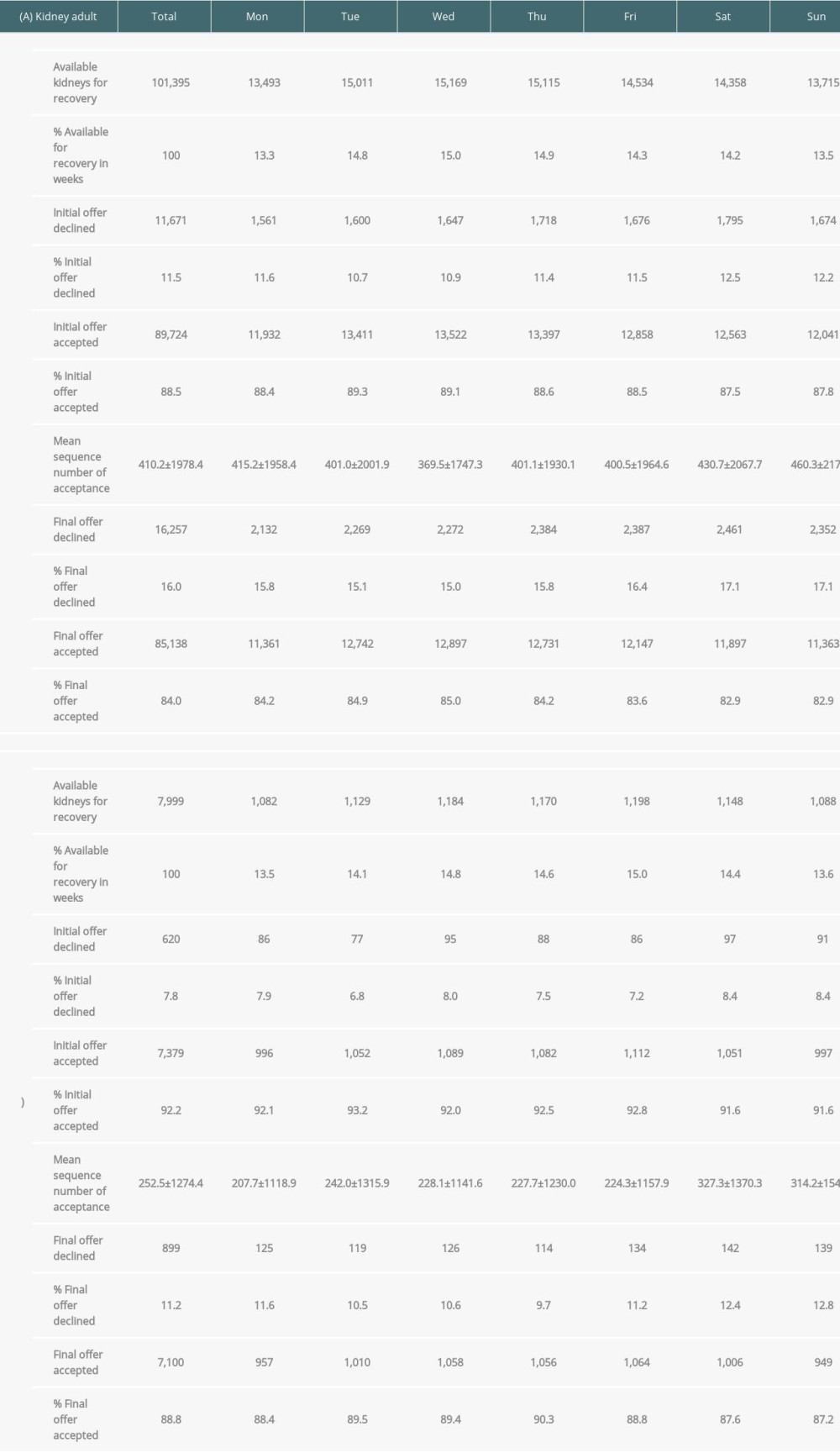 Supplementary Table 2. Total numbers, initial offer and final offers of potential livers from deceased donors by day of week (A. adult donors, B. pediatric donors).
Supplementary Table 2. Total numbers, initial offer and final offers of potential livers from deceased donors by day of week (A. adult donors, B. pediatric donors).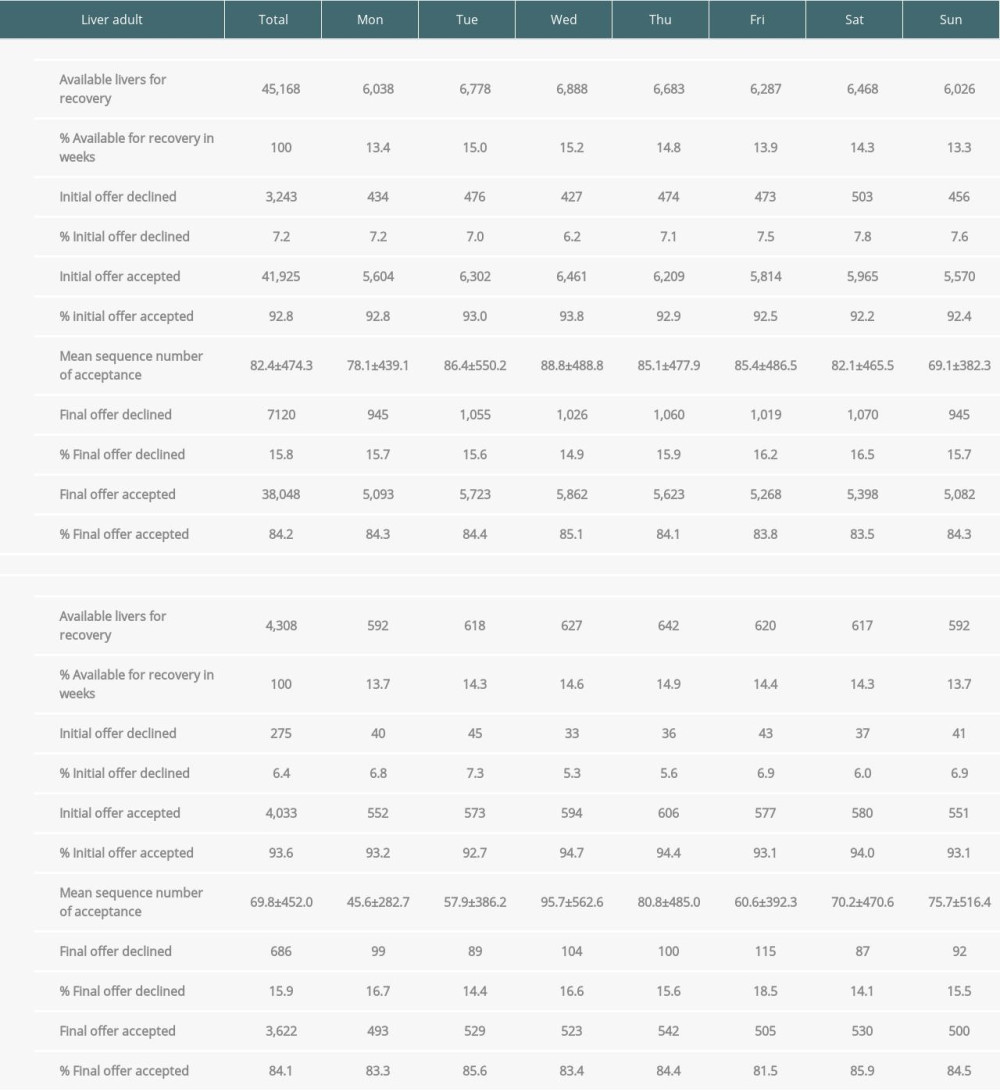 Supplementary Table 3. Adult donors vs pediatric donors of initial and final declined rate (A. Kidney, B. Liver).
Supplementary Table 3. Adult donors vs pediatric donors of initial and final declined rate (A. Kidney, B. Liver).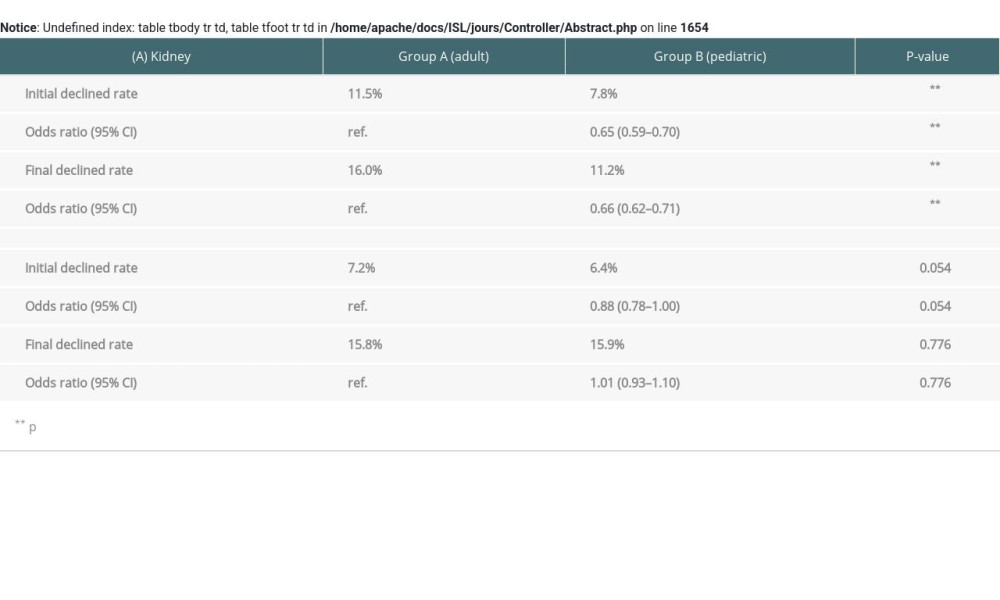
References
1. Mohan S, Foley K, Chiles MC, The weekend effect alters the procurement and discard rates of deceased donor kidneys in the United States: Kidney Int, 2016; 90(1); 157-63
2. Cohen JB, Shults J, Goldberg DS, Kidney allograft offers: Predictors of turndown and the impact of late organ acceptance on allograft survival: Am J Transplant, 2018; 18(2); 391-401
3. Carpenter DJ, Chiles MC, Verna EC, Deceased brain dead donor liver transplantation and utilization in the United States: Nighttime and weekend effects: Transplantation, 2019; 103(7); 1392-404
4. King KL, Husain SA, Cohen DJ, Mohan S, Deceased donor kidneys are harder to place on the weekend: Clin J Am Soc Nephrol, 2019; 14(6); 904-6
5. Feng S, Goodrich NP, Bragg-Gresham JL, Characteristics associated with liver graft failure: The concept of a donor risk index: Am J Transplant, 2006; 6(4); 783-90
6. Becker F, Vogel T, Voss T, The weekend effect in liver transplantation: PLoS One, 2018; 13(5); e0198035
7. Baid-Agrawal S, Martus P, Feldman H, Kramer H, Weekend versus weekday transplant surgery and outcomes after kidney transplantation in the USA: A retrospective national database analysis: BMJ Open, 2016; 6(4); e010482
8. Bell CM, Redelmeier DA, Mortality among patients admitted to hospitals on weekends as compared with weekdays: N Engl J Med, 2001; 345(9); 663-68
9. Yu K, King K, Husain SA, Kidney nonprocurement in solid organ donors in the United States: Am J Transplant, 2020; 20(12); 3413-25
10. Stewart ZA, Shah SA, Formica RN, A call to action: Feasible strategies to reduce the discard of transplantable kidneys in the United States: Clin Transplant, 2020; 34(9); e13990
11. Reese PP, Harhay MN, Abt PL, New solutions to reduce discard of kidneys donated for transplantation: J Am Soc Nephrol, 2016; 27(4); 973-80
12. Jung CW, Jorgensen D, Sood P, Outcomes and factors leading to graft failure in kidney transplants from deceased donors with acute kidney injury – a retrospective cohort study: PLoS One, 2021; 16(8); e0254115
13. Pei J, Cho Y, See YP, Impact of deceased donor with acute kidney injury on subsequent kidney transplant outcomes – an ANZDATA registry analysis: PLoS One, 2021; 16(3); e0249000
14. Sonnenberg EM, Hsu JY, Cohen JB, Acute kidney injury in deceased organ donors and kidney transplant outcomes: A National Cohort Study using a novel data source: Ann Surg, 2020 [Online ahead of print]
15. Daloul R, Pesavento TE, Goldberg DS, Reese PP, A review of kidney transplantation from HCV-viremic donors into HCV-negative recipients: Kidney Int, 2021; 100(6); 1190-98
16. Ariyamuthu VK, Sandikci B, AbdulRahim N, Trends in utilization of deceased donor kidneys based on hepatitis C virus status and impact of public health service labeling on discard: Transpl Infect Dis, 2020; 22(1); e13204
17. Kayler LK, Magliocca J, Fujita S, Recovery factors affecting utilization of small pediatric donor kidneys: Am J Transplant, 2009; 9(1); 210-16
18. de Santis Feltran L, Genzani CP, Hamamoto F, Encouraging outcomes of using a small-donor single graft in pediatric kidney transplantation: Pediatr Nephrol, 2022; 37(5); 1137-47
19. Fananapazir G, Tse G, Di Geronimo R, Urologic complications after transplantation of 225 en bloc kidneys from small pediatric donors ≤20 kg: Incidence, management, and impact on graft survival: Am J Transplant, 2020; 20(8); 2126-32
20. Troppmann C, Santhanakrishnan C, Fananapazir G, Short- and long-term outcomes of kidney transplants from very small (≤15 kg) pediatric donors with acute kidney injury: Transplantation, 2021; 105(2); 430-35
21. Rogers ME, Egberg MD, Sylvester F, Outcomes of pediatric liver transplant are unaffected by the time or day of surgery: Pediatr Transplant, 2020; 24(8); e13826
22. Rana A, Sigireddi RR, Halazun KJ, Predicting liver allograft discard: The discard risk index: Transplantation, 2018; 102(9); 1520-29
23. Kaltenbach MG, Harhay MO, Abt PL, Goldberg DS, Trends in deceased donor liver enzymes prior to transplant: The impact on graft selection and outcomes: Am J Transplant, 2020; 20(1); 213-19
24. Sobotka LA, Mumtaz K, Wellner MR, Outcomes of hepatitis C virus seropositive donors to hepatitis C virus seronegative liver recipients: A large single center analysis: Ann Hepatol, 2021; 24; 100318
25. Luckett K, Kaiser TE, Bari K, Use of hepatitis C virus antibody-positive donor livers in hepatitis C nonviremic liver transplant recipients: J Am Coll Surg, 2019; 228(4); 560-67
26. Malik T, Joshi M, Godfrey E, Pediatric discard risk index for predicting pediatric liver allograft discard: Pediatr Transplant, 2021; 25(5); e13963
Figures
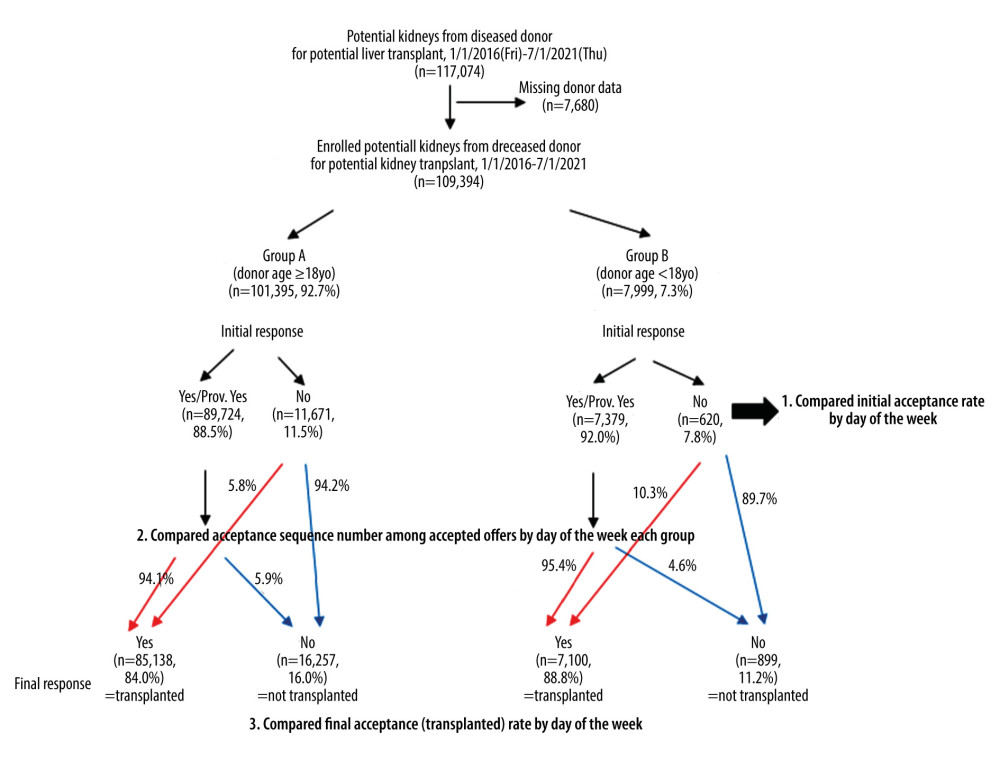 Figure 1. Schematic illustration of our cohort study of potential kidneys from deceased donors from 1/1/2016 to 7/1/2021. In the Group A (adult cases), 94.1% of initial offer acceptances accepted the kidney for transplant but 5.9% did not. On the other hand, 94.2% of initial offer declines declined the kidney for transplant, but 5.8% did not. In the Group B (pediatric cases), 95.4% of initial offer acceptances accepted the kidney for transplant, but 4.6% did not. On the other hand, 89.7% of initial offer declines declined the kidney for transplant, but 10.3% did not. Created using Microsoft® PowerPoint® for Microsoft 365 MSO (Version 2202 Build 16.0.14931.20602) 32-bit.
Figure 1. Schematic illustration of our cohort study of potential kidneys from deceased donors from 1/1/2016 to 7/1/2021. In the Group A (adult cases), 94.1% of initial offer acceptances accepted the kidney for transplant but 5.9% did not. On the other hand, 94.2% of initial offer declines declined the kidney for transplant, but 5.8% did not. In the Group B (pediatric cases), 95.4% of initial offer acceptances accepted the kidney for transplant, but 4.6% did not. On the other hand, 89.7% of initial offer declines declined the kidney for transplant, but 10.3% did not. Created using Microsoft® PowerPoint® for Microsoft 365 MSO (Version 2202 Build 16.0.14931.20602) 32-bit.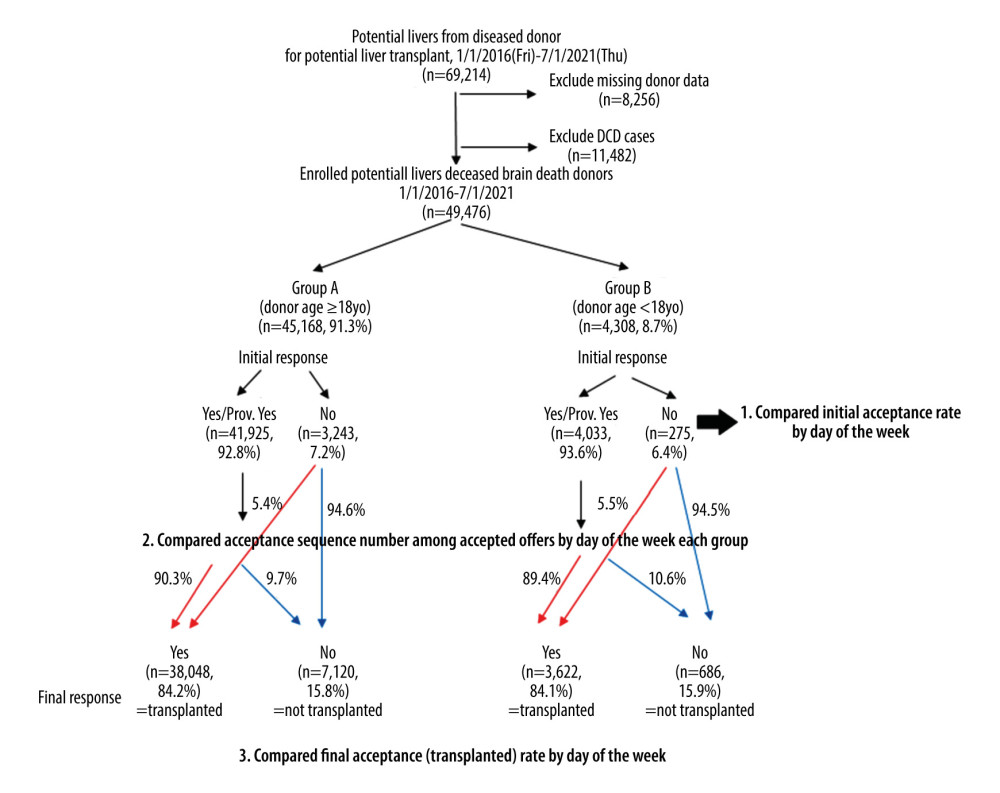 Figure 2. Schematic illustration for our cohort study of potential livers from deceased donors from 1/1/2016 to 7/1/2021. In the Group A (adult cases), 90.3% of initial offer acceptances accepted the liver for transplant but 9.7% did not. On the other hand, 94.6% of initial offer declines declined the liver for transplant, but 5.4% did not. In the Group B (pediatric cases), 89.4% of initial offer acceptances accepted the liver for transplant but 10.6% did not. On the other hand, 94.5% of initial offer declines declined the liver for transplant, but 5.5% did not. Created using Microsoft® PowerPoint® for Microsoft 365 MSO (Version 2202 Build 16.0.14931.20602) 32-bit.
Figure 2. Schematic illustration for our cohort study of potential livers from deceased donors from 1/1/2016 to 7/1/2021. In the Group A (adult cases), 90.3% of initial offer acceptances accepted the liver for transplant but 9.7% did not. On the other hand, 94.6% of initial offer declines declined the liver for transplant, but 5.4% did not. In the Group B (pediatric cases), 89.4% of initial offer acceptances accepted the liver for transplant but 10.6% did not. On the other hand, 94.5% of initial offer declines declined the liver for transplant, but 5.5% did not. Created using Microsoft® PowerPoint® for Microsoft 365 MSO (Version 2202 Build 16.0.14931.20602) 32-bit.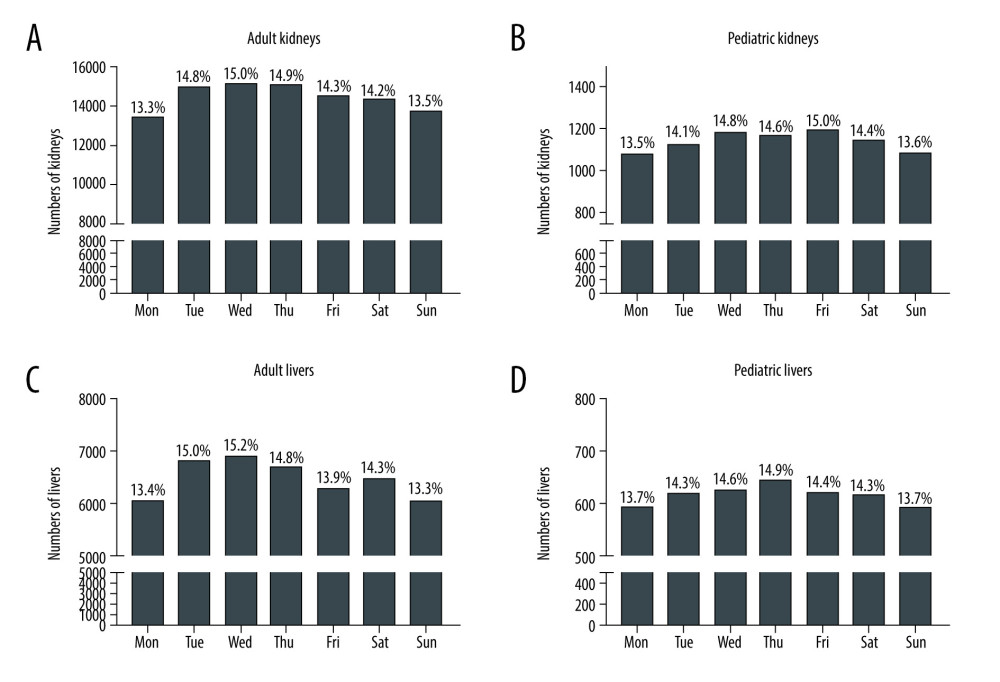 Figure 3. Total number of initial offers of adult kidneys (A), pediatric kidneys (B), adult livers (C), and pediatric livers (D) over the course of the week from 1/1/2016 to 7/1/2021. Each percentage on the day shows the percentage among total cases. Made by Microsoft® PowerPoint® for Microsoft 365 MSO (Version 2202 Build 16.0.14931.20602) 32-bit and social sciences software GraphPad Prism 9 (GraphPad Software, San Diego, CA).
Figure 3. Total number of initial offers of adult kidneys (A), pediatric kidneys (B), adult livers (C), and pediatric livers (D) over the course of the week from 1/1/2016 to 7/1/2021. Each percentage on the day shows the percentage among total cases. Made by Microsoft® PowerPoint® for Microsoft 365 MSO (Version 2202 Build 16.0.14931.20602) 32-bit and social sciences software GraphPad Prism 9 (GraphPad Software, San Diego, CA).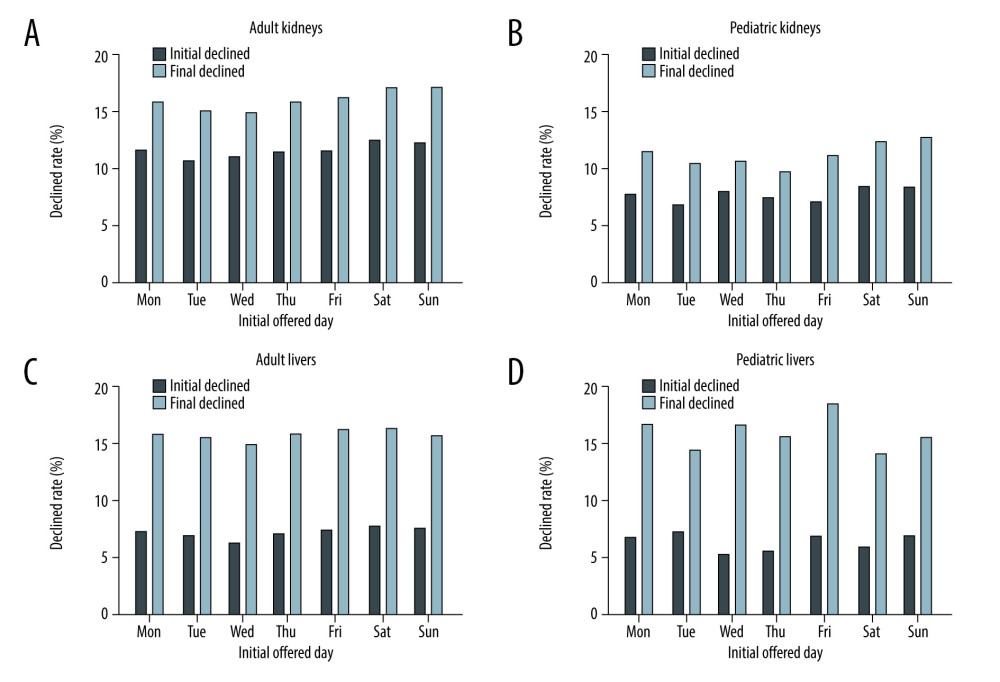 Figure 4. Rate of declined to initial and final offers of adult kidneys (A), pediatric kidneys (B), adult livers (C), and pediatric livers (D) over the course of the week from 1/1/2016 to 7/1/2021. Black bars show each rate of declined to initial offers and light bars show each rate of declined to final offers. Created using Microsoft® PowerPoint® for Microsoft 365 MSO (Version 2202 Build 16.0.14931.20602) 32-bit and social sciences software GraphPad Prism 9 (GraphPad Software, San Diego, CA).
Figure 4. Rate of declined to initial and final offers of adult kidneys (A), pediatric kidneys (B), adult livers (C), and pediatric livers (D) over the course of the week from 1/1/2016 to 7/1/2021. Black bars show each rate of declined to initial offers and light bars show each rate of declined to final offers. Created using Microsoft® PowerPoint® for Microsoft 365 MSO (Version 2202 Build 16.0.14931.20602) 32-bit and social sciences software GraphPad Prism 9 (GraphPad Software, San Diego, CA). Tables
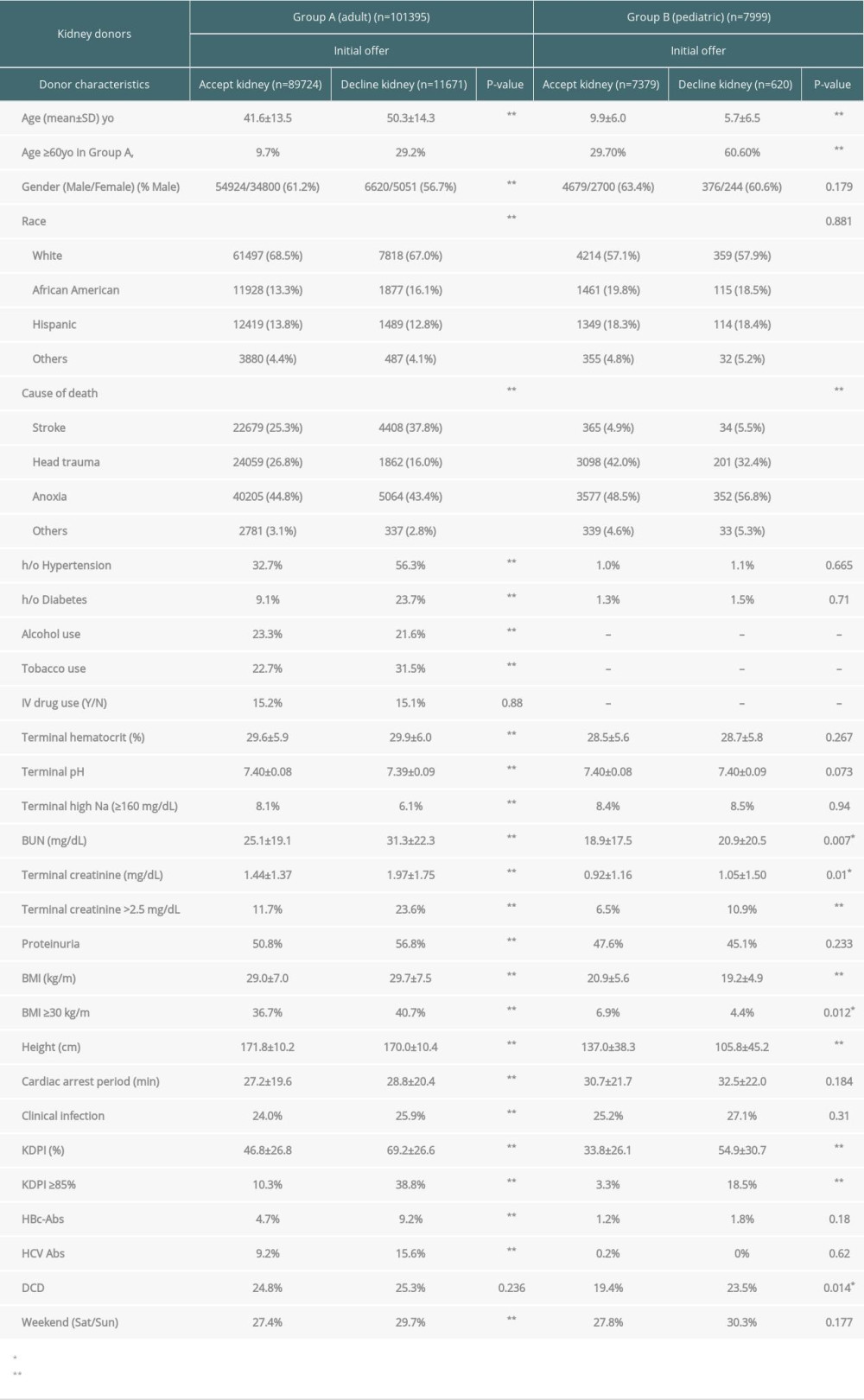 Table 1. Characteristics of potential deceased kidney donors for the initial offers (accept kidneys vs decline kidneys).
Table 1. Characteristics of potential deceased kidney donors for the initial offers (accept kidneys vs decline kidneys).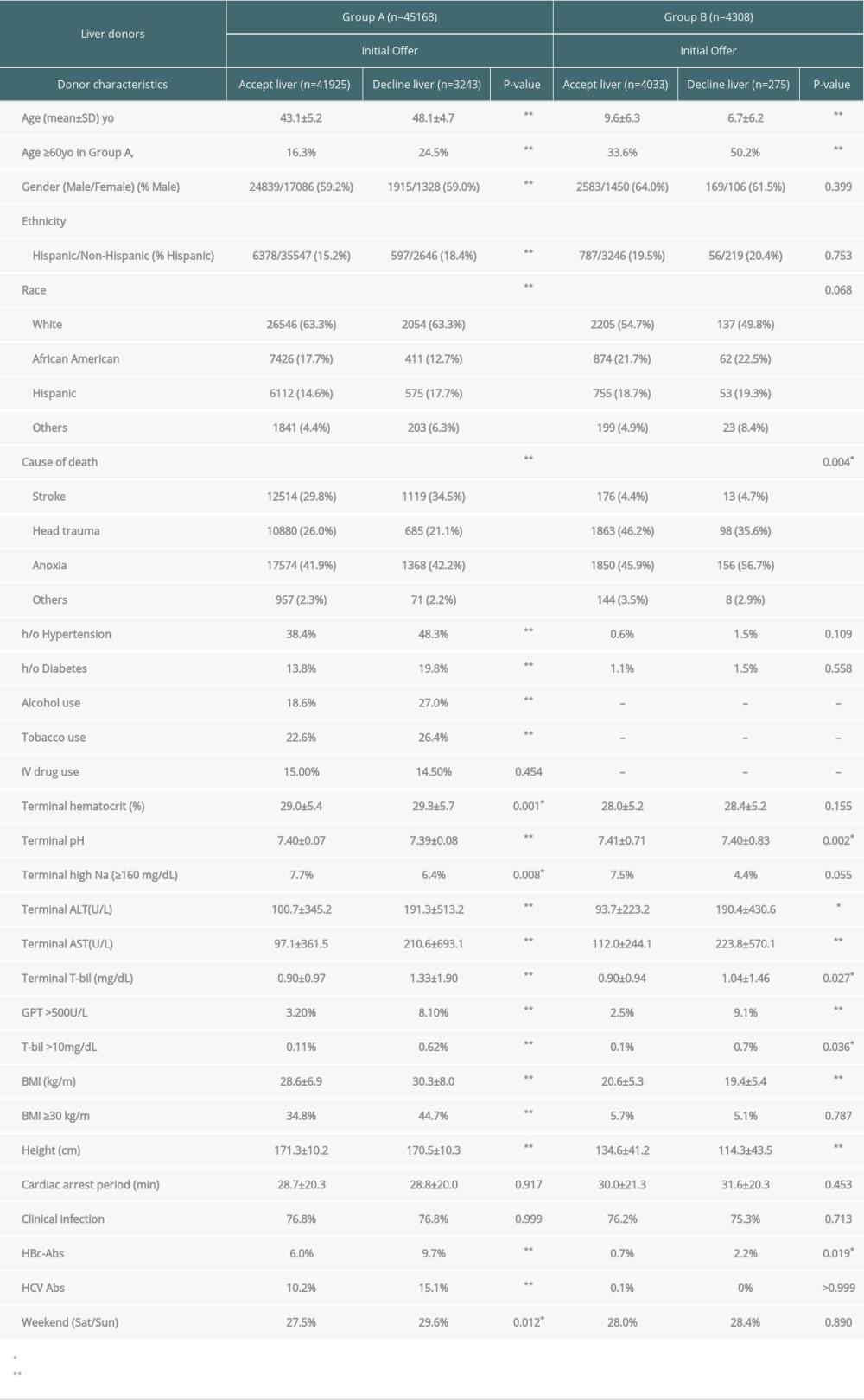 Table 2. Characteristics of potential deceased liver donors for the initial offers (accept liver vs decline liver).
Table 2. Characteristics of potential deceased liver donors for the initial offers (accept liver vs decline liver).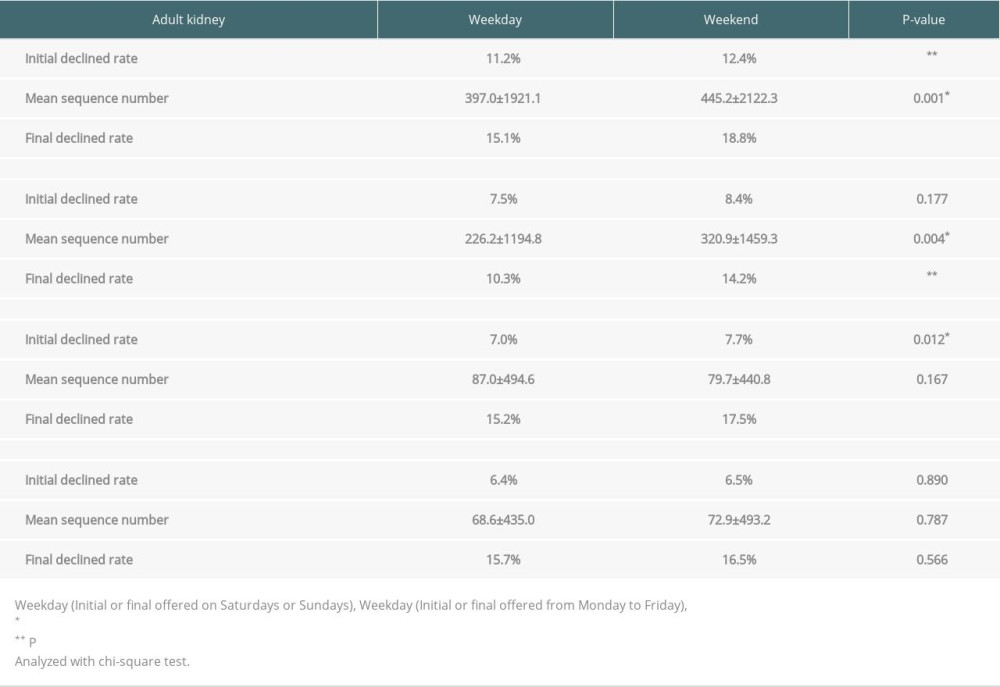 Table 3. Weekday vs weekend of initial declined rate, mean sequence number and final declined rate.
Table 3. Weekday vs weekend of initial declined rate, mean sequence number and final declined rate.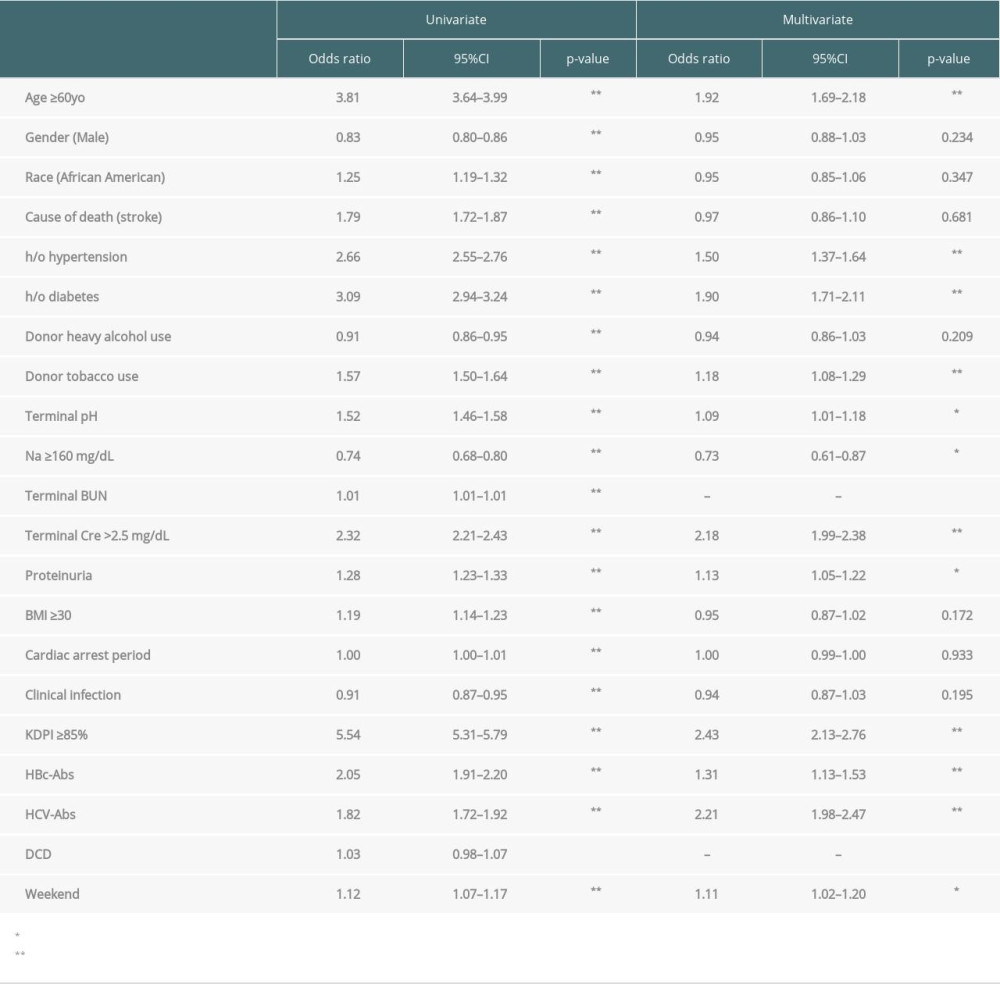 Table 4. Logistic regression for risk factors of declined to the initial offers in adult deceased kidneys.
Table 4. Logistic regression for risk factors of declined to the initial offers in adult deceased kidneys.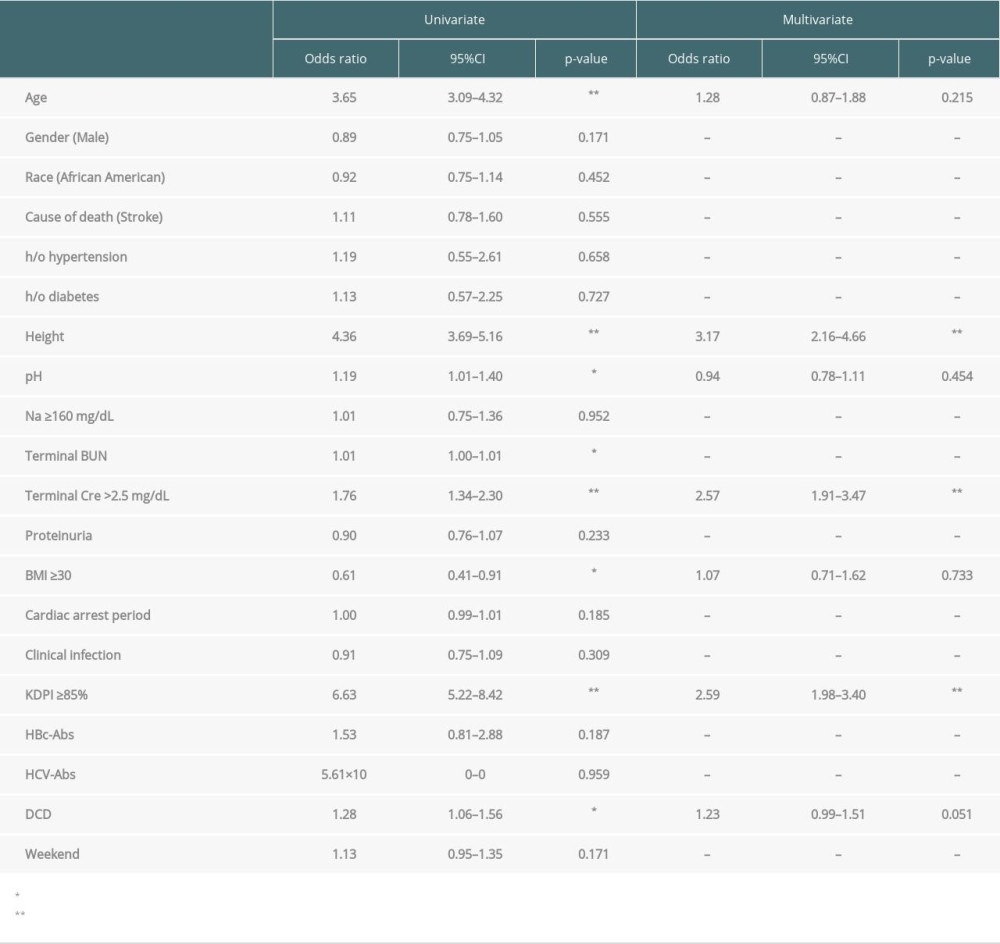 Table 5. Logistic regression for risk factors of declined to the initial offers in pediatric deceased kidneys.
Table 5. Logistic regression for risk factors of declined to the initial offers in pediatric deceased kidneys. Table 6. Logistic regression for risk factors of declined to the initial offers in adult deceased livers.
Table 6. Logistic regression for risk factors of declined to the initial offers in adult deceased livers. Table 7. Logistic regression for risk factors of declined to the initial offers in pediatric deceased livers.
Table 7. Logistic regression for risk factors of declined to the initial offers in pediatric deceased livers.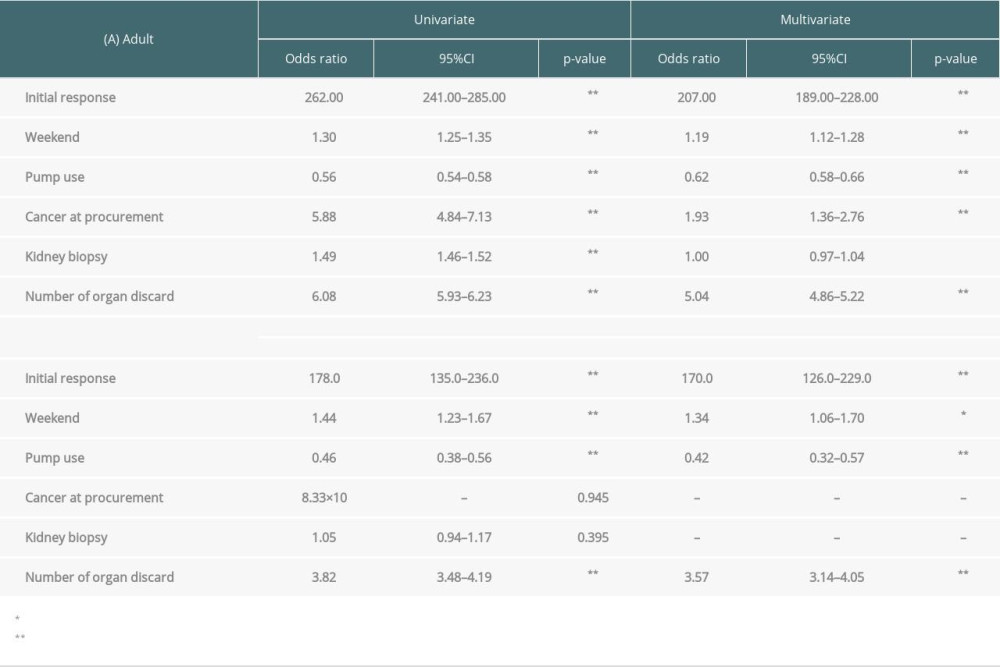 Table 8. Logistic regression for risk factors of declined to the final offers in (A) adult or (B) pediatric deceased kidneys.
Table 8. Logistic regression for risk factors of declined to the final offers in (A) adult or (B) pediatric deceased kidneys.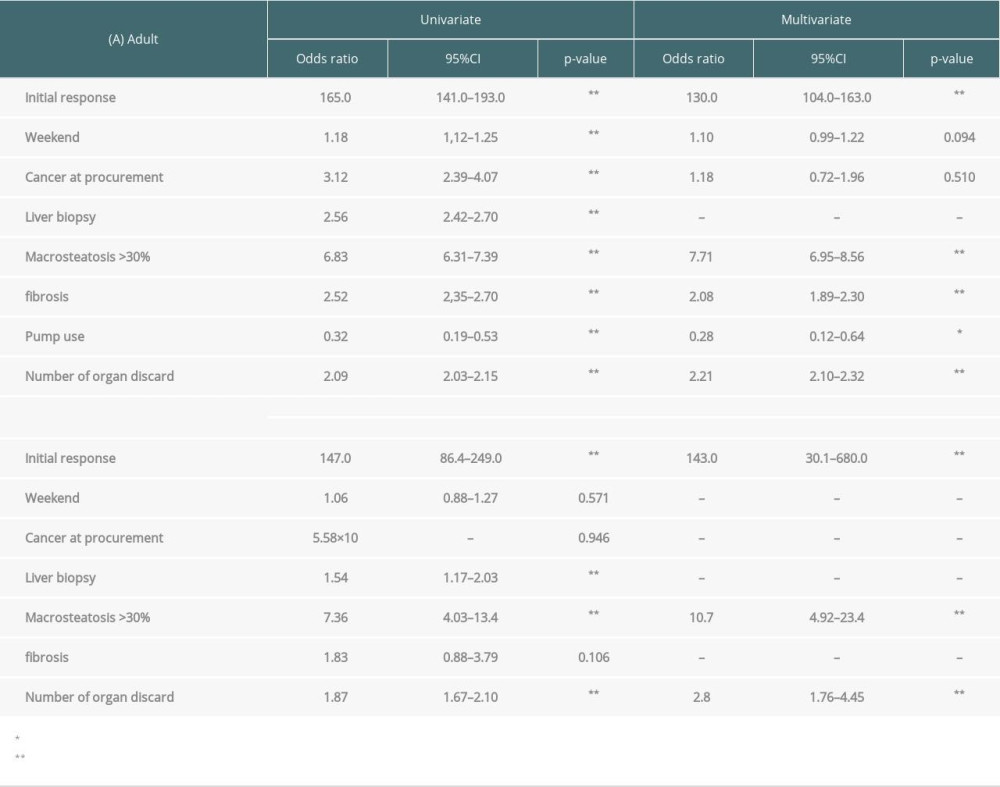 Table 9. Logistic regression for risk factors of declined to the final offers in (A) adult or (B) pediatric deceased livers.
Table 9. Logistic regression for risk factors of declined to the final offers in (A) adult or (B) pediatric deceased livers.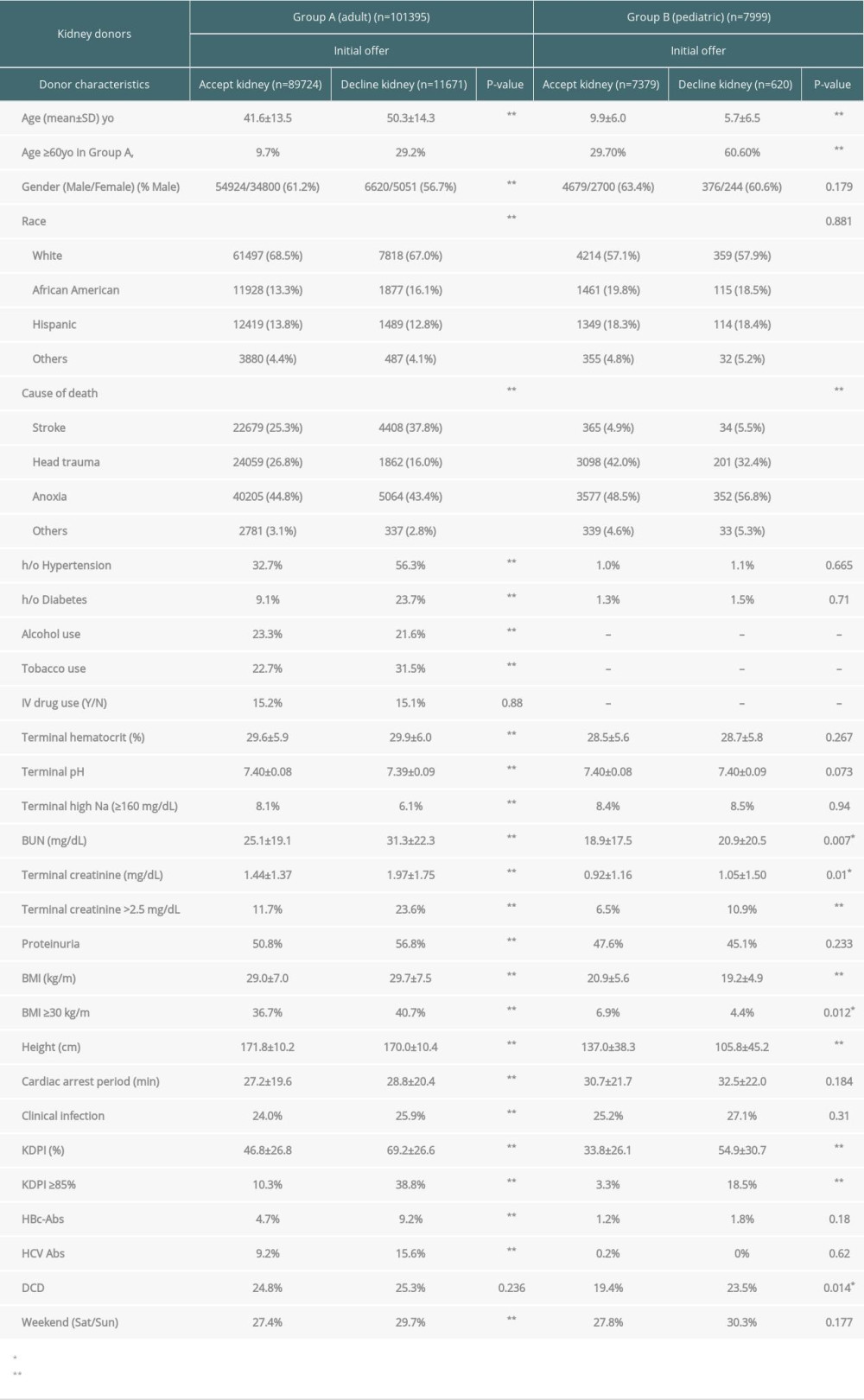 Table 1. Characteristics of potential deceased kidney donors for the initial offers (accept kidneys vs decline kidneys).
Table 1. Characteristics of potential deceased kidney donors for the initial offers (accept kidneys vs decline kidneys).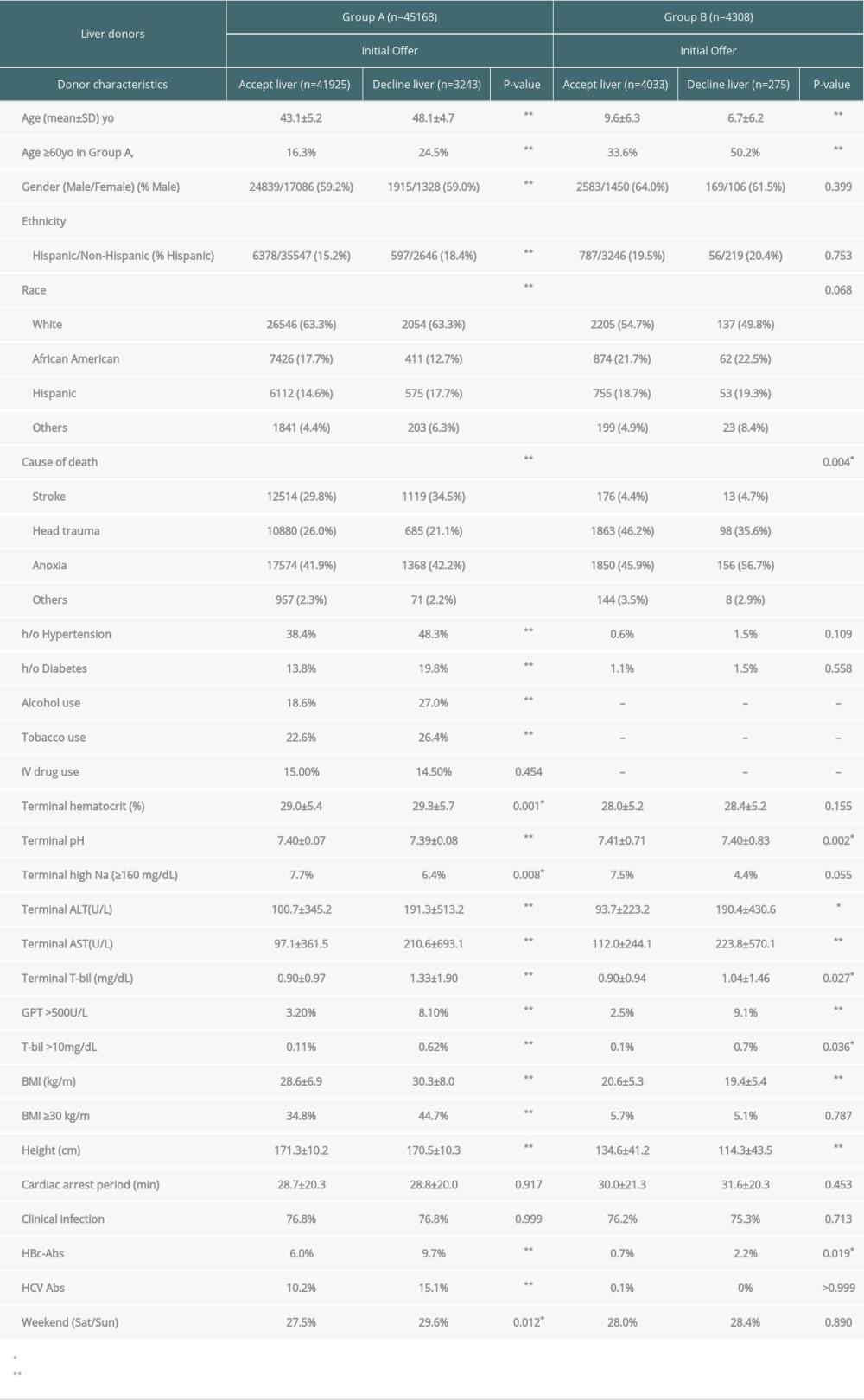 Table 2. Characteristics of potential deceased liver donors for the initial offers (accept liver vs decline liver).
Table 2. Characteristics of potential deceased liver donors for the initial offers (accept liver vs decline liver).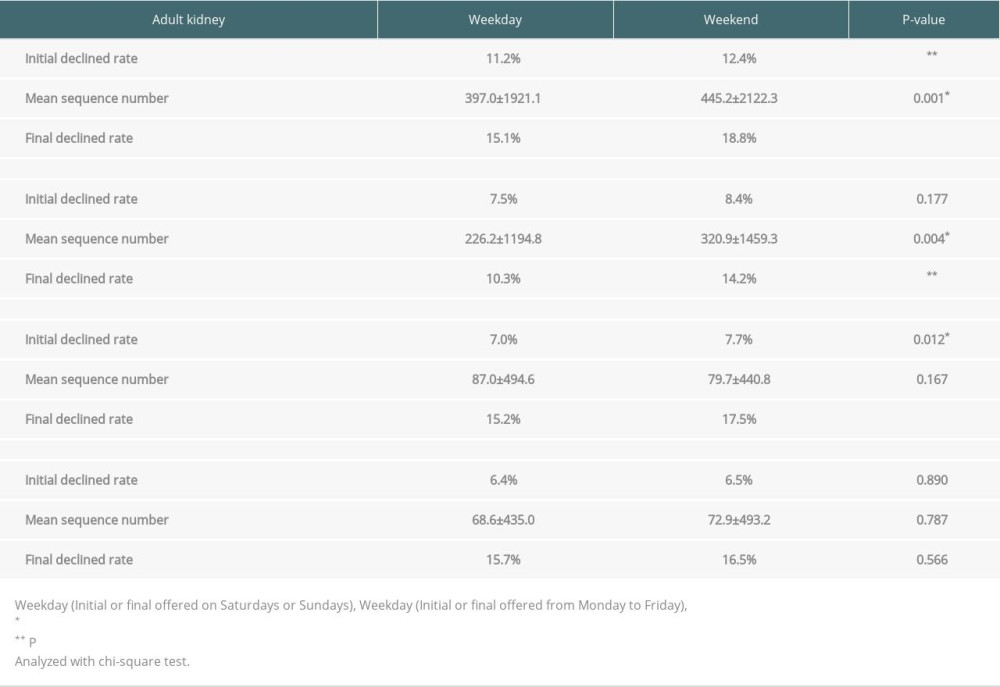 Table 3. Weekday vs weekend of initial declined rate, mean sequence number and final declined rate.
Table 3. Weekday vs weekend of initial declined rate, mean sequence number and final declined rate.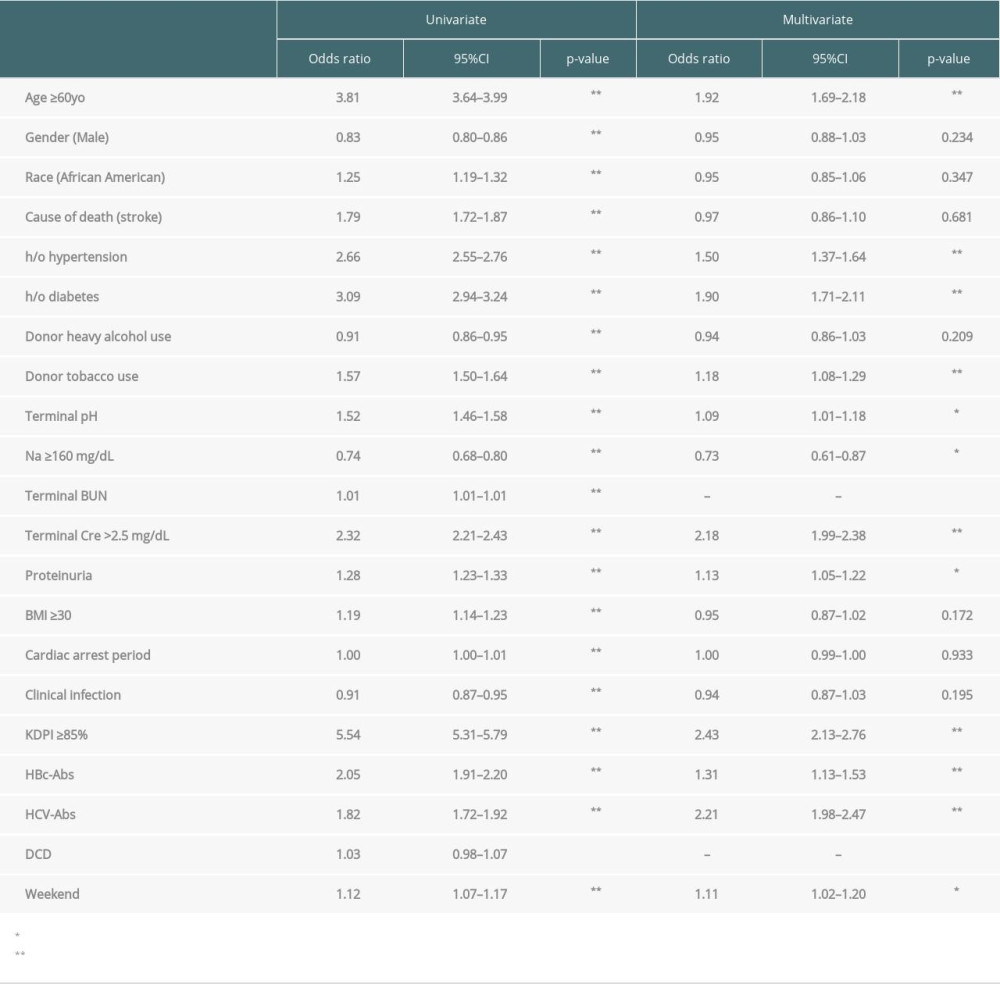 Table 4. Logistic regression for risk factors of declined to the initial offers in adult deceased kidneys.
Table 4. Logistic regression for risk factors of declined to the initial offers in adult deceased kidneys.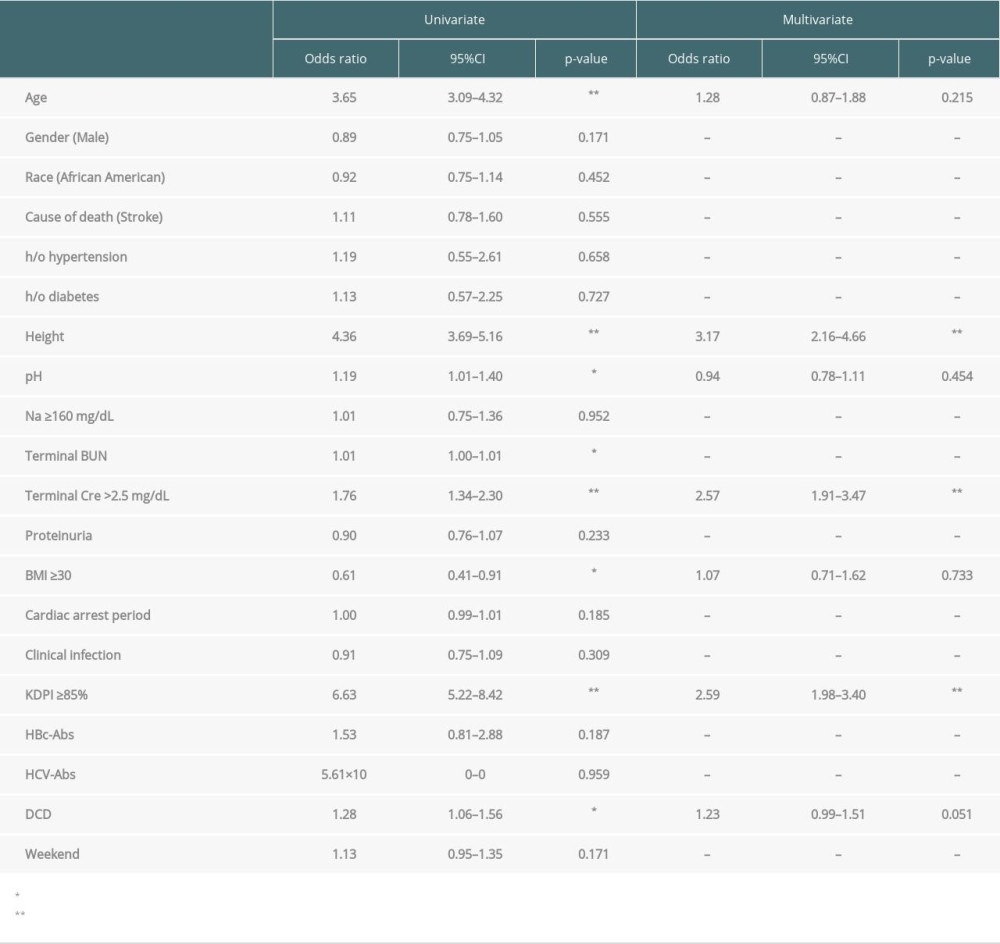 Table 5. Logistic regression for risk factors of declined to the initial offers in pediatric deceased kidneys.
Table 5. Logistic regression for risk factors of declined to the initial offers in pediatric deceased kidneys. Table 6. Logistic regression for risk factors of declined to the initial offers in adult deceased livers.
Table 6. Logistic regression for risk factors of declined to the initial offers in adult deceased livers. Table 7. Logistic regression for risk factors of declined to the initial offers in pediatric deceased livers.
Table 7. Logistic regression for risk factors of declined to the initial offers in pediatric deceased livers.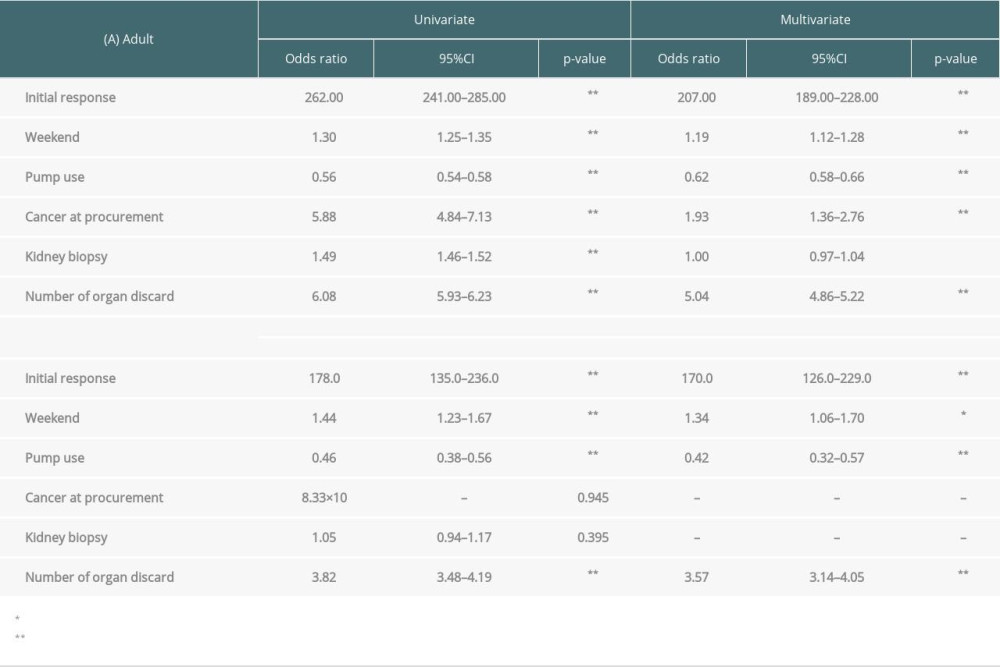 Table 8. Logistic regression for risk factors of declined to the final offers in (A) adult or (B) pediatric deceased kidneys.
Table 8. Logistic regression for risk factors of declined to the final offers in (A) adult or (B) pediatric deceased kidneys.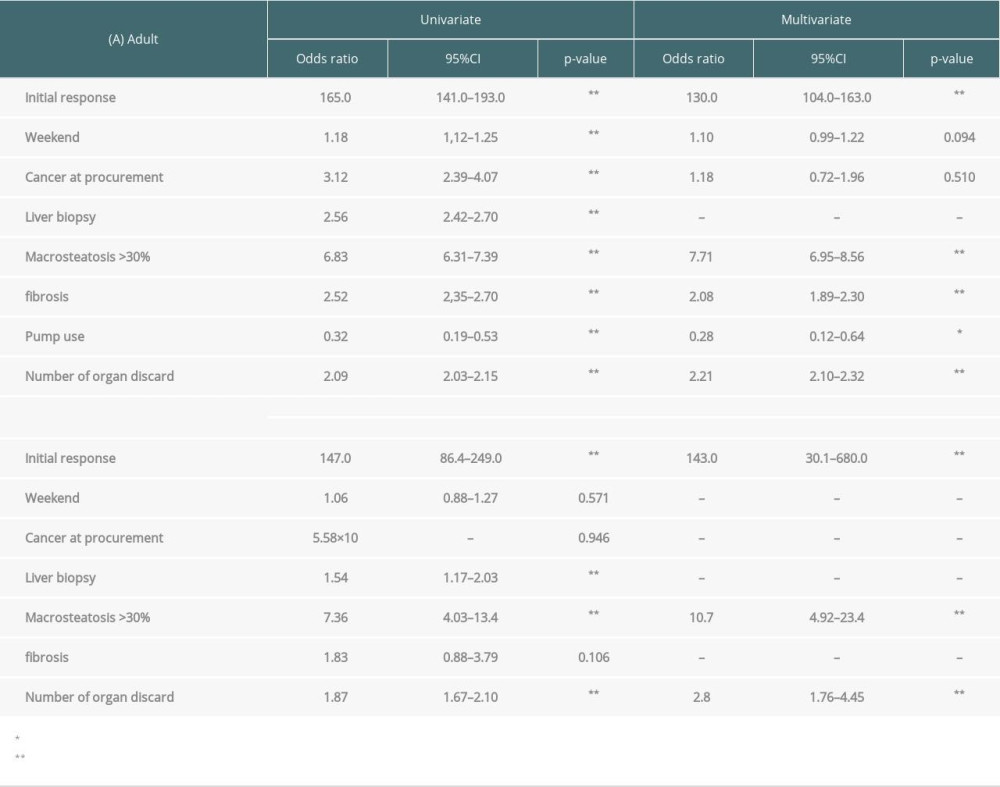 Table 9. Logistic regression for risk factors of declined to the final offers in (A) adult or (B) pediatric deceased livers.
Table 9. Logistic regression for risk factors of declined to the final offers in (A) adult or (B) pediatric deceased livers.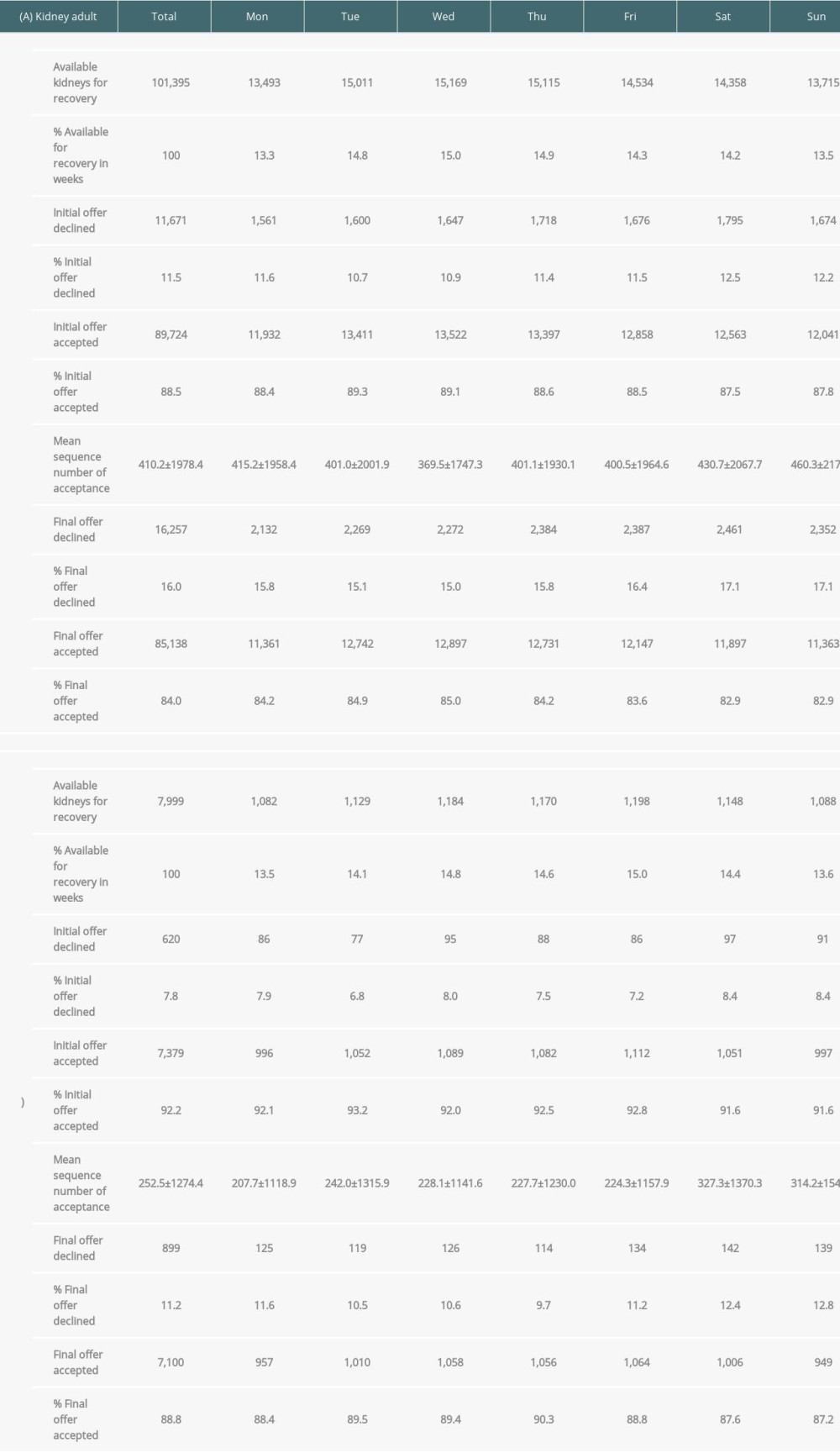 Supplementary Table 1. Total numbers, initial and final offers of potential kidneys from deceased donors by day of week (A. adult donors, B. pediatric donors).
Supplementary Table 1. Total numbers, initial and final offers of potential kidneys from deceased donors by day of week (A. adult donors, B. pediatric donors).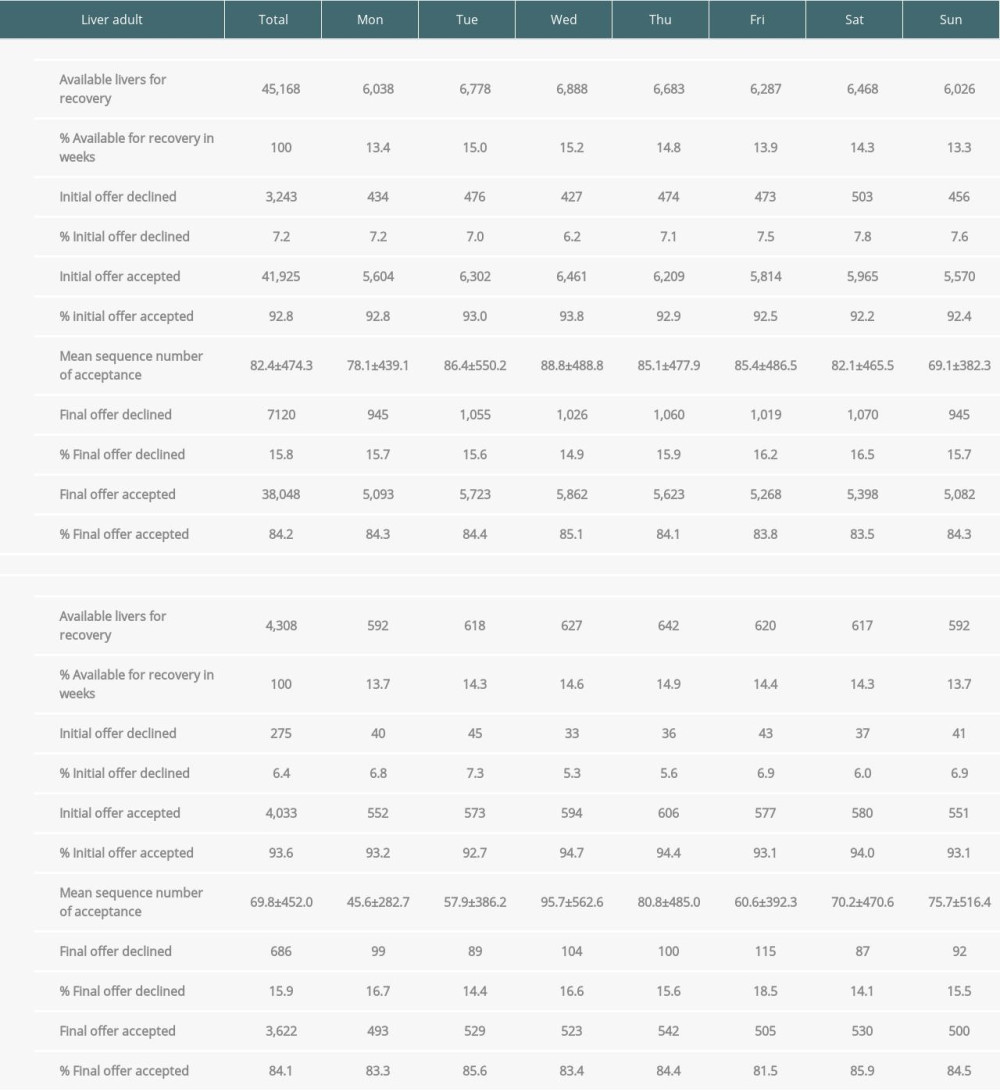 Supplementary Table 2. Total numbers, initial offer and final offers of potential livers from deceased donors by day of week (A. adult donors, B. pediatric donors).
Supplementary Table 2. Total numbers, initial offer and final offers of potential livers from deceased donors by day of week (A. adult donors, B. pediatric donors).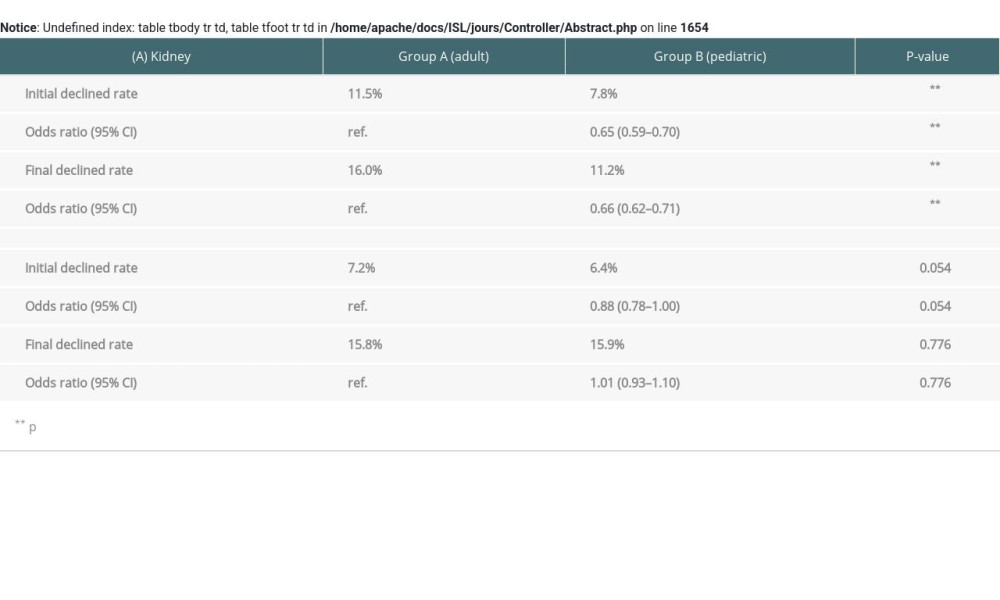 Supplementary Table 3. Adult donors vs pediatric donors of initial and final declined rate (A. Kidney, B. Liver).
Supplementary Table 3. Adult donors vs pediatric donors of initial and final declined rate (A. Kidney, B. Liver). In Press
18 Mar 2024 : Original article
Does Antibiotic Use Increase the Risk of Post-Transplantation Diabetes Mellitus? A Retrospective Study of R...Ann Transplant In Press; DOI: 10.12659/AOT.943282
20 Mar 2024 : Original article
Transplant Nephrectomy: A Comparative Study of Timing and Techniques in a Single InstitutionAnn Transplant In Press; DOI: 10.12659/AOT.942252
28 Mar 2024 : Original article
Association Between FEV₁ Decline Rate and Mortality in Long-Term Follow-Up of a 21-Patient Pilot Clinical T...Ann Transplant In Press; DOI: 10.12659/AOT.942823
02 Apr 2024 : Original article
Liver Transplantation from Brain-Dead Donors with Hepatitis B or C in South Korea: A 2014-2020 Korean Organ...Ann Transplant In Press; DOI: 10.12659/AOT.943588
Most Viewed Current Articles
05 Apr 2022 : Original article
Impact of Statins on Hepatocellular Carcinoma Recurrence After Living-Donor Liver TransplantationDOI :10.12659/AOT.935604
Ann Transplant 2022; 27:e935604
12 Jan 2022 : Original article
Risk Factors for Developing BK Virus-Associated Nephropathy: A Single-Center Retrospective Cohort Study of ...DOI :10.12659/AOT.934738
Ann Transplant 2022; 27:e934738
22 Nov 2022 : Original article
Long-Term Effects of Everolimus-Facilitated Tacrolimus Reduction in Living-Donor Liver Transplant Recipient...DOI :10.12659/AOT.937988
Ann Transplant 2022; 27:e937988
15 Mar 2022 : Case report
Combined Liver, Pancreas-Duodenum, and Kidney Transplantation for Patients with Hepatitis B Cirrhosis, Urem...DOI :10.12659/AOT.935860
Ann Transplant 2022; 27:e935860








